
Full Answer
How much does Medicaid cover for nursing home care?
Medicaid: If your income is low, your husband may qualify for Medicaid, which offers different home and community-based services that can pay for in-home care. To investigate this, contact your local Medicaid office. Also see if PACE — which stands for “Programs of All-Inclusive Care for the Elderly” — is available in your area (see NPAonline.org).
Is a nursing home covered by Medicare?
Medicare Part A (Hospital Insurance) typically covers skilled nursing facility care or nursing home care — with the exception that it’s neither custodial nor long-term. You may be able to receive coverage through Medicare Part A if a physician deems it is “medically necessary” for you to have skilled nursing care.
Are nursing homes covered by Medicare and Medicaid?
Most people who enter nursing homes start by paying for their care out-of-pocket. There are several other ways you can pay for nursing home care: Medicaid. Medicaid is a joint federal and state program that helps with medical costs for some people with limited income and resources. Most health care costs are covered if you qualify for both Medicare and Medicaid. Most, but not all, nursing homes accept Medicaid payment.
Will Medicare cover the cost of nursing home?
Yes, private insurers are now required to cover the cost of at-home COVID-19 tests.
Which type of care is not covered by Medicare?
does not cover: Routine dental exams, most dental care or dentures. Routine eye exams, eyeglasses or contacts. Hearing aids or related exams or services.
What type of care does Medicare provide?
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
Does Medicare pay for a nurse visit?
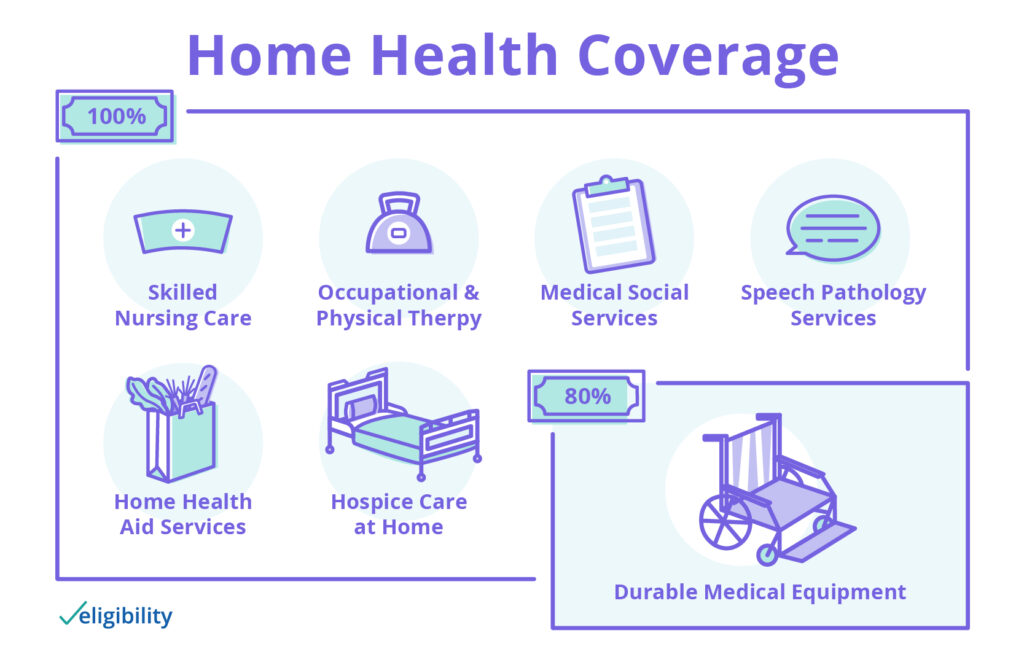
Medicare will pay for 100% of the following services related to home health care: part-time skilled nursing care—usually two to three visits per week in a plan certified by a physician.
What is the 100 day rule for Medicare?
Medicare pays for post care for 100 days per hospital case (stay). You must be ADMITTED into the hospital and stay for three midnights to qualify for the 100 days of paid insurance. Medicare pays 100% of the bill for the first 20 days.
What does Medicare Part B cover in a nursing home?
