Noridian's Medical Review Team and the Comprehensive Error Rate Testing (CERT) Contractor have identified multiple errors regarding incorrect billing of laboratory services. Laboratory medical records are requested to determine correct billing and coverage under Medicare guidelines. Coverage and Documentation
Full Answer
Are there Entity code errors in medical billing services?
Jan 06, 2022 · They can help assist you in correcting the billing issue. Those with Original Medicare (parts A and B) can call 1-800-MEDICARE with any billing issues. If the error is with a private insurer, they should have a claims issue hotline you can call. If you have any questions regarding Medicare billing, contact your local Social Security Administration office, your private …
What are the most common types of billing errors in healthcare?
Jan 18, 2017 · Under the Qualified Medicare Beneficiaries (QMB) program, medical providers such as doctors, hospitals, and medical supply companies aren’t allowed to bill enrollees for Medicare deductibles, coinsurance, and copayments. If you get a wrongful bill, you don’t have to pay it. You have the right to a refund if you’ve already paid.
What happens if you make a mistake in healthcare billing?
Nov 04, 2019 · Entity’s health insurance claim number (HICN)—This error shows up when a claim has been corrected and resubmitted. In this case, the entity is the payer and the biller needs to ensure that the claim number assigned to the original claim by the payer is used. Entity’s contract/member number—Errors with this reference usually are pointing out missing …
What are the billing responsibilities of a Medicare provider?
Oct 01, 2008 · “This program is going to help us dramatically reduce costly payment errors.” CMS established the MUE program to reduce payment errors for Medicare Part B claims. Claims processing contractors utilize these edits to assure that providers and suppliers do not report excessive services.

How do I correct a Medicare billing error?
Does Medicare allow corrected claims?
Who is responsible for Medicare billing?
What is the name of the entity that processes Medicare claims?
What is the resubmission code for a corrected claim for Medicare?
Can you resubmit a Medicare claim?
Can a provider refuse to bill Medicare?
What is Medicare billing?
Can a Medicare patient be balance billed?
When a third party payer identifies an error on the claim form the claim is?
What organization processes Medicare claims for CMS?
How does CMS-1500 relate to the claims process?
What to do if your provider won't stop billing you?
If the medical provider won’t stop billing you, call Medicare at 1-800-MEDICARE (1-800-633-4227) . TTY users can call (877) 486-2048 . Medicare can confirm that you’re in the QMB Program. Medicare can also ask your provider to stop billing you, and refund any payments you’ve already made. 3.
Can you get a bill for QMB?
If you’re in the QMB Program and get a bill for charges Medicare covers: 1. Tell your provider or the debt collector that you're in the QMB Program and can’t be charged for Medicare deductibles, coinsurance, and copayments.
Is Medicare billed for QMB?
The Centers for Medicare & Medicaid Services (CMS) has heard from people with Medicare who report being billed for covered services, even though they’re in the QMB program.
What are common errors in Medicare bill?
Common errors: There can be things as simple as duplicate charges or incorrect quantities of services, or cancelled items that were not removed from the bill. Default patient medical bills often have vague descriptions of what services were provided, so patients will sometimes ask for an itemized version of the bill with complete medical service codes that can be looked up on the Centers of Medicare & Medicaid Services website.
Why is medical billing important?
Medical billing is an integral part to any practice, but it’s essential to ensure the bills you submit are accurate, especially given its critical role in medical billing. At Med USA, we have decades of experience in medical billing and many other departments that can take the workload off your practice and allow you to focus on what’s important: Giving the best possible medical care to your patients. Visit us today at https://medusarcm.com and let’s talk about how we can work together.
