2017 Medicare Saving Programs Eligibility Limits
| MSP Program Type | Single Income | Married Income |
| Qualified Medicare Beneficiary (QMB) | $1,025 | $1,374 |
| Specified Low-Income Medicare Beneficiar ... | $1,226 | $1,644 |
| Qualifying Individual (QI) | $1,377 | $1,847 |
Where can I get help Paying my Medicare premiums?
Medicare Savings Programs. You can get help from your state paying your Medicare premiums. In some cases, Medicare Savings Programs may also pay Medicare Part A (Hospital Insurance) and Medicare Part B (Medical Insurance) deductibles, coinsurance, and copayments if you meet certain conditions.
What are the different Medicare Part A and Part B programs?
There are currently four programs that fall under the MSP umbrella: Qualified Medicare Beneficiary (QMB) Program for Part A and/or Part B premiums. Specified Low-Income Medicare Beneficiary (SLMB) Program for Part B premiums. Qualifying Individual (QI) Program for Part B premiums.
What is a Medicare Savings Program (MSP)?
For Medicare recipients under a certain income and asset level, Medicare benefits can be cost prohibitive. A Medicare Savings Program (MSP) is designed to cover all or part of Medicare out-of-pocket expenses that encumber Medicare recipients who live within limited financial means.
How do Medicare savings programs pay for care?
In some cases, Medicare Savings Programs may also pay Part A covers inpatient hospital stays, skilled nursing facility care, hospice care, and some home health care. Part B covers certain doctors’ services, outpatient care, medical supplies, and preventive services. deductibles, coinsurance, and copayments if you meet certain conditions.

What is Medicare Beneficiary program?
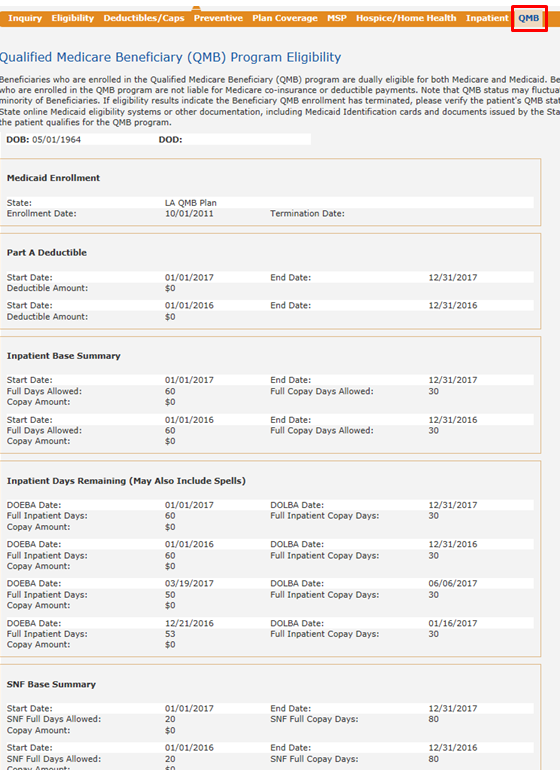
The Qualified Medicare Beneficiary (QMB) program provides Medicare coverage of Part A and Part B premiums and cost sharing to low-income Medicare beneficiaries. In 2017, 7.7 million people (more than one out of eight people with Medicare) were in the QMB program.
What is QMB stand for?
State of California—Health and Human Services Agency. QUALIFIED MEDICARE BENEFICIARY (QMB), SPECIFIED LOW-INCOME MEDICARE BENEFICIARY (SLMB), AND QUALIFYING INDIVIDUALS (QI) APPLICATION.
Which program helps individuals who receive Social Security and Medicare?
What is Social Security Medicare Savings Program? Medicare Savings Programs (MSP) are federally funded programs administered by each individual state. These programs are for people with limited income and resources to help pay some or all of their Medicare premiums, deductibles, copayments, and coinsurance.
What is the Medicare savings program in Arizona?
Medicare beneficiaries in Arizona can qualify for a Medicare Savings Program (MSP) with incomes up to $1,416 a month if single and $1,920 a month if married. In Arizona, applicants can qualify for Medicaid for the aged, blind and disabled with monthly incomes up to $1,064 (single) and $1,437 (married).
Is QMB the same as Medicare?
The Qualified Medicare Beneficiary (QMB) Program is one of the four Medicare Savings Programs that allows you to get help from your state to pay your Medicare premiums. This Program helps pay for Part A premiums, Part B premiums, and deductibles, coinsurance, and copayments.
Does SLMB pay deductible?
Unlike the Qualified Medicare Beneficiary (QMB) program, SLMB does not pay for Parts A and B cost sharing (e.g. deductibles, co-pays and coinsurance) or for Part A premiums (if an enrollee owes them).
Which program helps individuals whose assets are not low enough to qualify them for Medicaid by requiring states to pay their Medicare Part A and B?
Medicare Supplementary Insurance (MSI) is designed to supplement Medicare benefits by: paying for services that Medicare does not cover.
Which program helps individuals whose assets are not low enough to qualify them for Medicaid by requiring states to pay their Medicare Part A and B premiums?
Health Insurance Chapter 14, 15QuestionAnswerThis helps individuals whose assets are not low enough to qualify them for medicaid by requiring states to pay their medicare part A and B premiums, deductibles, and coinsurance amountsqualified medicare beneficiary program (QMBP)39 more rows
Which of the following is used by the federal government to provide Social Security and Medicare benefits quizlet?
