Clinical social workers (CSWs) are the largest group of mental health service providers in the United States and are among the professions that can bill Medicare Part B for mental health services.1 They have a graduate degree (master’s or doctorate) in social work, two years of postgraduate supervised experience in a clinical setting, and a clinical license in their state or jurisdiction of practice.
Full Answer
How to find a mental health counselor who accepts Medicare?
Mental health care (outpatient)
- One depression screening per year. ...
- Individual and group psychotherapy with doctors or certain other licensed professionals allowed by the state where you get the services.
- Family counseling, if the main purpose is to help with your treatment.
- Testing to find out if you’re getting the services you need and if your current treatment is helping you.
How to choose your mental health care provider?
To find a mental health provider, you have several options:
- Ask your health insurance company for a list of covered providers. ...
- Seek a referral or recommendation from your primary care provider.
- Ask trusted friends, family or clergy.
- Check to see whether your company's employee assistance program (EAP) or student health center offers mental health services, or ask for a referral.
Does Medicaid improve mental health?
While these programs do not focus exclusively on mental health, Medicaid is the single largest funder of mental health services in the country, which makes this support especially valuable. The federal government also provides Mental Health Block Grants (MHBG) that support states in building out their community mental health services.
Does Medicaid offer mental health services?
If you have Medicaid, know that you have access to an array of mental health services you need for yourself and your children. In fact, Medicaid is the largest national single-payer for mental health services in the United States, so rest assured. After all, many others who use Medicaid have found mental health services that are covered, which means you can too; it’s all about knowing where to look.
Can a therapist bill Medicare?
Medicare has covered psychiatrists, psychologists and clinical social workers since 1989, but does not cover Licensed Professional Counselors (LPC's).
Who can Bill 90887?
Description: CPT code 90887 is used when the treatment of the patient may require explanations to the family, employers or other involved persons for their support in the therapy process. This may include reporting of examinations, procedures, and other accumulated data.
Who can bill G2214?
Primary care practices that are providing collaborative care services can bill for those services using CPT® codes for Psychiatric collaborative care management services (99492, 99493, 99494 and G2214).
Who can Bill 90833?
Able to be utilized by psychiatrists, nurse practitioners, physicians, and physician assistants (or those who can prescribe medication), Code 90833 allows prescribers to take 16-37 minutes to talk to their patients about their mental health issues themselves.
Can a psychologist Bill 99358?
Their answer is yes, with several caveats. And, a few reminders: Beginning in 2021, 99358 may not be reported on the same day as an office visit code 99202—99215. These codes are for the work of a physician or qualified health care professional who has E/M in their scope of practice, not clinical staff.
Who can Bill 90847?
To bill 90846 or 90847, you must choose one person in the family as the identified patient (ideally the primary holder of the insurance or the one with the more severe symptoms).
Who can bill for CPT code 99484?
The BHI codes (99492, 99493,99494, and 99484) can be billed (directly reported) by physicians and non- physician practitioners whose scope of practice includes evaluation & management (E/M) services and who have a statutory benefit for independently reporting services to Medicare.
Can CCM and BHI be billed in the same month?
The BHI codes can be billed for the same patient in the same month as CCM if advance consent for both services and all other requirements to report BHI and to report CCM are met and time and effort are not counted more than once.
What is the difference between 99446 and 99451?
Codes 99446, 99447, 99448, 99449 conclude with a verbal opinion report and written report from the consultant to the treating/requesting physician or other QHP. Code 99451 concludes with only a written report.
Who can bill for 96112?
CPT 96112, developmental test administration (including assessment of fine and/or gross motor, language, cognitive level, social, memory and/or executive functions by standardized developmental instruments when performed), by physician or other qualified health care professional, with interpretation and report; first ...
Can a physician assistant Bill for 90833?
MDs, DOs, qualified Clinical Nurse Specialists, Nurse Practitioners and Physician Assistants are the only providers that may render psychotherapy codes that include an E/M component (CPT codes 90833, 90836, 90838).
Who can Bill 90837?
CPT code 90837 doesn't have to be billed by a licensed medical doctor. It's mainly used by licensed mental health professionals. Typically, Licensed Clinical Social Workers, Licensed Professional Clinical Counselors, Licensed Marriage and Family Therapists, and Clinical Psychologists will bill CPT code 90837.
Which is the largest payer for mental health services in the United States?