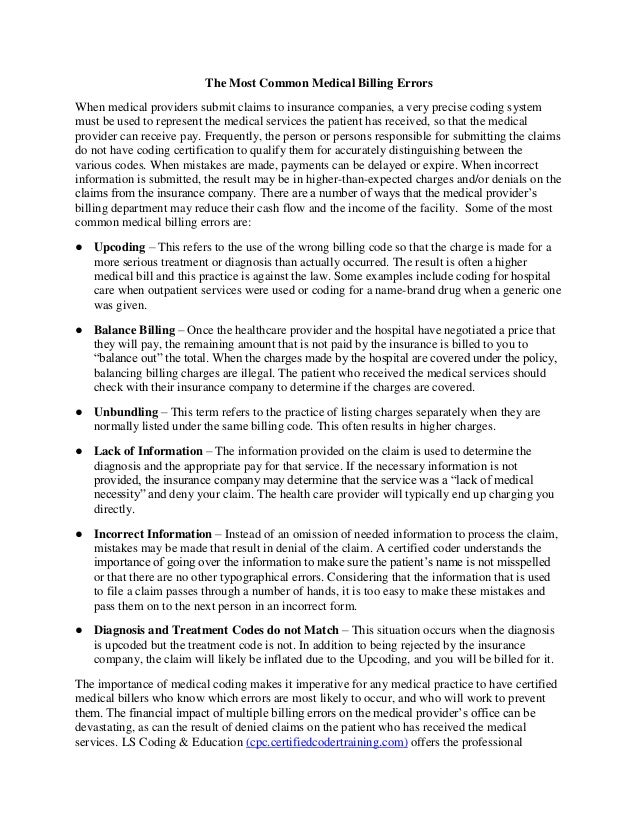
What is upcoding in medical billing?
Upcoding: Upcoding is simply known as charging you for a higher level of care than you actually received , such as a hospital charging for a gurney transport when really what happened is you walked into the ER under your own power. Upcoding is a difficult error to spot for those not trained in medical billing.
What percentage of credit card debt is medical?
The Consumer Financial Protection Bureau once estimated that 52% of all debt listed on credit reports in America is a result of medical bills. And when a consumer has a bad charge on their credit card bill from a medical billing error, that is a black mark on the practice they have visited.
Can you have a wrong birthday on a medical bill?
Sometimes, that isn’t a big deal — think of the number of times that you may have gotten a mailing with your name spelled incorrectly, or a piece of mail was sent to your address by mistake with a different person’s name on it? But with medical billing, there is no such thing as a “ small mistake” with spelling of a person’s name. Those mistakes can have huge consequences when dealing with insurance companies.
Can medical bills be unbundled?
Unbundling: Some medical bill charges are bundled under a single procedural code. One example of this is when you have a deep cut that needs to be cleaned, then have stitches, before the wound is properly dressed. But sometimes those charges are entered separately, and when that happens in some instances it can dramatically increase the bill’s total.
Is anesthesia time on a bill?
Operating room time and anesthesia time: It’s common for bills for surgeries to be according to how long people were in the operating room or under anesthesia. And sometimes that number can be inputted incorrectly on the bill.
How to determine primary payer for Medicare?
The CMS Questionnaire should be used to determine the primary payer of the beneficiary’s claims. This questionnaire consists of six parts and lists questions to ask Medicare beneficiaries. For institutional providers, ask these questions during each inpatient or outpatient admission, with the exception of policies regarding Hospital Reference Lab Services, Recurring Outpatient Services, and Medicare+Choice Organization members. (Further information regarding these policies can be found in Chapter 3 of the MSP Online Manual.) Use this questionnaire as a guide to help identify other payers that may be primary to Medicare. Beginning with Part 1, ask the patient each question in sequence. Comply with all instructions that follow an answer. If the instructions direct you to go to another part, have the patient answer, in sequence, each question under the new part. Note: There may be situations where more than one insurer is primary to Medicare (e.g., Black Lung Program and Group Health Plan). Be sure to identify all possible insurers.
When do hospitals report Medicare Part A retirement?
When a beneficiary cannot recall his/her retirement date, but knows it occurred prior to his/her Medicare entitlement dates, as shown on his/her Medicare card, hospitals report his/her Medicare Part A entitlement date as the date of retirement. If the beneficiary is a dependent under his/her spouse's group health insurance and the spouse retired prior to the beneficiary's Medicare Part A entitlement date, hospitals report the beneficiary's Medicare entitlement date as his/her retirement date. If the beneficiary worked beyond his/her Medicare Part A entitlement date, had coverage under a group health plan during that time, and cannot recall his/her precise date of retirement but the hospital determines it has been at least five years since the beneficiary retired, the hospital enters the retirement date as five years retrospective to the date of admission. (Example: Hospitals report the retirement date as January 4, 1998, if the date of admission is January 4, 2003)
What is secondary payer?
