Does Medicaid cover physical therapy?
The physical therapy, cognitive-behavioral therapy, chiropractic therapy, and acupuncture services will now be offered at no charge to Medicaid patients. If you are enrolled in MoHealthNet, these new, complementary treatments will be available.
How much does Medicare Part B pay for physical therapy?
Medicare can help pay for physical therapy (PT) that’s considered medically necessary. After meeting your Part B deductible, which is $198 for 2020, Medicare will pay 80 percent of your PT costs. PT can be an important part of treatment or recovery for a variety of conditions.
Is PT covered by Medicare?
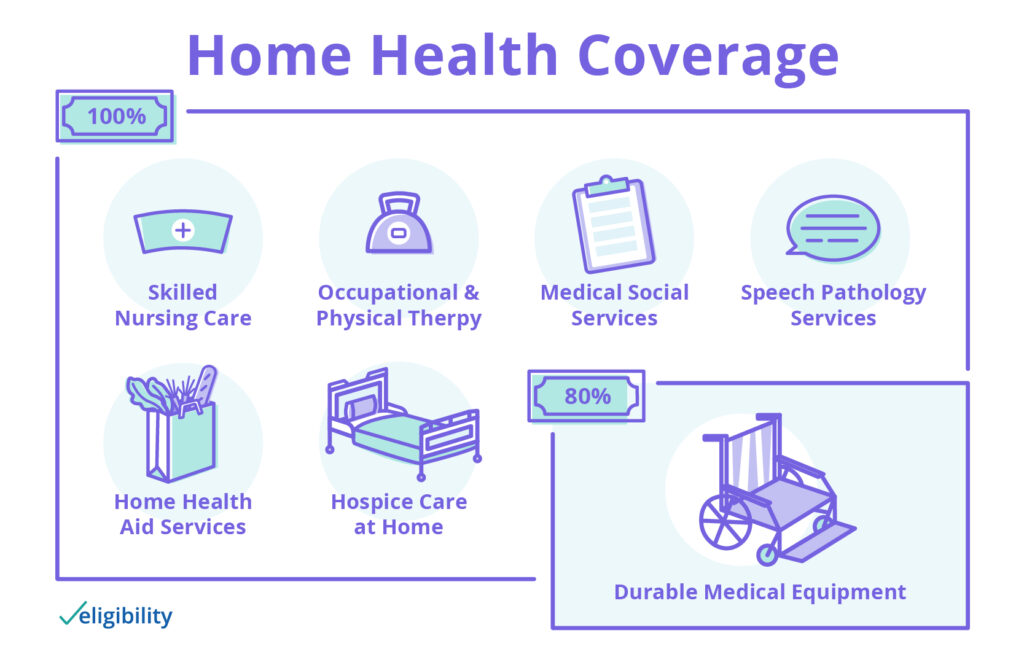
Medicare-certified hospice care is usually given in your home or other facility where you live, like a nursing home. Original Medicare will still pay for covered benefits for any health problems that aren't part of your terminal illness and related conditions, but hospice should cover most of your care.
What does basic Medicare cover?
Medicare covers up to 100 days of part-time daily care or intermittent care if medically necessary. You must have spent at least three consecutive days as a hospital inpatient within 14 days of receiving home health care. If you don’t qualify for home health care coverage under Part A, you might have Medicare coverage under Part B.
How many PT sessions will Medicare pay for?
Medicare Coverage The good news is there's no limit on the number of physical therapy treatments within one calendar year as long as your physician or physical therapist can certify that treatment is medically necessary.
What is the Medicare deductible for physical therapy?
Outpatient Physical Therapy Costs Medicare beneficiaries should expect to pay 20% of the Medicare-approved amount with Medicare covering 80% of that amount. In order for an individual to have Part B coverage, they must pay the Part B monthly deductible. In 2022, the Medicare Part B deductible is $233 per month.
Does Medicare contribute to physical therapy for elderly?
Medicare does cover physical therapy for members. Original Medicare Part A covers inpatient rehabilitation care, including physical therapy. Outpatient physical therapy patients can get coverage under Original Medicare Part B. Seniors can also receive physical therapy coverage under Medicare Advantage plans.
Will Medicare pay for physical therapy at home?
