Medicare ABN Specific Modifiers – GA, GX, GY, GZ
- GA Modifier: Waiver of Liability Statement Issued as Required by Payer Policy. ...
- GX Modifier: Notice of Liability Issued, Voluntary Under Payer Policy. ...
- GY Modifier: Notice of Liability Not Issued, Not Required Under Payer Policy. ...
- GZ Modifier: Item or Service Expected to Be Denied as Not Reasonable and Necessary. ...
- GA Modifier: Waiver of Liability Statement Issued as Required by Payer Policy. ...
- GX Modifier: Notice of Liability Issued, Voluntary Under Payer Policy. ...
- GY Modifier: Notice of Liability Not Issued, Not Required Under Payer Policy. ...
- GZ Modifier:
Which modifier goes first 25 or 95?
You put the modifier that affects payment the most first. Since AI is informational only and the 25 determine if the visit level should be paid ... put the 25 first then the AI You must log in or register to reply here.
What is Kx modifier with Medicare?
KX Modifier Thresholds (formerly known as Therapy Cap Process) Under Medicare Part B, the annual limitations on per beneficiary incurred expenses for outpatient therapy services are commonly referred to as “therapy caps” now known as KX modifier thresholds. The KX modifier thresholds are determined on a calendar year basis, which means that all beneficiaries begin a new threshold amount each year.
What is a Gy modifier for Medicare?
- Are proper and needed for the diagnosis or treatment of the patient’s medical condition
- Are furnished for the diagnosis, direct care, and treatment of the patient’s medical condition
- Meet the standards of good medical practice
- Are not mainly for the convenience of the patient, provider, or supplier Examples of services that are covered include:
When to use Medicare ABN claim modifiers?
You may also use the ABN as a voluntary notice to alert patients of their financial liability prior to providing care that Medicare never covers. An ABN is not required to bill a patient for an item or service that is not a Medicare benefit and is never covered. Medicare prohibits routine issuing of ABNs.
What is a modifier?
What is anesthesia modifier?
What is a performance modifier?
Can you use more than one modifier in a CPT code?
Can you bill Medicare for a trip with a modifier?

Does Medicare accept modifier 59?
Modifier 59 is not going away and will continue to be a valid modifier, according to Medicare. However, modifier 59 should NOT be used when a more appropriate modifier, like a XE, XP, XS or XU modifier, is available. Certain codes that are prone to incorrect billing may also require one of the new modifiers.
Does Medicare accept modifiers?
A clear understanding of Medicare's rules and regulations is necessary to assign the appropriate modifier. Examples of when modifiers may be used: Identification of professional or technical only components. Repeat services by the same or different provider.
Is the 25 modifier only for Medicare?
Definition of modifier 25 Medicare requires that modifier 25 be used only on claims for E/M services and only when the E/M service is provided by the same physician on the same day as a global procedure or service.
Does Medicare accept modifier LT and RT?
Several DME MAC LCD-related Policy Articles require the use of the RT and LT modifiers for certain HCPCS codes. The right (RT) and left (LT) modifiers must be used when billing two of same item or accessory on the same date of service and the items are being used bilaterally.
Is the GA modifier only for Medicare?
The GA HCPCS modifier indicates that there is an ABN on file. The GY HCPCS modifier indicated that an item or service is statutorily non-covered or in not a Medicare benefit.
Should I use GT or 95 modifier?
A GT modifier is an older coding modifier that serves a similar purpose as the 95 modifier. CMS recommends 95, different companies have varying standards for which codes to be billed. It is a good idea to check with the plans before billing.
What are modifiers 25 and 59?
The CPT defines modifier 59 as a “distinct procedural service.” General Guidelines for Modifier 59 from the CPT: Modifier 59 is used to identify procedures/services, other than E&M services, that are not normally reported together, but are appropriate under the circumstances. date, see modifier 25.
What is 26 modifier used for?
