Does Medicare usually cover in home care?
Medicare will usually cover home health care services that are “medically necessary.”. Home health care services are health services given in the home by trained medical professionals and as part of an overall health plan created by your doctor. Another difference between long-term care and home health care is how long the care is provided.
What in-home care will Medicare cover?
In Home Care Medicare will cover skilled nursing care in the home for a limited time period, but not non-medical care. Care must be prescribed by a doctor and needed part-time only. The senior must be "confined", meaning they are unable to leave the home without the assistance of another person. This is formally referred to as " homebound ".
Which Medicare covers emergency room visits?
Your emergency room costs under Medicare might include:
- A copayment for the emergency room visit and a copayment for the hospital services (you might not know this copayment amount until you get the bill)
- 20% of the Medicare approved amount for doctor visits
- Your Part B deductible applies
Does Medicare cover my home care needs?
There are many misconceptions about what Medicare will cover and how to qualify for it. Medicare only covers limited home care under certain strict conditions. When these conditions are met, Medicare can cover the in-home care needed by you or your loved one for significantly reduced costs, and, in some cases, care is completely free.

Which is generally covered by Medicare for the homebound patient?
Medicare considers you homebound if: You need the help of another person or medical equipment such as crutches, a walker, or a wheelchair to leave your home, or your doctor believes that your health or illness could get worse if you leave your home.
What services are covered under Medicare Part A?
In general, Part A covers:Inpatient care in a hospital.Skilled nursing facility care.Nursing home care (inpatient care in a skilled nursing facility that's not custodial or long-term care)Hospice care.Home health care.
Which is not covered under Medicare Part A?
Part A does not cover the following: A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care.
Does Medicare come to your house?
Remember that Medicare will never call you to sell you anything or visit you at your home. Medicare, or someone representing Medicare, will only call and ask for personal information in these 2 situations: A Medicare health or drug plan may call you if you're already a member of the plan.
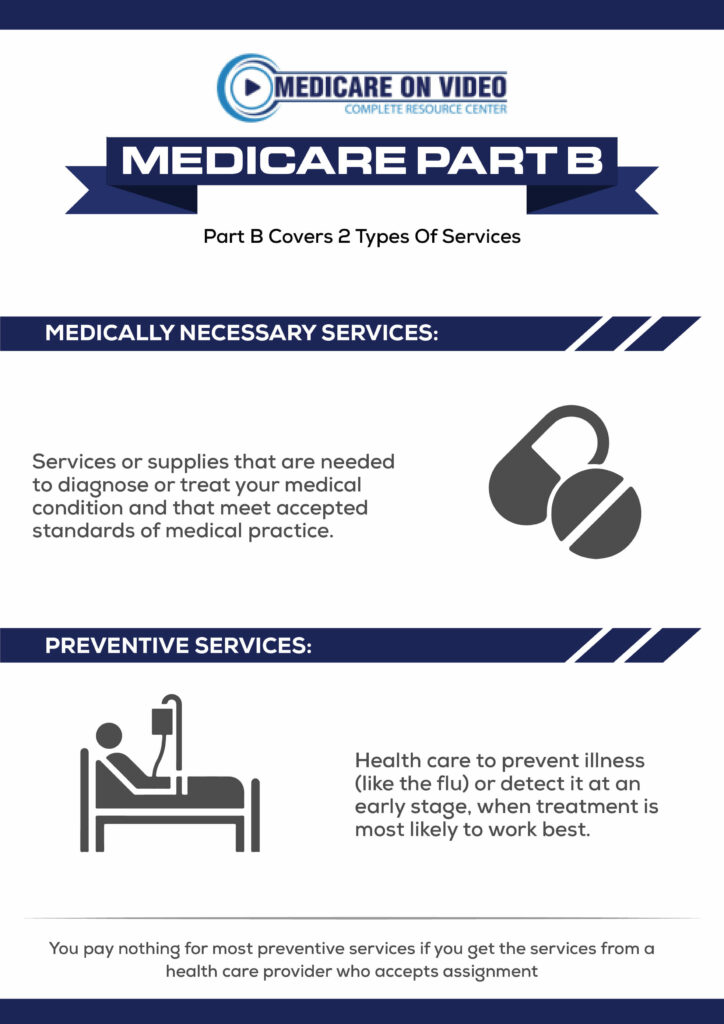
What does Part B of Medicare pay for?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services. Part B also covers some preventive services. Look at your Medicare card to find out if you have Part B.