Original Medicare Part A covers inpatient hospital care, skilled nursing facility care, and hospice stays. Part B provides coverage for outpatient services, such as visits to a doctor's office, durable medical equipment, therapeutic services, and some limited prescription medication.
What are the 3 types of Medicare?
Different types of Medicare health plansMedicare Advantage Plans. ... Medicare Medical Savings Account (MSA) Plans. ... Medicare health plans (other than MA & MSA) ... Rules for Medicare health plans.
Does Medicare pay for home caregivers?
Medicare typically doesn't pay for in-home caregivers for personal care or housekeeping if that's the only care you need. Medicare may pay for short-term caregivers if you also need medical care to recover from surgery, an illness, or an injury.
How Long Will Medicare pay for home health care?
To be covered, the services must be ordered by a doctor, and one of the more than 11,000 home health agencies nationwide that Medicare has certified must provide the care. Under these circumstances, Medicare can pay the full cost of home health care for up to 60 days at a time.
What can RN's bill for?
An RN (or medical / clinic assistant) can only bill for his/her time for an established patient, and only with one particular code. What codes can an RN bill for? Insurance reimbursement coding is based on the American Medical Association CPT2 coding system.
Does Medicare cover ICU costs?
(Medicare will pay for a private room only if it is "medically necessary.") all meals. regular nursing services. operating room, intensive care unit, or coronary care unit charges.
What happens when Medicare hospital days run out?
Medicare will stop paying for your inpatient-related hospital costs (such as room and board) if you run out of days during your benefit period. To be eligible for a new benefit period, and additional days of inpatient coverage, you must remain out of the hospital or SNF for 60 days in a row.
How many days will Medicare pay 100% of the covered costs of care in a skilled nursing care facility?
20 daysSkilled Nursing Facility (SNF) Care Medicare pays 100% of the first 20 days of a covered SNF stay. A copayment of $194.50 per day (in 2022) is required for days 21-100 if Medicare approves your stay.
What Nursing Home Care Does Medicare Cover?
Nursing home care can be broken into two broad categories: Custodial care and skilled nursing care.Custodial careCustodial care is help with daily...
What Nursing Home Care Expenses Will Original Medicare Cover?
If you qualify, then Original Medicare may cover expenses related to your nursing home care in a skilled nursing facility for the first 100 days as...
How Can Medicare Supplement Insurance Plans Help With Nursing Home Care Expenses?
A Medicare Supplement Insurance policy offered by a private company may help you pay for certain Medicare out-of-pocket costs, such as copayments,...
How Can Medicare Advantage Plans Help With Nursing Home Care Expenses?
Some people choose to get their Medicare benefits through Medicare Advantage plans, an alternative way to receive Original Medicare (Part A and Par...
Where Can I Get Help With Nursing Home Care Expenses?
If you need long-term nursing home care after Medicare coverage expires, your state may be able to help you through the Medicaid program. To see if...
When Could I Need Skilled Nursing Care?
You may need skilled nursing care if you have an illness or injury that requires treatment or monitoring. Skilled nursing facilities provide 24-hou...
When Would I Be Eligible For Medicare Coverage of Skilled Nursing Facility Care?
Generally Medicare will help pay for skilled nursing facility (SNF) care if all of these are true: 1. You were a hospital inpatient for at least th...
What Skilled Nursing Facility Services Does Medicare Cover?
Typically Medicare will pay for the following items and services delivered by trained health professionals: 1. Semi-private room 2. Meals 3. Care b...
How Can I Get Help Paying Skilled Nursing Facility Costs?
You might want to consider a Medicare Supplement plan for help paying some of your skilled nursing facility out-of-pocket costs. Medicare Supplemen...
How Can I Find A Medicare-Certified Skilled Nursing Facility?
You can call Medicare to find out about Medicare-certified skilled nursing facilities in your area. Call Medicare at 1-800-MEDICARE (1-800-633-4227...
Does Medicare pay for nursing home care?
If you have had a qualifying inpatient hospital stay and your doctor orders an additional period of treatment in a skilled nursing facility, Medicare Part A generally covers allowable expenses. Your Part A nursing home benefit usually covers:
What are the requirements for Medicare nursing home coverage?
