Is there a modifier for urodynamic codes?
Sep 19, 2019 · The –GA modifier (“Waiver of Liability Statement Issued as Required by Payer Policy”) should be used when physicians, practitioners, or suppliers want to indicate that they anticipate that Medicare will deny a specific service as not reasonable and necessary and they do have an ABN signed by the beneficiary on file.
What modifier should be used for billing non-covered services?
Oct 24, 2019 · Local Coverage Articles are a type of educational document published by the Medicare Administrative Contractors (MACs). Articles often contain coding or other guidelines that are related to a Local Coverage Determination (LCD). Finding a specific code. Some articles contain a large number of codes.
What is the CPT code for full Urodynamic testing?
Jan 06, 2019 · Billing Tips: Report the CPT code with the highest RVU first. In most cases, this will be either 51729, 51728, 51727, or 51726. All other codes are reported with the -51-modifier appended, to designate additional procedures. Typically, this would be attached to a complex uroflowmetry study done at the same time e.g. 51741-51.
What are the reimbursement trends for urodynamics in 2020 (UDS)?
If a physician performs more than one urodynamic procedure on the same patient on the same day, Medicare will pay as follows: The primary procedure (billed first) at 100% of the fee schedule amount; the subsequent procedures (billed using a “51” modifier) will be paid at 50% of the fee schedule amount.

Is urodynamics covered by Medicare?
How do you bill for urodynamics?
What is the 26 modifier?
Does Medicare accept RT and LT modifiers?
What is the CPT code for urodynamics test?
What is the CPT code for cystoscopy?
What is the difference between modifier TC and 26?
What is 59 modifier used for?
What is a 54 modifier?
When a physician or other qualified health care professional performs a surgical procedure and another provides preoperative and/or postoperative management, surgical services may be identified by adding this modifier to the usual procedure code.Feb 12, 2020
What is 76 modifier used for?
Used to indicate a procedure or service was repeated by the same physician or other qualified health care professional subsequent to the original procedure or service.Jan 25, 2022
Does Medicare pay for modifier 50?
Medicare will allow 100% of the highest paying surgical procedure on the claim plus 50% for the other ASC-covered surgical procedures furnished in the same session.
What is the Xu modifier used for?
What happens if you submit a claim without a diagnosis code?
A claim submitted without a valid ICD-10-CM diagnosis code will be returned to the provider as an incomplete claim under Section 1833 (e) of the Social Security Act.
Why do contractors need to specify revenue codes?
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination. Complete absence of all Revenue Codes indicates that coverage is not influenced by Revenue Code and the article should be assumed to apply equally to all Revenue Codes.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Articles. CMS believes that the Internet is an effective method to share Articles that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
What is a bill and coding article?
Billing and Coding articles provide guidance for the related Local Coverage Determination (LCD) and assist providers in submitting correct claims for payment. Billing and Coding articles typically include CPT/HCPCS procedure codes, ICD-10-CM diagnosis codes, as well as Bill Type, Revenue, and CPT/HCPCS Modifier codes. The code lists in the article help explain which services (procedures) the related LCD applies to, the diagnosis codes for which the service is covered, or for which the service is not considered reasonable and necessary and therefore not covered.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Is CPT copyrighted?
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. American Medical Association. All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the American Medical Association (AMA).
Where are articles related to LCD?
Articles are often related to an LCD, and the relationship can be seen in the “Associated Documents” section of the Article or the LCD.
Who performs urodynamics?
Urodynamics can be performed by non-physician practitioners such as physician assistants, nurse, or medical technician. However, billing for these services requires direct supervision, which means that the billing physician must be present in the office when that individual performs the urodynamics.
What is the EMG code for uroflowmetry?
51741 for complex uroflowmetry 51729 for complex cystometrogram, including measurement of urethral pressure and bladder voiding/flow pressure 51784 or 51785 for the EMG +51797 for the abdominal pressure, whether measured rectally or vaginally
What is urodynamic testing?
Urodynamic testing is specialized testing of the bladder, urethra and pelvic floor function during urine storage and micturition. The testing utilizes small pressure measuring catheters to assess bladder (detrusor) pressure and compliance as well as urethral sphincter pressure and tone. Assessment of levator muscle function during the storage and micturition phases can also be assessed.
What is the modifier for diagnostic services?