What is the difference between Part C and Part D Medicare?
Medicare Part C and Medicare Part D. Medicare Part D is Medicare's prescription drug coverage that's offered to help with the cost of medication. Medicare Part C (Medicare Advantage) is a health plan option that's similar to one you'd purchase from an employer.
What's the difference between Medicare Part A and Part B?
If you're wondering what Medicare Part A covers and what Part B covers: Medicare Part A generally helps pay your costs as a hospital inpatient. Medicare Part B may help pay for doctor visits, preventive services, lab tests, medical equipment and supplies, and more.
How Much Does Medicare pay for home health care per hour?
Medicare will cover 100% of the costs for medically necessary home health care provided for less than eight hours a day and a total of 28 hours per week. The average cost of home health care as of 2019 was $21 per hour.
What is not covered by Part A and Part B?
Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
Should you give your Medicare number over the phone?
Treat your Medicare card like it's a credit card. Don't ever give it out except to your doctor or other Medicare provider. Never give your Medicare Number in exchange for free medical equipment or any other free offer. Dishonest providers will use your numbers to get payment for services they never delivered.
Why does United Healthcare do home visits?
HouseCalls helps supplement the care you provide to your patients by visiting them in their home to identify care opportunities, educate them about their health and help reinforce the patient's relationship with you.
Does Medicare make wellness calls?
Medicare will never call you! Medicare may need information from you or may need to reach you; but, they'll NEVER call. You'll get a letter that will notify you of the necessary information that Medicare needs. Long story short, if the calls you're receiving claim to be from Medicare, it's a spam call.
What is home health care?
Home Health Services Medicare Benefits Cover. There are several services Medicare covers under home health visits by a nurse, doctor, or nurse practitioner. They include: Skilled Nursing – This is care that requires a nurse’s skills. The person giving your skilled nursing care must not give services for more than 28 hours a week.
What are the benefits of Medicare?
There are some benefits your Medicare benefits won’t pay for you to have. If you choose to get them, you’ll pay the full cost on your own. These services include: 1 24-hour care 2 Homemaker services like cleaning, shopping, or laundry 3 Delivered meals 4 Personal or custodial care like dressing, bathing, and bathroom assistance
How many hours a day does a skilled nursing home need to be homebound?
Continued occupational therapy. Physical therapy. Speech services. Intermittent skilled nursing care less than eight hours a day. You have to be homebound and have trouble leaving your home or walking without help. The home health agency has to have a certification by Medicare as well.
Do home health agencies have to be certified?
The home health agency has to have a certification by Medicare as well. Additionally, a doctor or nurse practitioner has to document that you’ve had a face-to-face visit within the required timeframe. The face-to-face appointment has to be related to why you need home health services.
Does Medicare cover house calls?
Many people wonder if Medicare benefits cover house calls, and the short answer is yes and no. Medicare did test a house calls program, but it was only in select states for a five-year test. At the end of the five years, they found that house calls did save Medicare money, but doctors would see less than 10 patients a day because ...
Does Medicare pay for social services?
Social Services – As long as your doctor thinks you need these services to address your emotional and social concerns, Medicare will pay for social services. This service includes helping you find community-based services or counseling.
Does Medicare cover durable medical equipment?
Medicare may also cover the cost of durable medical equipment, up to 80%. If your home care agency can’t give you the durable medical equipment, they’ll usually arrange for it through a third-party supplier. The supplier must participate in Medicare and accept assignment.
Home Doctor Visits: What Does Medicare Cover?
Since the beginning of the Covid-19 pandemic, patients have been hesitant to schedule in-person doctor visits – hence the increase in telehealth and telemedicine services. Yet, there are many conditions, services, and treatments for which virtual appointments are far from ideal.
Types of Medicare Coverage
Before you try to figure out whether Medicare will cover a home doctor visit, you’ll need to know which doctors you can visit with your coverage. When you have Original Medicare (Parts A and B), with or without a Medicare Supplement (Medigap) policy, you’ll have coverage for any practitioner accepting Medicare assignment.
When Does Medicare Cover House Calls?
Unfortunately, Medicare doesn’t typically cover the type of house calls with which people are most familiar. Even in the age of Covid, it’s not as simple to make an appointment for a home visit from your primary care physician as it is to schedule a telehealth visit.