Medicare Part B medical insurance will cover at home physical therapy from certain providers including private practice therapists and certain home health care providers. If you qualify, your costs are $0 for home health physical therapy services.
Does Medicare cover outpatient physical therapy?
Yes. Physiotherapy can be covered by Medicare so long as it's a chronic and complex musculoskeletal condition requiring specific treatment under the CDM.
How much is physical therapy without insurance?
$75 – $150 (Without Insurance) Physical therapy costs from $20 to $150 per session on average depending on the extent of your injury and if you have insurance coverage. With insurance, rates range from a $20 to $55 co-pay after you've paid your deductible, and between $75 to $150 if you're paying without insurance.
Does Medicare cover physical therapy for arthritis?
Medicare Part B Medicare will usually cover doctor's visits related to arthritis, physical therapy, and some DME, such as splints, braces, walkers, or canes. A person is often required to obtain prior authorization from Medicare before purchasing equipment or pursuing therapy services.
What is the Medicare deductible for 2022?
$233The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.
Does Medicare cover physical therapy for osteoporosis?
Medicare Part B generally covers physical therapy services. If you get physical therapy at the hospital, an outpatient center, or in your doctor's office, Part B typically covers 80% of allowable charges after you meet your Part B deductible.
Does Medicare pay for home caregivers?
Medicare typically doesn't pay for in-home caregivers for personal care or housekeeping if that's the only care you need. Medicare may pay for short-term caregivers if you also need medical care to recover from surgery, an illness, or an injury.
Does Medicare cover physical therapy after hip replacement?
Medicare Part B generally covers most of these outpatient medical costs. Medicare Part B may also cover outpatient physical therapy that you receive while you are recovering from a hip replacement. Medicare Part B also generally covers second opinions for surgery such as hip replacements.
Does Medicare cover rehab after surgery?
Medicare Part A covers medically necessary inpatient rehab (rehabilitation) care, which can help when you're recovering from serious injuries, surgery or an illness. Inpatient rehab care may be provided in of the following facilities: A skilled nursing facility.
Why is Physical Therapy Valuable?
According to the American Physical Therapy Association (APTA), physical therapy can help you regain or maintain your ability to move and function after injury or illness. Physical therapy can also help you manage your pain or overcome a disability.
Does Medicare Cover Physical Therapy?
Medicare covers physical therapy as a skilled service. Whether you receive physical therapy (PT) at home, in a facility or hospital, or a therapist’s office, the following conditions must be met:
What Parts of Medicare Cover Physical Therapy?
Part A (hospital insurance) covers physical therapy as an inpatient service in a hospital or skilled nursing facility (SNF) if it’s a Medicare-covered stay, or as part of your home health care benefit.
Does Medicare Cover In-home Physical Therapy?
Medicare Part A covers in-home physical therapy as a home health benefit under the following conditions:
What Are the Medicare Caps for Physical Therapy Coverage?
Medicare no longer caps medically necessary physical therapy coverage. For outpatient therapy in 2021, if you exceed $2,150 with physical therapy and speech-language pathology services combined, your therapy provider must add a modifier to their billing to show Medicare that you continue to need and benefit from therapy.
How does physical therapy help with Medicare?
Physical therapy can help restore normal physical functioning and reduce and eliminate various limitations or disabilities caused by disease, injury, or a chronic health condition. Physical therapy can help you maintain your independence and your ability to perform activities of daily living. If you qualify for Medicare due to age ...
What is physical therapy?
Physical therapy focuses on restoring and increasing joint mobility, muscle strength, and overall functionality. All of these factors play key roles in improving quality of life and affecting the activities and hobbies you are able to participate in.
Does Medicare cover physical therapy?
Medicare does offer coverage for all physical therapy treatments that are prescribed by a physician and deemed medically necessary to improve your specific health condition. In most cases, your therapy treatments are covered by Medicare Part B. Part B is responsible for covering medically necessary outpatient procedures and services.
Does Medicare cover home health care?
If you are homebound and require physical therapy treatments to occur in your own home, you may receive coverage through your Medicare benefits for home health care. Specific requirements must be met to receive home health care, including being homebound and needing skilled nursing services intermittently.
How much does physical therapy cost on Medicare?
Although Medicare does not have a spending limit on physical therapy sessions, once the cost reaches $2,080, a person’s healthcare provider will need to indicate that their care is medically necessary.