Current Procedural Terminology (CPT®) modifier 26 represents the professional (provider) component of a global service or procedure and includes the provider work, associated overhead and professional liability insurance costs. This modifier corresponds to the human involvement in a given service or procedure.
Can you bill modifier 57 and 25 together?
A visit or consultation is not billed in addition to the procedure. Both Major and Minor Surgeries on the Same Day When a decision for surgery includes both major and minor surgeries and is made the day of surgery, the E&M billed for the decision must have both modifier –57 and modifier –25 appended.
Does Medicare accept the 50 modifier?
Medicare will allow 100% of the highest paying surgical procedure on the claim plus 50% for the other ASC-covered surgical procedures furnished in the same session.
Does modifier 59 go before RT?
Contributor. different shoulders, modifiers RT and LT should be used, not modifier 59. LT and RT have not effect on the actual processing of the claim for payment, because they are informational.
What is the LT modifier used for?
Modifier LT This modifier is used to identify procedures performed on left side of body. Be sure to determine if HCPCS modifier LT is applicable for a particular procedure code. It does not affect allowed amount on a claim; however, lack of a required modifier can cause denials or development to occur.
Can you use modifiers on CPT® add-on codes?
Modifiers may be appropriate on CPT® add-on codes (identified here and in many coding resources with a +), but you should confirm that the individu...
Can you use CPT® modifiers on HCPCS Level II codes and vice versa?
There is no general restriction on using the modifiers from one code set (CPT® or HCPCS Level II) with the codes from another code set, and such us...
Can you append more than one modifier to a CPT® or HCPCS Level II code?
Appending both CPT® and HCPCS Level II modifiers to a single code may be appropriate. For instance, an encounter may call for both CPT® modifier 22...
What is the difference between modifier 52 and modifier 53?
Pro-fee coders may consider appending modifier 52 Reduced services or modifier 53 Discontinued procedure to a medical code when a provider does not...
When should you use repeat modifiers 76 and 77?
Modifier 76 Repeat procedure or service by same physician or other qualified health care professional is appropriate to use when the same provider...
What are the ABN modifiers (GA, GX, GY, GZ)?
An Advance Beneficiary Notice of Noncoverage (ABN) form helps a beneficiary decide whether to get an item or service that Medicare may not cover. T...
Is drug-waste modifier JW only for Medicare?
Modifier JW Drug amount discarded/not administered to any patient is not limited to use for Medicare claims. Other third-party payers also may acce...
When should you use modifier KX?
Modifier KX Requirements specified in the medical policy have been met is appropriate in a variety of circumstances. In particular, Medicare and so...
When should you use hospice modifiers GV and GW?
The hospice modifiers are modifier GV and GW:GV Attending physician not employed or paid under arrangement by the patient’s hospice providerGW Serv...
Does Medicare provide information about preventive services modifier 33?
Modifier 33 Preventive services is referenced in Medicare Claims Processing Manual, Chapter 18.Section 1.2 and Section 60.1.1 both state, “Coinsura...
Modifiers - Complete Listing - Novitas Solutions
Some modifiers cause automated pricing changes, while others are used for information only. When selecting the appropriate modifier to report on your claim, please ensure that it is valid for the date of service billed.
List of CPT & HCPCS MODIFIERS - Medical billing cpt modifiers and list ...
Modifiers Definition A modifier provides the means by which the reporting provider can indicate that a service or procedure that has been performed has been altered by some specific circumstance but not changed in its definition or code.
Coding Modifiers Table
20. . . or. . or. . .
Modifiers Used with Procedure Codes (modif used)
modif used 2 Part 2 – Modifiers Used with Procedure Codes Page updated: May 2022 Allowable Modifiers The “Allowable Modifiers” column refers to services or procedures that may use certain
Where to find the definition of modifier?
The definition of each modifier can be found within the document linked in the type of modifier column in the chart below.
What to do if you need more than one modifier?