Independence at Home
In 2011, the Centers for Medicare & Medicaid Services (CMS) launched a program called the Independence at Home Demonstration. It is a voluntary, primary care program for patients with multiple chronic conditions who are still living independently but would benefit from a doctor’s visit at home.
The Future of Home Doctor Visits on Medicare
Hesitancy to attend in-person medical appointments due to possible Covid-19 exposure increases the need for alternative options. While Medicare now includes more coverage for telehealth than ever, the same cannot be said for house calls.
How do I contact Medicare for home health?
If you have questions about your Medicare home health care benefits or coverage and you have Original Medicare, visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) . TTY users can call 1-877-486-2048. If you get your Medicare benefits through a Medicare Advantage Plan (Part C) or other
What happens when home health services end?
When all of your covered home health services are ending, you may have the right to a fast appeal if you think these services are ending too soon. During a fast appeal, an independent reviewer called a Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) looks at your case and decides if you need your home health services to continue.
What is an appeal in Medicare?
Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
Why is home health important?
In general, the goal of home health care is to provide treatment for an illness or injury. Where possible, home health care helps you get better, regain your independence, and become as self-sucient as possible. Home health care may also help you maintain your current condition or level of function, or to slow decline.
Can Medicare take home health?
In general, most Medicare-certified home health agencies will accept all people with Medicare . An agency isn’t required to accept you if it can’t meet your medical needs. An agency shouldn’t refuse to take you because of your condition, unless the agency would also refuse to take other people with the same condition.
What Is In-Home Care?
In-home care (also known as “home health care”) is a service covered by Medicare that allows skilled workers and therapists to enter your home and provide the services necessary to help you get better.
What Parts Of In-Home Care Are Covered?
In-home care can cover a wide range of services, but they’re not all covered by Medicare. According to the Medicare site, the in-home care services covered by parts A and B include:
How To Get Approved For In-Home Care
There are a handful of steps and qualifications you need to meet to have your in-home care covered by Medicare. It starts with the type of help your doctor says you or your loved one needs and includes other aspects of care.
Cashing In On In-Home Care
Once you qualify for in-home care, it’s time to find the right agency who will provide you or your loved one services. The company you receive your services from is up to you, but they must be approved by Medicare in order for their services to be covered.
How To Pay for In-Home Care Not Covered By Medicare
There may be times when not every part of your in-home care is covered. We already know 20 percent of the durable medical equipment needed to treat you is your responsibility, but there are other services like custodial care or extra round-the-clock care that won’t be covered by Medicare. This is where supplemental insurance (Medigap) comes in.
How long does it take for Medicare to pay for home health?
You also must receive home health services within 14 days of your hospital or SNF discharge to be covered under Part A. Any additional days past 100 are covered by Part B. Regardless of whether your care is covered by Part A or Part B, Medicare pays the full cost.
How many days of home health care do you have to be in a hospital?
Specifically, if you spend at least three consecutive days as a hospital inpatient or have a Medicare-covered SNF stay, Part A covers your first 100 days of home health care. You still must meet other home health care eligibility requirements, such as being homebound and needing skilled care. You also must receive home health services within 14 ...
Is home health insurance deductible or coinsurance?
There is no prior hospital stay requirement for Part B coverage of home health care. There is also no deductible or coinsurance for Part B-covered home health care. While home health care is normally covered by Part B, ...
What is Medicare Part A?
Medicare Part A is the portion that provides hospital coverage. Medicare Part A is free to most individuals when they or their spouse worked for at least 40 quarters paying Medicare taxes.
Who must review home health care plans?
You must be under the care of a doctor who has created a plan for you that involves home health care. Your doctor must review the plan at regular intervals to make sure it is still helping you. Your doctor must certify that you need skilled nursing care and therapy services.
What is the difference between home health and skilled nursing?
The difference is that, for reimbursement, you must be getting skilled nursing services as well.
How to qualify for home health care?
Ideally, home health can enhance your care and prevent re-admission to a hospital. There are several steps and conditions to qualify for home health care: 1 You must be under the care of a doctor who has created a plan for you that involves home health care. Your doctor must review the plan at regular intervals to make sure it is still helping you. 2 Your doctor must certify that you need skilled nursing care and therapy services. To need this care, your doctor must decide that your condition will improve or maintain through home health services. 3 Your doctor must certify that you are homebound. This means it is very difficult or medically challenging for you to leave your home.