Medicaid is the single largest payer for mental health services in the United States and is increasingly playing a larger role in the reimbursement of substance use disorder services.
What is the Mental Health Parity and Addiction Equity Act?
The most recent law, the Mental Health Parity and Addiction Equity Act (MHPAEA), impacts the millions of Medicaid beneficiaries participating in Managed Care Organizations, State alternative benefit plans (as described in Section 1937 of the Social Security Act) and the Children’s Health Insurance Program.
What is the MHPAEA?
Effective benefit design for substance use disorder services. Mental Health Parity and Addiction Equity Act (MHPAEA) application to Medicaid programs.
What is the Medicare Part B coverage for a clinical psychologist?
Clinical psychologists diagnose and treat mental, emotional, and behavioral disorders – and are one of the health care providers covered by Medicare Part B. Coverage: Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the Medicare-approved amount, the Part B deductible, and coinsurance costs.
What is Medicare Part B?
Coverage: Medicare Part B helps pay for a psychiatric evaluation. Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the approved amount, the Part B deductible, and coinsurance costs.
What percentage of Medicare does a nurse practitioner pay?
Nurse practitioners. Physician assistants. Coverage: Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the Medicare-approved amount, the Part B deductible, and coinsurance costs.
Does Medicare cover marriage counseling?
Medicare does not cover other types of relationship counseling, such as marriage counseling. You’re only covered for mental health services from a licensed psychiatrist, clinical psychologist, or other health care professional who accepts Medicare assignment.
Does Medicare cover depression screening?
Coverage: A yearly depression screening and preventive visit does not cost anything if your doctor or health care provider accepts assignment.
Does Medicare cover mental health?
Medicare Coverage of Mental Health Services. A person’s mental health refers to their state of psychological, emotional, and social well-being – and it’s important to take care of it at every stage of life , from childhood to late adulthood. Fortunately, Medicare beneficiaries struggling with mental health conditions may be covered ...
What is mental health billing?
Working with a mental health billing company can help behavioral health practices improve their collection rates, often allowing practices to collect 96 percent or more of money owed to them. Psychiatric Billing Associates is a national mental health billing service that focuses on assisting psychiatrists, psychologists, social workers and therapists. In business since 1994, Psychiatric Billing has an excellent track record of providing services such as: 1 Insurance claims processing 2 Payment posting 3 Client billing and communications 4 Unpaid claims follow-up 5 Verification of Benefits
What is billed for mental health?
In the mental health field, patients and insurers are billed primarily for therapy, medical management and psychological testing services. Insurers have rules about how long a session they’ll pay for, how many they’ll pay for per day or week, and often a maximum number of treatments that they will pay for. The mental health needs of the patient may ...
How long does it take for a mental health insurance claim to be processed?
In most cases, it will take at least 30 days from the date the insurer receives a claim to when your mental health practice will receive reimbursement. Some insurers move faster, with turnaround times of two to three weeks, but, as a rule, 30 days is what most practices can expect. Can clients be billed for the balance after insurance reimbursement?
How can mental health professionals stay informed?
By contacting insurers and making sure that clients’ coverage is still in effect and has not changed , mental health professionals can stay informed and avoid wasting time on rejected claims. This can be labor intensive, but the time it will save makes it worthwhile.
Why do people become mental health professionals?
People become mental health professionals because they want to help others. However, providers cannot help others unless they collect sufficient funds to run their practices, and pay themselves.
Why is it important to have a biller who makes sure that the claims are filed correctly?
This is important because the claims address on the card isn’t always the correct address and if you submit to the wrong address your claims will be rejected. It gets complicated so it’s important to have a biller who makes sure that the claims are filed correctly to avoid payment delays.
Can mental health providers balance bill their clients?
Mental health practices that have contracted with insurance companies cannot balance bill their clients. They must accept the rate the insurer provides and write off any remaining balance. If you’re out of an insurer’s network, you may accept reimbursement from the insurer and then bill the patient for the rest.
Types of Covered Mental Health Services
It's important to know the types of covered mental health services for your patients who may have varying insurance or medical coverage. For example, some insurance will only cover mental health services by specific providers, such as physicians, psychiatrists, clinical psychologists and clinical social workers.
The Role of Medical Record Documentation
Private practice billing services must include proper documentation. Everything transpiring between a patient and the mental healthcare provider should be in the medical record.