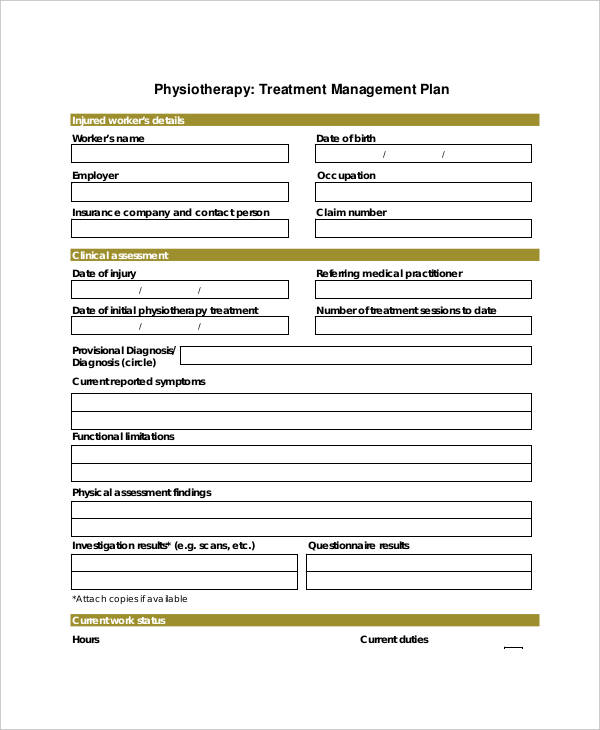
What is the process of creating a physical therapy plan?
The process of creating and maintaining a physical therapy plan may include the following steps: A physical therapist evaluates the person who needs physical therapy and creates a plan of care. This plan includes a recommended number of sessions, treatment types, and treatment goals.
What happens after a physical therapist completes a physical therapy visit?
At this time, the therapist may release the individual from further physical therapy. Alternatively, the referring doctor may recommend participating in additional sessions.
What is an example of a woman with Medicare?
Here is an example: A woman with Medicare was in a car accident and injured her knee. Her doctor recommended physical therapy to improve her strength and range of motion. She participated in the recommended physical therapy sessions and made improvements in strength but had not fully reached her goals for mobility.
Does Medicare consider progress in physical therapy?
Treatment progress is not the only consideration when Medicare evaluates continued funding for an individual’s physical therapy. For example, Medicare requires a physical therapist to recertify that physical therapy is medically necessary after the total costs for therapy exceed $2,080.
How much does Medicare pay for outpatient therapy?
For outpatient therapy, you pay 20 percent of the Medicare-approved amount for the service. The Part B deductible applies; Medicare will pay its share once you’ve met your deductible for the year. Unlike with Part A, prior hospitalization is not a prerequisite for Part B to cover physical therapy.
How to contact Medicare for therapy?
If you have questions about coverage and costs for therapeutic services, call 1-800-MEDICARE (800-633-4227) or contact your State Health Insurance Assistance Program. Return to Medicare Q&A main page.
When did Medicare stop paying for therapeutic services?
Medicare used to set an annual maximum for what it would pay for outpatient therapeutic services, but the cap was eliminated in 2018. This government health insurance program no longer limits what it will pay in a given year for a beneficiary to receive medically necessary therapeutic services.
Does Medicare cover physical therapy?
Medicare Part A, which includes hospital insurance, or Part B, which covers outpatient treatment, might cover this service depending on the circumstances and the setting. The same holds true for occupational and speech therapy. Medicare Part A pays some or all of the cost of physical therapy you receive at an inpatient rehabilitation facility.
What is the best physical therapy for seniors?
Some of the physical therapy methods used to treat seniors include: Physical manipulation such as stretching, walking and range of motion exercises. Ultrasounds to promote blood flow and the heating of muscles, tendons and tissues.
Why do seniors need physical therapy?
There are several reasons why a senior citizen might undergo physical therapy, such as: Recovering from a fall, accident or stroke. Falls are the most common type of accident for seniors, and they often result in broken bones and other injuries.
What is the Medicare Part B deductible?
Medicare Part B provides coverage for occupational therapy on an outpatient basis . The Part B deductible applies, and you will owe up to 20% of the Medicare-approved amount after you meet your annual Part B deductible.