Payment for diagnostic services consists of a technical component and a professional component. These components are identified by the modifiers –TC (technical component) and -26 (professional component) appended to the CPT code. The absence of a modifier represents “global” billing (technical component + professional component). When the physician only interprets the results and/or operates the equipment, the professional component (i.e., modifier -26 appended) is reported. When multiple procedures are performed in the same investigative session, modifier -51 (“multiple procedures”) should be appended.
Is CPT copyrighted?
Current Procedural Terminology (CPT®) is copyright 2017 American Medical Association (AMA). All Rights Reserved. No fee schedules, basic units, relative values or related listings are included in CPT. The AMA assumes no liability for the data contained herein. CPT is a registered trademark of the American Medical Association.
What are the modifiers for urodynamics?
Three other modifiers that might be used with urodynamic coding are -58, -78, and -79. These modifiers are necessary if the urodynamic test is performed while patient is in a 90-day post-surgery global period. The -58 modifier is used if the urodynamic test is a planned or staged part of the surgery (dictated as part of the plan in the operative note) that created the post-operative global period. The -78 modifier is used when there is an unplanned need for urodynamics during the global post-operative time period because of a medical problem related to the original surgery. The -79 modifier is used when the same physician is performing urodynamics on a patient during the post-operative global time period for a medical condition not related to the original surgery. Of note, when the above three codes are used correctly, reimbursement should not be affected.
What are the modifiers in CPT?
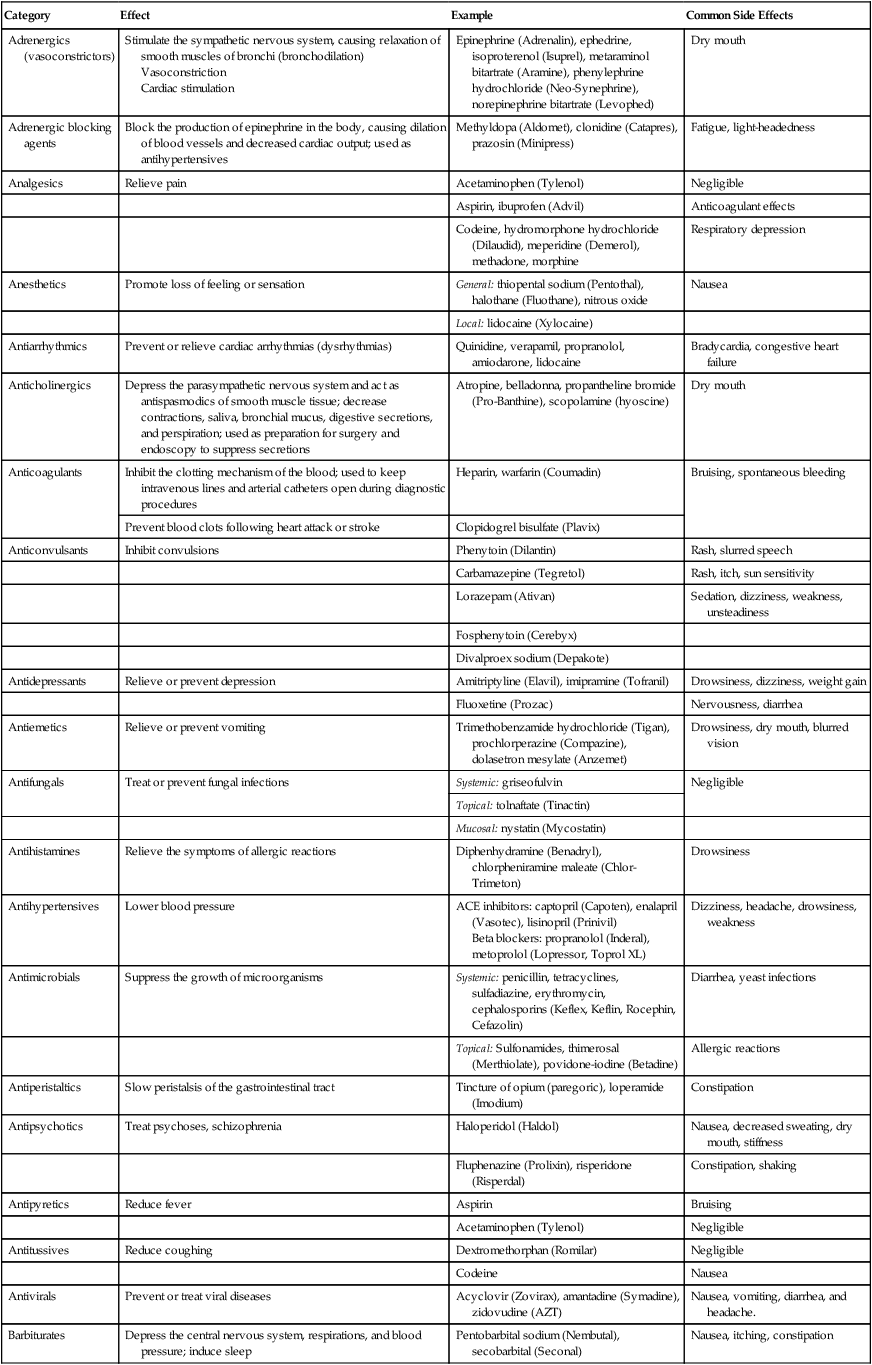
Modifiers are two digit codes that are added to a CPT Procedure code or E&M code in order to clarify the services being billed . The four most commonly used modifiers for urodynamic billing by a physician are the -26, -51, -25, and -59 modifiers. This information is summarized in Table 4.2 .