Diagnosis Coding
Diagnosis coding allows mental health professionals to identify different treatments, diagnoses or actions given to the patient. Diagnosis coding is documented to make it easier to categorize different mental disorders or diagnostic evaluations during therapy. These codes are essential for the billing process concerning insurance.
Why Mental Health Billing Can Be Complicated
There are many different mental health treatments and services with varying restraints that can make medical billing difficult. To break it down, let's compare it to routine checkups at a doctor for your physical health. In this case, most exams are pretty standard and similar.
Tips for Mental Health Billing
When learning how to bill for therapy services, there is always room for improvement and efficiency. Some elements can speed up insurance billing and ensure a reduction in errors — benefitting mental health providers and patients alike. Consider these mental health billing tips that can help make the process smoother.
Always Double Check Each Patient's Insurance
As with any mental and behavioral health industry procedure, it doesn't hurt to double-check yourself. If you have had issues with incorrect information in the past leading to claims issues, it's always best to implement double-checking in your practice. Confirming your patient's insurance is one of these areas where you want to be certain.
Perform a Verification of Benefits
As mentioned above, the verification of benefits (VOB) is important to confirm a patient's insurance coverage and the service they intend to receive. In this process, you can check your patient's policy for information that won't often be directly on their insurance card.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This article contains coding and other guidelines that complement the Local Coverage Determination (LCD) for Psychiatry and Psychology Services.
ICD-10-CM Codes that Support Medical Necessity
The correct use of an ICD-10-CM code listed below does not assure coverage of a service. The service must be reasonable and necessary in the specific case and must meet the criteria specified in the related determination.
ICD-10-CM Codes that DO NOT Support Medical Necessity
Severe and profound intellectual disabilities (ICD-10-CM codes F72, F73, and F79) are never covered for psychotherapy services or psychoanalysis (CPT codes 90832-90840, 90845-90849 and 90853). In such cases, rehabilitative, evaluation and management (E/M) codes should be reported.
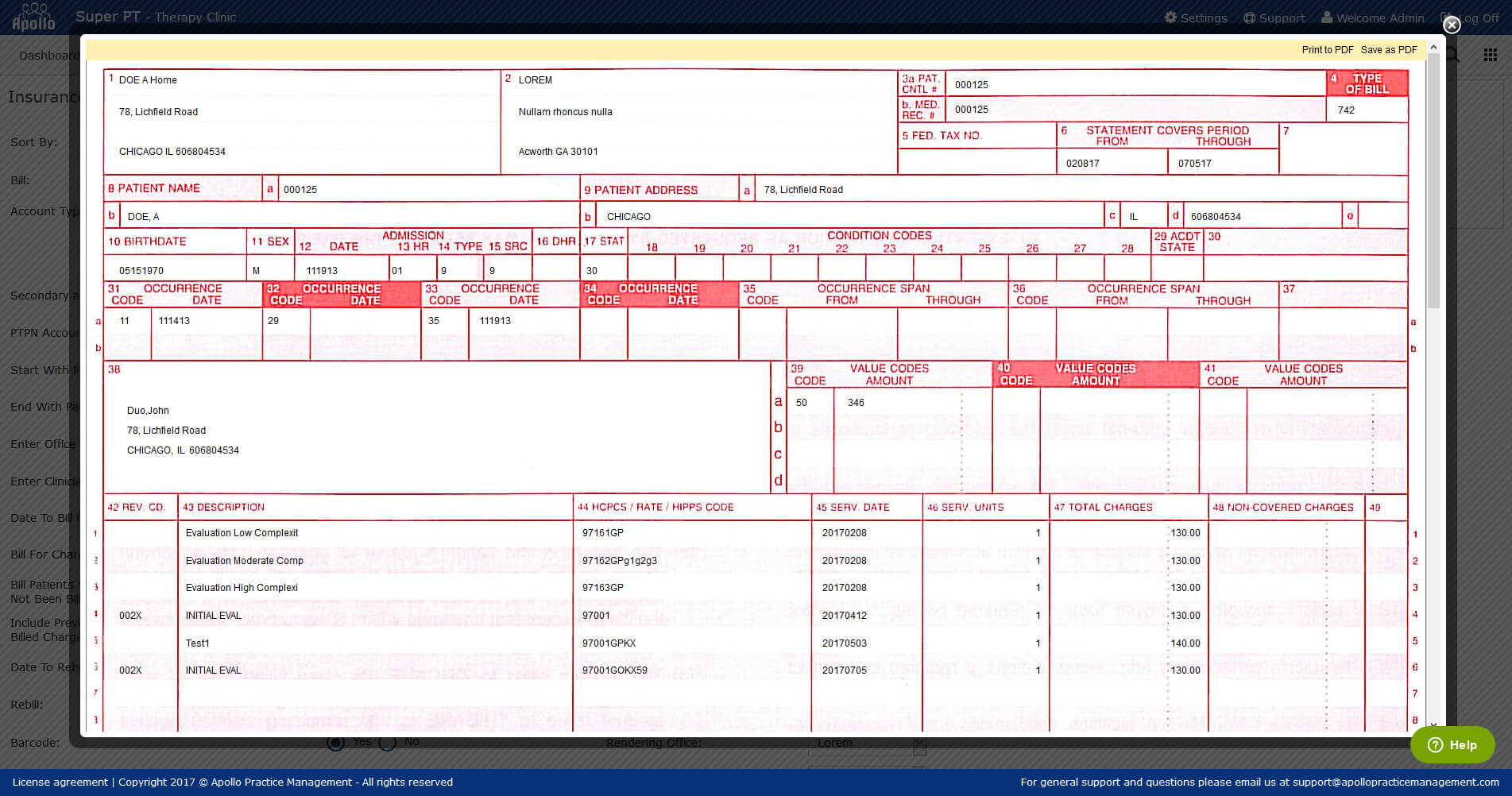
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
How does the Mental Health Act affect Medicare?
The legislation enhances Medicare beneficiaries’ access to the valuable services of independent CSWs in two scenarios: The Improving Access to Mental Health Act also increases the Medicare reimbursement rate for CSWs from 75% to 85% of the physician fee schedule, thereby mitigating reimbursement inequity .
Who introduced the Mental Health Act?