How does physical therapy help with pain?
Physical therapy can be an effective form of pain relief for chronic pain conditions such as arthritis and osteoporosis. Reducing dependence on prescription medications. Finding pain relief through physical therapy can reduce or eliminate one’s dependency on pain killing medication.
What type of therapy is best for seniors?
Common types of physical therapy for seniors. Because there are so many different reasons for going through physical therapy, there are several different types of therapy that can match each unique need. Depending on your situation, your doctor may recommend one of the following types of physical therapy. Orthopedic physical therapy targets ...
What is pelvic floor rehabilitation?
Pelvic floor rehabilitation aims to treat complications in the digestive system along with pelvic pain resulting from injuries, surgery or other conditions. As there are different types of physical therapy, there are also a number of different methods that may be used to deliver therapeutic treatment.
Do you need to add a notation to a physical therapy claim?
Your therapy provider may need to add a notation to your therapy claim, confirming that your therapy services are reasonable and necessary. Your therapist may also add information to your medical records explaining why the services are medically necessary. If your physical therapy services are not medically necessary, ...
Why do doctors order physical therapy after surgery?
Doctors sometimes order physical therapy after surgery to help you recover and regain your mobility, but might order these services in other situations where physical therapy services might improve your ability to function.
What is Medicare Part B?
Medicare Part B helps pay for medically necessary services, generally up to a certain limit or cap as described below. Find affordable Medicare plans in your area. Find Plans. Find Medicare plans in your area. Find Plans. Physical therapy involves examination, evaluation, and treatment to improve your ability to move or restore certain aspects ...
Does Medicare Supplement pay for out of pocket costs?
You may have the option of signing up for a Medicare Supplement (Medigap) plan to help pay for Original Medicare’s out-of-pocket costs. Different Medigap plans pay for different amounts of those costs, such as copayments, coinsurance, and deductibles.
Does Medicare cover physical therapy?
If your Medicare-assigned doctor decides that physical therapy is medically necessary outside of home health care, Medicare Part B will cover 80 percent of the Medicare- approved costs of outpatient physical therapy, occupational therapy, and speech-language pathology, until the limits are reached. The Medicare Part B deductible also applies.
Physical Therapy and Medicare Coverage
Medicare Part A can cover some of the cost of physical therapy at either an inpatient facility or your home. The longevity of the treatment as well as your deductibles and other payments are taken into consideration when calculating the overall costs for physical therapy coverage.
Medicare and the Costs of Physical Therapy
The costs of physical therapy vary depending on your Medicare coverage, but it can range between $75 to $350 per session (out of pocket). Fortunately, there are many ways to ease the financial burden if you qualify for coverage through Medicare.
Bottom Line
Medicare coverage for physical therapy largely depends on the specific plan and services you’re enrolled in. For the most part, Medicare can cover part or the full cost of physical therapy, depending on what your physician or physical therapist deems as medically necessary.
What is the goal of physical therapy?
The goal for most physical therapy treatment plans is to not only improve a person’s condition, but to help them prevent injuries from occurring or the pain associated with an existing injury from worsening. Neurological conditions that impact how the body moves can also require the support of a physical therapist.
What conditions can a physical therapist help with?
Neurological conditions that impact how the body moves can also require the support of a physical therapist. Other chronic conditions, such as arthritis or diabetes, can lead to secondary mobility or pain management issues that benefit from physical therapy techniques.
How does Medicare Supplement and Medicare Advantage work?
Both Medicare Supplement and Medicare Advantage plans work to expand or enhance the benefits Original Medicare recipients enjoy. They are also both offered through private insurers who are contracted by Medicare to offer some or several plan options.
What is Medicare Supplement?
Medicare Supplement, or Medigap, policies are sold by private insurance companies to help lower these out-of-pocket costs. Medicare recipients can choose to enhance their existing Original Medicare benefits with Medicare Supplement plans, like Plan N.
Does Medicare Supplement Plan have Part A and Part B?
Unlike a Medicare Advantage plan, a Medicare Supplement plan does not bundle Part A and Part B benefits into its own plan. A Medicare Supplement plan stands alone from Original Medicare Part A and Part B, but a recipient must have both Original Medicare coverage in order to enroll in a Medicare Supplement plan.