Before Medicare covers skilled nursing home costs, you must have a qualifying hospital stay of at least three inpatient days prior to your nursing home admission. You must have inpatient status for at least three days; time spent in the emergency department or observation unit doesn’t count toward the three-day requirement.
What Medicare nursing home coverage am I eligible for if I need long-term care?
Medicare won’t pay your nursing home costs, but you still have your Part A and Part B benefits while you’re in a nursing home. For example, Part B covers your doctor visits and medical therapy visits, and if you need hospital care, Part A benefits apply. If you have a Part D Prescription Drug Plan, the medications you take in the nursing home are usually covered. You may have to enroll in a plan that works with your nursing home pharmacy, but the facility should help you choose the right coverage.
Do Medicare Supplement insurance plans cover nursing home costs?
Medicare Supplement insurance plans may cover your out-of-pocket costs for doctor visits and other medical services covered under Part A and Part B while you are a nursing home resident.
What does Medicare cover for a hospital stay?
Skilled nursing care. Physical, occupational, and/or speech language therapy. Medicare also may cover: A medical social worker. Dietary counseling if indicated. Medical equipment and devices you use during your hospital stay.
What is covered by Part B?
For example, Part B covers your doctor visits and medical therapy visits , and if you need hospital care, Part A benefits apply. If you have a Part D Prescription Drug Plan, the medications you take in the nursing home are usually covered.
Is home care nursing covered by Medicare?
It is usually not covered by Medicare. Home care nursing is generally home health care provided by a credentialed medical professional. It can be short-term while you recover from an illness or injury, or long-term if you have a serious chronic condition or have chosen hospice care.
What is a benefit period?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF.
What is SNF in Medicare?
Skilled nursing facility (SNF) care. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Care like intravenous injections that can only be given by a registered nurse or doctor. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services.
What is skilled nursing?
Skilled care is nursing and therapy care that can only be safely and effectively performed by, or under the supervision of, professionals or technical personnel. It’s health care given when you need skilled nursing or skilled therapy to treat, manage, and observe your condition, and evaluate your care.
How many days do you have to stay in a hospital to qualify for SNF?
Time that you spend in a hospital as an outpatient before you're admitted doesn't count toward the 3 inpatient days you need to have a qualifying hospital stay for SNF benefit purposes. Observation services aren't covered as part of the inpatient stay.
What services does Medicare cover?
Medicare-covered services include, but aren't limited to: Semi-private room (a room you share with other patients) Meals. Skilled nursing care. Physical therapy (if needed to meet your health goal) Occupational therapy (if needed to meet your health goal)
When does the SNF benefit period end?
The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins. You must pay the inpatient hospital deductible for each benefit period.
How long do you have to be in the hospital to get SNF?
You must enter the SNF within a short time (generally 30 days) of leaving the hospital and require skilled services related to your hospital stay. After you leave the SNF, if you re-enter the same or another SNF within 30 days, you don't need another 3-day qualifying hospital stay to get additional SNF benefits.
What skilled nursing facility services does Medicare cover?
Typically Medicare will pay for the following items and services delivered by trained health professionals:
How can I find a Medicare-certified skilled nursing facility?
Or you can visit Medicare’s web site at Medicare.gov to search and compare skilled nursing facilities . At this web site you may also want to read the guide to choosing a nursing home and/or the checklist of questions to ask when you are visiting skilled nursing facilities.
When could I need skilled nursing care?
You may need skilled nursing care if you have an illness or injury that requires treatment or monitoring. Skilled nursing facilities provide 24-hour care for people who need rehabilitation services or who suffer from serious health issues that are too complicated to be tended at home. Some skilled nursing facilities might have laboratory, radiology and pharmacy services, social and educational programs, and limited transportation to needed health services that are not available at the facility.
How can I get help paying skilled nursing facility costs?
You might want to consider a Medicare Supplement plan for help paying some of your skilled nursing facility out-of-pocket costs. Medicare Supplement (Medigap) plans help pay for some of your out-of-pocket costs under Medicare Part A and Part B, including certain cost-sharing expenses. In most states, plan benefits are standardized across 10 plan types (labeled letters A through N), and each plan includes different benefits and level of coverage. Several of these standardized plans may cover at least a portion of skilled nursing facility copayments.