If more than one modifier is needed, list the payment modifiers —those that affect reimbursement directly—first.
What does "modify" mean in a service?
Modifiers indicate that a service or procedure performed has been altered by some specific circumstance, but not changed in its definition or code. They are used to add information or change the description of service in order to improve accuracy or specificity. Modifiers can be alphabetic, numeric or a combination of both, but will always be two digits.
Does CMS have modifiers?
There are times when coding and modifier information issued by CMS differs from the American Medical Association regarding the use of modifiers. A clear understanding of Medicare's rules and regulations is necessary to assign the appropriate modifier.
Can you list multiple informational modifiers in any order?
If multiple informational/statistical modifiers apply, you may list them in any order (as long as they are listed after payment modifiers).
What are the two types of modifiers?
There are two types of modifiers A) Level 1 Modifier and B) Level 2 Modifier.
What is a CPT modifier?
CPT Modifiers are an important part of the managed care system or medical billing. A service or procedure that has both a professional and technical component. (26 or TC) A service or procedure that was performed more than once on the same day by the same physician or by a different physician. (76 or 77)
Why is CPT modifier important?
CPT Modifiers are also playing an important role to reduce the denials also. Using the correct modifier is to reduce the claims defect and increase the clean claim rate also. The updated list of modifiers for medical billing is mention below
What is Medicare modifier 52?
Modifier 52- Reduced services. Under certain circumstances, a service or procedure is partially reduced or elimininated at the physician’s direction. Medicare requires and operative report for surgical procedures and s concise statement as to how the reduced service is different from standard procedure. Claims for non surgical services reported with modifier 52 must contain a statement as to how the reduce service is different from standard service.
What is a modifier AD?
Modifier AD – Medical supervision by a physician, more than four services is an anesthesiologist.
What is a modified 53 procedure?
Modifier 53- Discontinued procedure. Under certain circumstances the physician may elect to terminate a surgical or diagnostic procedure. An operative report is required as well as a statement as to how much of the original procedure was accomplished.
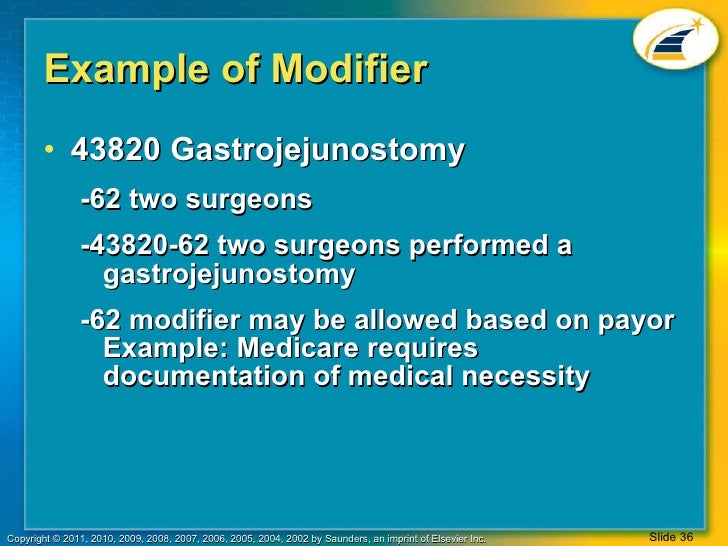
When to use modifier 62?
Modifier 62- WhenTwo surgeons involved in the procedure. When 2 surgeons work together as primary surgeons performing distinct parts of procedure, each surgeon should report the distinct operative work adding the modifier 62 to the procedure code and any associated add on code for that procedures as long as both surgeons continue to work together primary surgeon.
Why is it important to use modifiers?
Proper use of modifiers is important both for accurate coding and because some modifiers affect reimbursement for the provider. Omitting modifiers or using the wrong modifiers may cause claim denials that lead to rework, payment delays, and potential reimbursement loss.
What is the most problematic requirement for modifier 25?