870/H.R. 2035). This legislation was introduced in a bipartisan manner by Senators Debbie Stabenow, MSW (D-MI), and John Barrasso, MD (R-WY), and has a companion House bill introduced by Representative Barbara Lee, MSW (D-CA-13).
What is the Medicare reimbursement rate for CSWs?
The Improving Access to Mental Health Act also increases the Medicare reimbursement rate for CSWs from 75% to 85% of the physician fee schedule, thereby mitigating reimbursement inequity.
Can Medicare beneficiaries receive mental health services?
However, beneficiaries who receive SNF services under Medicare Part A cannot simultaneously receive services from an independent CSW under Part B. This limits the pool of practitioners who can serve SNF residents, which is problematic given the high incidence of mental health conditions among SNF residents, and the high ratio of 120 residents to every medical social worker (who may not actually have received a social work degree). This access barrier exists because when SNF consolidated billing was implemented, psychiatrists’ and psychologists’ services were excluded from the Prospective Payment System, but CSW services were not. Medicare beneficiaries who transfer from a setting in which they receive mental health services from an independent CSW under Medicare Part B to a SNF, where they cannot receive such services, experience a disruption in care. Such care transitions can occur even if the beneficiary is moved within the same building or remains in the same bed. The reimbursement restriction also limits the pool of Medicare providers available to meet newly identified mental health needs of beneficiaries during a SNF stay. Correcting this will enhance beneficiaries’ access to mental health services in SNFs.
Can you get Medicare Part B reimbursement for a psychiatrist?
Although beneficiaries can access Medicare Part B–reimbursed HBAI services from psychologists and psychiatrists, they cannot access them from independent CSWs. This access barrier exists because Medicare Part B reimbursement for independent CSW services is restricted to the diagnosis and treatment of mental illness.
Is Blue Cross Blue Shield the highest reimbursing plan?
To sum things up, the Blue Cross and Blue Shield network across the United States is one of the highest reimbursing and most competitive plans to work with. Inquire about your local BCBS within google by typing in “Blue Cross Blue Shield” + your state’s name.
Does Medicaid pay poorly?
Sadly, Medicaid pays poorly and is overly complex, often requiring license-level modifiers and taxonomy codes. The reason I would recommend working with Medicaid is to establish a very busy practice (perhaps with a billing team on your side) and/or because you want to serve this population of folks in need.
Is Medicaid subcontracted?
Many Medicaid polices are subcontracted out to lower paying organizations. This can skew data downward in comparison to brands that to not facilitate a Medicaid plan in that State. Likewise, EAP sessions have far more hoops, billing nuance, and prior-to-session manual labor (authorizations) involved in billing.