How long does Medicare benefit last?
You haven’t used up all the days in your Medicare benefit period. A benefit period starts the day you’re admitted to a hospital as an inpatient. It ends when you haven’t been an inpatient in a hospital or skilled nursing facility for 60 days in a row. If you meet these requirements, Medicare may cover skilled nursing facility care ...
What does Medicare pay for?
Typically Medicare will pay for the following items and services delivered by trained health professionals: 1 Semi-private room 2 Meals 3 Care by registered nurses 4 Therapy care (including physical, speech and occupational therapy) 5 Medical social services 6 Nutrition counseling 7 Prescription medications 8 Certain medical equipment and supplies 9 Ambulance transportation (when other transportation would be dangerous to your health) if you need care that’s not available at the skilled nursing facility
How long do you have to be in a hospital to be a skilled nursing facility?
You were a hospital inpatient for at least three days in a row (not counting the day you leave), and you entered a Medicare-certified skilled nursing facility within 30 days of leaving the hospital.
What is covered by Part A?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
How many hours a day is part time nursing?
Part-time or intermittent nursing care is skilled nursing care you need or get less than 7 days each week or less than 8 hours each day over a period of 21 days (or less) with some exceptions in special circumstances.
What is personal care?
Custodial or personal care (like bathing, dressing, or using the bathroom), when this is the only care you need
What is the eligibility for a maintenance therapist?
To be eligible, either: 1) your condition must be expected to improve in a reasonable and generally predictable period of time, or 2) you need a skilled therapist to safely and effectively make a maintenance program for your condition , or 3) you need a skilled therapist to safely and effectively do maintenance therapy for your condition. ...
Does Medicare pay for home health aide services?
Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
Does Medicare change home health benefits?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process. For more information, call us at 1-800-MEDICARE.
Can you get home health care if you attend daycare?
You can still get home health care if you attend adult day care. Home health services may also include medical supplies for use at home, durable medical equipment, or injectable osteoporosis drugs.
What type of insurance covers long term care?
Long-term care insurance. This type of insurance policy can help pay for many types of long-term care, including both skilled and non-skilled care. Long -term care insurance can vary widely. Some policies may cover only nursing home care, while others may include coverage for a range of services, like adult day care, assisted living, ...
How to find out if you have long term care insurance?
If you have long-term care insurance, check your policy or call the insurance company to find out if the care you need is covered. If you're shopping for long-term care insurance, find out which types of long-term care services and facilities the different policies cover.
Does Medicare cover nursing home care?
Medicare generally doesn't cover Long-term care stays in a nursing home. Even if Medicare doesn’t cover your nursing home care, you’ll still need Medicare for hospital care, doctor services, and medical supplies while you’re in the nursing home.
Do nursing homes accept Medicaid?
Most, but not all, nursing homes accept Medicaid payment. Even if you pay out-of-pocket or with long-term care insurance, you may eventually "spend down" your assets while you’re at the nursing home, so it’s good to know if the nursing home you chose will accept Medicaid. Medicaid programs vary from state to state.
Can federal employees buy long term care insurance?
Federal employees, members of the uniformed services, retirees, their spouses, and other qualified relatives may be able to buy long-term care insurance at discounted group rates. Get more information about long-term care insurance for federal employees.
Does Medicare Advantage Cover Skilled Nursing Care?
These include: medical supplies and equipment, semi-private room, ambulance transportation, meals, physical therapy, occupational therapy, medication, and other covered treatments and services. Keep in mind that Medicare will not cover custodial care or long-term care, especially if that’s the only type of care you need.
What is Medicare Advantage?
Medicare Advantage plans are private insurance plans that combine Original Medicare coverage and additional benefits, such as prescription drug coverage. They are sold by private insurance companies that are contracted with Medicare and can serve as an alternative to Original Medicare coverage.
Do you need inpatient care from a skilled nursing facility?
You need inpatient services from a skilled nursing facility and your doctor ordered it