Many coders find that determining whether an E/M service is significant and separately identifiable is the most problematic requirement for modifier 25 use. The documentation must clearly show that the provider performed extra E/M work beyond the usual work required for the other procedure or service on the same date. In other words, if you removed all the documentation represented by the code for the other procedure or service, would the remaining documentation support reporting an E/M code?
What is a pricing modifier?
A pricing modifier is a medical coding modifier that causes a pricing change for the code reported. The Multi-Carrier System (MCS) that Medicare uses for claims processing requires pricing modifiers to be in the first modifier position, before any informational modifiers. On the CMS 1500 claim form, the appropriate field is 24D (shown below). You enter the pricing modifier directly to the right of the procedure code on the claim. Most providers use the electronic equivalent of this form to bill Medicare for professional (pro-fee) services.
What is a modifier 59?
Modifier 59 Distinct procedural service is a medical coding modifier that indicates documentation supports reporting non-E/M services or procedures together that you normally wouldn’t report on the same date. Appending modifier 59 signifies the code represents a procedure or service independent from other codes reported and deserves separate payment.
What is informational modifier?
An informational modifier is a medical coding modifier not classified as a payment modifier. Another name for informational modifiers is statistical modifiers. These modifiers belong after pricing modifiers on the claim.
How many doctors are required to perform a procedure?
A procedure requires two physicians of different specialties to perform it. Each reports the code with modifier 62 appended. Two surgeons simultaneously perform parts of a procedure, such as for a heart transplant or bilateral knee replacements. Again, each surgeon reports the code with modifier 62 appended.
When to use modifier 25?
Suppose the physician sees a patient with head trauma and decides the patient needs sutures. After checking allergy and immunization status , the physician performs the procedure. An E/M is not separately reportable in this scenario. But, if the physician performs a medically necessary full neurological exam for the head trauma patient, then reporting a separate E/M with modifier 25 appended may be appropriate.
How to request reconsideration for Medicare PTP?
If you would like to make a Medicare PTP reconsideration request, please email us at [email protected] with exact code pairs, detailed reconsideration, new proposed edits, and any supporting documentation you have . **NOTE** Any submissions made to the NCCI contractor that contain Personally Identifiable Information (PII) or Protected Health Information (PHI) are automatically discarded, regardless of the content, in accordance with federal privacy rules with which the NCCI Contractor must comply.
How often are NCCI edits valid?
There is no set time period for which NCCI edits are valid. Some edits may remain in place indefinitely. The PTP edits and MUEs may be updated at least quarterly.
What does MAI mean in CMS?
The MUE files on the CMS NCCI website display an MAI for each HCPCS/CPT code. An MAI of “1” indicates that the edit is a claim line edit. An MAI of “2” or “3” indicates that the edit is a date of service MUE.
What is CMS MUE?
The CMS MUE program was developed to reduce the paid claims error rate for Medicare claims. MUEs are designed to reduce errors due to clerical entries and incorrect coding based on criteria such as anatomic considerations, HCPCS/CPT code descriptors, CPT coding instructions, established CMS policies, nature of a service/procedure, nature of an analyte, nature of equipment, prescribing information, and claims data.
What is a MUE in CMS?
For date of service MUEs, the claims processing system sums all UOS on all claim lines with the same HCPCS/CPT code and date of service. The MUE files on the CMS NCCI webpage display an “MUE Adjudication Indicator ” (MAI) for each HCPCS/CPT code. An MAI of “1” indicates that the edit is a claim line MUE. An MAI of “2” or “3” indicates that the edit is a date of service MUE. Further information is available in MLN Matters MM8853.
How often are NCCI PTP files updated?
The NCCI PTP edit files and MUEs files are updated at least quarterly.
Where can I find the NCCI policy manual?
The NCCI Policy Manual for Medicare Services may be obtained on the CMS NCCI webpage.
What is a modifier in Medicare?