Medicare is the Secondary Payer when Beneficiaries are: 1 Treated for a work-related injury or illness. Medicare may pay conditionally for services received for a work-related illness or injury in cases where payment from the state workers’ compensation (WC) insurance is not expected within 120 days. This conditional payment is subject to recovery by Medicare after a WC settlement has been reached. If WC denies a claim or a portion of a claim, the claim can be filed with Medicare for consideration of payment. 2 Treated for an illness or injury caused by an accident, and liability and/or no-fault insurance will cover the medical expenses as the primary payer. 3 Covered under their own employer’s or a spouse’s employer’s group health plan (GHP). 4 Disabled with coverage under a large group health plan (LGHP). 5 Afflicted with permanent kidney failure (End-Stage Renal Disease) and are within the 30-month coordination period. See ESRD link in the Related Links section below for more information. Note: For more information on when Medicare is the Secondary Payer, click the Medicare Secondary Payer link in the Related Links section below.
Why did CMS develop an operational policy?
CMS developed an operational policy to help alleviate a major concern that hospitals have had regarding completion of the CMS Questionnaire.
Does Medicare pay for black lung?
Federal Black Lung Benefits - Medicare does not pay for services covered under the Federal Black Lung Program. However, if a Medicare-eligible patient has an illness or injury not related to black lung, the patient may submit a claim to Medicare. For further information, contact the Federal Black Lung Program at 1-800-638-7072.
Does Medicare pay for the same services as the VA?
Veteran’s Administration (VA) Benefits - Medicare does not pay for the same services covered by VA benefits.
Does no fault insurance cover medical expenses?
Treated for an illness or injury caused by an accident, and liability and/or no-fault insurance will cover the medical expenses as the primary payer.
How much money do doctors lose due to medical billing errors?
Although these errors are fairly common, they can be expensive. According to Healthcare Business and Technology, doctors lose $125 billion each year because of poor medical billing systems and errors. Most errors can be avoided if the medical coder or biller takes a few simple steps:
Why are medical billers important?
Medical billers and coders are crucial to the healthcare industry. They keep doctors and nurses on track and organized by carefully documenting patient procedures and treatments. In addition, they submit bills to insurance companies, which then pay claims. When a medical biller or coder makes a mistake, it can delay the claims process, ...
How often do you need to update your CPT code?
Stay current and on top of code changes. ICD-10 and CPT code manuals are updated annually. Also, if you’re a member of American Academy of Professional Coders (AAPC) or American Health Information Management Association (AHIMA), you are required to complete education credits every two years to help you remain current.
What is the ICD-10 code?
The World Health Organization created the International Classification of Diseases, Tenth Revision (ICD-10), which universally classifies and codes all diagnoses, symptoms and medical procedures.
Why is a claim denied?
In another scenario, a claim may be denied if the payer determines the procedure or charge is not payable. Perhaps it violates the payer-patient contract (i.e., using an out-of-network provider) or is a high-tier prescription that is not covered.
Why are medical records and health information technicians growing?
According to the Bureau of Labor Statistics, the employment rate for medical records and health information technicians (billers and coders) is growing much faster than the average for other occupations because people in these jobs are the ones who handle insurance and patient claims.
What happens if a claim is denied?
If a claim request has been submitted incorrectly, resulting in errors found before it is processed, the insurance company will reject the claim and not pay the bill as written. It’s then sent back with an explanation, and the process begins again.
Tuesday, December 11, 2012
This Claim is rejected for Invalid Information for a Rendering Provider's National Provider Identifier (NPI). (A7:562:82)
Medicare top ten errors
This Claim is rejected for Invalid Information for a Rendering Provider's National Provider Identifier (NPI). (A7:562:82)
What is EDI in Medicare?
EDI is the automated transfer of data in a specific format following specific data content rules between a health care provider and Medicare, or between Medicare and another health care plan. In some cases, that transfer may take place with the assistance of a clearinghouse or billing service that represents a provider of health care or another payer. EDI transactions are transferred via computer either to or from Medicare. Through use of EDI, both Medicare and health care providers can process transactions faster and at a lower cost.
What is the ASCA requirement for Medicare?
The Administrative Simplification Compliance Act (ASCA) requirement that claims be sent to Medicare electronically as a condition for payment; How you can obtain access to Medicare systems to submit or receive claim or beneficiary eligibility data electronically; and. EDI support furnished by Medicare contractors.