What is a 26 modifier?
The -26 modifier is used ONLY for diagnostic tests performed in a facility setting where reimbursement is being shared between the facility and the physicians. The -26 modifier designates the professional component of a service provided, such as interpretation of a test results. The -26 modifier tells CMS or other payers that it needs to split reimbursement between the physician and the facility. The physician will receive reimbursement for the Professional Component and the facility receives reimbursement for the Technical Component.
What is the conversion factor for Medicare?
The conversion factor (CF for 2013 was $34.0230) is a simple way for Medicare and the government to control cost by adjusting physician reimbursement [ 4 ]. Recently, the implementation of cuts to the conversion factor has been an important topic in the news and medical society communications. Large decreases in the CF have continually been delayed by congress over the past 5 years. Unless it is again delayed, changes to the conversion factor will cut physician reimbursement by 25 % in January 2014.
When to use a 25 modifier?
The -25 modifier is used when billing for both an E&M code and a procedure code on the same day. This is often used if the urodynamics are done in the setting of a new patient encounter. The E&M code should be separate, identifiable, and above and beyond what is expected for the procedure/s performed. As long as the visit is properly documented and the modifier is used, billing for a new patient encounter and urodynamics on the same day should not affect reimbursement.
Is a diagnostic test a reimbursement?
If a diagnostic test is performed in a facility then only the PC will be used to calculate reimbursement to the physician. However, if a diagnostic test is not being performed in a facility then the physician is reimbursed based on the total Global RVU. It is the authors’ opinion that if a physician is performing diagnostic tests in a facility setting, the facility should be paying a portion of the physician’s malpractice expenses because the facility is being reimbursed for malpractice coverage by CMS as part of the TC. Of note, there are some CPT codes that are either only PC or only TC. Lastly, the TC payment amount reimbursed to a facility also depends on whether it is a hospital or ambulatory surgery center.
Who performs urodynamics?
Urodynamics can be performed by non-physician practitioners such as physician assistants, nurse, or medical technician. However, billing for these services requires direct supervision, which means that the billing physician must be present in the office when that individual performs the urodynamics.
What is the EMG code for uroflowmetry?
51741 for complex uroflowmetry 51729 for complex cystometrogram, including measurement of urethral pressure and bladder voiding/flow pressure 51784 or 51785 for the EMG +51797 for the abdominal pressure, whether measured rectally or vaginally
What is urodynamic testing?
Urodynamic testing is specialized testing of the bladder, urethra and pelvic floor function during urine storage and micturition. The testing utilizes small pressure measuring catheters to assess bladder (detrusor) pressure and compliance as well as urethral sphincter pressure and tone. Assessment of levator muscle function during the storage and micturition phases can also be assessed.
Is modifier 51 required for Medicare?
Note that for Medicare, modifier –51 is not required, but the order on the bill should be listed as above.
Is a nurse practitioner billed for a urology test?
Every procedure in the office is billed as if a qualified provider (the urologist, a physician assistant, or nurse practitioner) provided the service. Therefore, the nurse (or technician) who performs a test is not reimbursed; the service is instead charged as an "incident to" service by the qualified provider who is immediately available and in the office at the time of the procedure.