What is home health aide?
Home health aides are health professionals who help people in their home when they have disabilities, chronic illnesses, or need extra help. Aides may help with activities of daily living, such as bathing, dressing, going to the bathroom, or other around-the-home activities. For those who need assistance at home, home health aides can be invaluable.
Is long term care insurance part of Medicare?
Some people choose to purchase separate long-term care insurance, which isn’t a part of Medicare . These policies may help to cover more home health care services and for longer time periods than Medicare. However, the policies vary and do represent an extra cost to seniors.
Does Medicare cover home health?
Medicare covers some aspects of these home health services, including physical and occupational therapy as well as skilled nursing care. However, Medicare doesn’t cover all home health services, such as around-the-clock care, meal delivery, or custodial care — many of these services fall under those of a home health aide.
What is the CPT code for home visits?
Home visits services ( CPT codes 99341-99350) may only be billed when services are provided in beneficiary's private residence ( POS 12). To bill these codes, physician must be physically present in beneficiary's home.
What is a home visit?
Home and domiciliary visits are when a physician or qualified non-physician practitioner (NPPs) oversee or directly provide progressively more sophisticated evaluation and management (E/M) visits in a beneficiary's home. This is to improve medical care in a home environment. A provider must be present and provide face to face services. This is not to be confused with home healthcare incident to services.
What is a domiciliary care facility?
Domiciliary Care Facility - A home providing mainly custodial and personal care for persons who do not require medical or nursing supervision, but may require assistance with activities of daily living because of a physical or mental dis ability. This may also be referred to as a sheltered living environment.
What are the modalities of home and domiciliary visits?
Modalities. Home and domiciliary visits require complex or multidisciplinary care modalities involving: Beneficiaries seen may be disabled either physically or mentally making access to a traditional office visit very difficult, or may have limited support systems.
Can a home health provider perform a NPP on the same day?
There may be circumstances where home health services and services of physician/qualified non-physician practitioners (NPPs) are performed on same day. These services cannot be duplicative or overlapping.
Is home health covered by Medicare Part B?
Based on Consolidative Billing Regulations, no service will be covered under Medicare Part B when performed only to provide supervision for a visiting nurse/home health agency visit (s) If a beneficiary is receiving care under home health benefit, primary treating physician will be working in concert with home health agency.
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This First Coast Billing and Coding Article for Local Coverage Determination (LCD) L33817 E&M Home and Domiciliary Visits provides billing and coding guidance for frequency limitations as well as diagnosis limitations that support diagnosis to procedure code automated denials.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10-CM Codes that are covered” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What if my ER visit isn't covered by Medicare?
If your ER visit isn’t covered under Medicare Part A, you may be able to get coverage through Medicare Part B, C, D, or Medigap, depending on your specific plan. Read on to learn more about Part A coverage for ER visits, including what may or may not be covered, and other coverage options you may have. Share on Pinterest.
How long do you have to be in the hospital for Medicare Part A?
Most of the time, you have to be admitted as an inpatient for two consecutive midnights for Medicare Part A to cover your visit. If a doctor admits you to the hospital following an ER visit and you stay in the hospital for two midnights or longer, Medicare Part A pays for your inpatient hospital stay plus the outpatient costs from your ER visit.
How many people go to the emergency room every year?
The Centers for Disease Control and Prevention (CDC) Trusted Source. estimates that 145 million people visit the emergency room every year, with a little more than 12.5 million of them being admitted to the hospital for inpatient care as a result.
What are the services that are available at the ER?
You may receive several different kinds of services you may need during an ER visit, including: emergency examination by one or more physicians. lab tests. X-rays. scans or screenings. medical or surgical procedures. medical supplies and equipment, like crutches. medications.
Does Medicare cover ambulances?
Takeaway. Medicare Part A is sometimes called “hospital insurance,” but it only covers the costs of an emergency room (ER) visit if you’re admitted to the hospital to treat the illness or injury that brought you to the ER.
Does Medicare pay for ER visits?
The good news is that Medicare Part B (medical insurance) generally pays for your ER visits whether you’ve been hurt, you develop a sudden illness, or an illness takes a turn for the worse.
Can you take medication at home while in the ER?
However, if you need medication that you usually take at home and it’s given by the hospital while in the ER, that’s considered a self-administered drug. If the medication you’re given is on your Medicare Part D drug list, Part D may pay for that medication.