Modifiers Definition#N#A modifier provides the means by which the reporting provider can indicate that a service or procedure that has been performed has been altered by some specific circumstance but not changed in its definition or code.#N#For Medicare purposes, modifiers are two-digit codes that may consist of alpha and/or numeric characters, which may be appended to Healthcare Common Procedure Coding System (HCPCS) procedure codes to provide additional information needed to process a claim. This includes HCPCS Level 1, also known as Current Procedural Terminology® (CPT®) codes, and HCPCS Level II codes. Modifiers answer questions such as: which one, how many, what kind and when.#N#What is the purpose of using a modifier?
How to use modifiers in Blue Cross?
For Blue Cross claims filing, modifiers, when applicable, always should be used by placing the valid CPT or HCPCS modifier (s) in Block 24D of the CMS-1500 claim form. A complete list of valid modifiers is listed in the most current CPT or HCPCS code book. Please ensure that your office is using the current edition of the code book reflective of the date of service of the claim. If necessary, please submit medical records with your claim to support the use of a modifier.
What is modifier 47?
Modifier 47 – This modifier should be appended only to the surgical procedure code when applicable. It is not appropriate to use this modifier on anesthesia procedure codes. The anesthesiologist would not use this modifier. Do not report modifier 47 when the physician reports moderate (conscious) sedation. 50 26, LT, RT, TC KMAP uses the Medicare Physician Fee Schedule Relative Value file to determine which procedures are appropriately billed with modifier 50. KMAP uses the Bilat Surg indicator field on the file as a basis to determine proper usage of modifier 50. 54 55, 56, 80, 81, 82, AS When one physician performs a surgical procedure and another provides preoperative and/or postoperative management, surgical codes can be identified by adding the modifier 54. Physicians who perform the surgery and furnish all of the usual pre- and post-operative work bill for the global package by entering the appropriate CPT® KMAP uses the Medicare Physician Fee Schedule Relative Value file to determine which procedures are appropriately billed with modifier 54. code for the surgical procedure only; therefore, modifiers 54 and 55 cannot be combined on a single detail line item. KMAP uses the Glob Days field on the file as a basis to determine proper usage of modifier 54. The following determinations have been made based on the individual indicators.
What is the amount of anesthesia allowed by a surgeon?
Amount allowed is 25% of the surgical procedure allowance.
Why is correct modifier important?
Correct modifier use is an important part of avoiding fraud and abuse or noncompliance issues, especially in coding and billing processes involving government programs.
When to use modifier 76?
Modifier 76 is used when the procedure is repeated by the same physician subsequent to the original service. The repeat service must be identical to the initial service provided. This modifier is separate and distinct from modifiers 58, 78, and 79. Please refer to details for these modifiers.
How many unrelated evaluation and management services by the same physician during a postoperative period?
24 Unrelated Evaluation and Management Service by the Same Physician During a Postoperative Period
What is a modifier?
Modifiers can be two digit numbers, two character modifiers, or alpha-numeric indicators. Modifiers provide additional information to payers to make sure your provider gets paid correctly for services rendered.
What is anesthesia modifier?
Anesthesia modifiers are used to receive the correct payment of anesthesia services. Pricing modifiers must be placed in the first modifier field to ensure proper payment (AA, AD, QK, QX, QY, and QZ). Informational modifiers are used in conjunction with pricing modifiers and must be placed in the second modifier position (QS, G8, G9, and 23).
What is a performance modifier?
Performance measure modifiers are used to indicate to special circumstances of a patient's encounter with the physician.
Can you use more than one modifier in a CPT code?
If appropriate, more than one modifier may be used with a single procedure code; however, are not applicable for every category of the CPT codes. Some modifiers can only be used with a particular category and some are not compatible with others.
Can you bill Medicare for a trip with a modifier?
Trips with one of these origin/destination modifiers are not covered and should not be submitted to Medicare. A provider may bill the patient directly for these services. If a provider must bill Medicare for a denial, append modifier GY.