* FICA TAXES: Part A of Medicare and all the benefits of the Social Security program are financed through a system of payroll and self-employment taxes paid by all persons covered under the programs.
What is Ahcccs SLMB?
AHCCCS SLMB-PART B BUY-IN (Health Program ID #008040) AHCCCS SLMB-PART B BUY-IN is strictly a Medicare Savings Program that pays Medicare Part B premium. No claim payments are done by AHCCCS Administration. For questions regarding Medicare coverage, call 1-800-MEDICARE.
Does Arizona have a Medicaid program?
The Arizona Health Care Cost Containment System (AHCCCS) is Arizona's Medicaid agency, and Medicaid within the state is often referred to as “AHCCCS.” Although the agency provides the medical insurance coverage, DES determines the eligibility for Medicaid.
Is Ahcccs Medicare?
AHCCCS is Arizona's State Medicaid Program. AHCCCS Members who also have Medicare are called Dual Eligible Members. Being enrolled in the same health plan for Medicare and Medicaid is called “alignment.”
What is Medicare Savings Program?
A Medicare Savings Program (MSP) is designed to cover all or part of Medicare out-of-pocket expenses that encumber Medicare recipients who live within limited financial means.
What is a Medicare summary notice?
You will also receive a Medicare Summary Notice (MSN), which is proof of being in the program and shows the healthcare provider you should not be billed for services, deductibles, coinsurance or copayments. An exception is outpatient prescriptions.
What is QDWI in Medicare?
Qualified Disabled and Working Individuals (QDWI) Program for Part A premiums. If your application for the QMB Program is accepted, you will receive a QMB card. Be sure to show this card along with your Medicare or Medicaid card every time you receive healthcare services. You will also receive a Medicare Summary Notice (MSN), ...
Is Medicare cost prohibitive?
The cost of Medicare benefits in the form of premiums, coinsurance, copayments and deductibles can raise concerns about affordability, especially when you are on a limited income. For Medicare recipients under a certain income and asset level, Medicare benefits can be cost prohibitive.
How long does it take for Medicare to cover seniors?
Coverage in Medicare Savings Programs typically begins one month after a senior has been approved for Medicare. Application processing varies by state but is typically less than 60 days.
What is a QMB in Medicare?
Eligibility for each is primarily based on a senior’s financial resources and income. 1) Qualified Medicare Beneficiary (QMB) – helps pay for Medicare Part A & Part B, as well as deductibles, copayments, and coinsurance. 2) Specified Low-Income Medicare Beneficiary (SLMB) – helps pay for Medicare Part B only.
How old do you have to be to qualify for Medicare?
Seniors must be eligible for Medicare and therefore Medicare Saving Program’s eligibility begins at the same age of 65 years old.
How many states have elder care programs?
Did You Know? All 50 states have programs that help low income seniors in need of eldercare. Many states have multiple programs. Search for assistance in your state.
Does Medicare pay for adult day care?
Medicare hospice care is the one notable exception to this rule. Adult Day Care. Medicare does not pay for adult day care services.
Does Medicare cover assisted living?
The care must be for short term recovery following a hospital stay. Medicare does not cover any cost of assisted living.
Does Medicare provide cash payments to seniors?
Medicare Savings Programs provide reductions in Medicare premiums, deductibles and co-payments for the elderly. This program does not provide seniors with cash payments.
The MSP consist of: QMB, SLMB, and ALMB PROGRAMS
The QMB, SLMB, and ALMB help eligible Medicare beneficiaries pay all or some of Medicare’s cost sharing amounts (i.e. premiums, deductibles and co-payments). Individuals must re-apply every year for each program.
ALMB (Additional Low-Income Beneficiary Program)
Congress only appropriated a limited amount of funds to each state to pay for this program. Once a state’s appropriated money is gone, even eligible individuals will not be able to get into the program.
Do these programs help with prescription drug coverage?
Enrollment in any of the above three programs, automatically grants the beneficiary enrollment in the Low Income Subsidy ‘Extra Help’ under Medicare Part D. This is very beneficial because:
MSP Frequently Asked Questions
MSP is administered by the State Department of Social Services (DSS). Applications can be found on the DSS website or contact Choices.
What Is the Income Limit for the Medicare Savings Program?
These limits get adjusted each year. For 2021, the Medicare Savings Program income and resource limit s are:
How Much Money Can You Have in the Bank on Medicare?
Money in bank accounts is considered a resource when determining whether you’re eligible for a Medicare Savings Plan. This amount changes depending on which Medicare Savings Program you qualify for. Just like with income limits, your state may accept your application if your resources are higher than the limits allowed. To see if you are eligible, contact your local SHIP.
What are Medicare Savings Programs?
These are Medicaid-administered benefits that help cover Medicare premiums and out-of-pocket costs, such as deductibles and coinsurance . Who qualifies for Medicare Savings Programs? MSPs are available for Medicare beneficiaries with limited incomes and resources who do not qualify to be fully enrolled in Medicaid. Participants must meet certain income and resource levels and have Medicare Part A to qualify. If requirements are met, Medicare and state Medicaid programs work together to provide assistance through Medicare Savings Programs.
What is Extra Help from Medicare?
Extra Help is a federal program that helps people with limited income and resources pay for their Part D premiums and drug costs. What exactly does Extra Help with Medicare cover? Most people who qualify will pay:
