
What caregiving costs and services will Medicare cover?
Medicare doesn’t cover long-term care (also called custodial care) if that's the only care you need. Most nursing home care is custodial care, which is care that helps you with daily living activities (like bathing, dressing, and using the bathroom).
How to reduce the cost of long term care insurance?
Mar 09, 2021 · Does Medicare pay for long-term care? Original Medicare (Part A and Part B) covers some hospital and medical costs. Medicare Part D covers some prescription drugs. Medicare generally doesn’t cover long-term care except in certain circumstances.
How much long term care insurance coverage do I Need?
Long-term care hospitals specialize in treating patients with more than 1 serious medical condition who are hospitalized for 25 days or more. The patients may improve with time and care, and eventually return home. Long-term care hospitals typically give services like respiratory therapy, hea d trauma treatment, and pain management.
What should I know about long term care insurance?
Medicare will pay for medical social services, home health aide services, medical supplies, and durable medical equipment used in the home for qualifying patients. However, custodial home health care is not covered by Medicare. Medigap Does Not Pay For Long-Term Care. Medigap plans, like Medicare, only cover a portion of long-term care services.
What is the difference between Parts A and B of Medicare coverage?
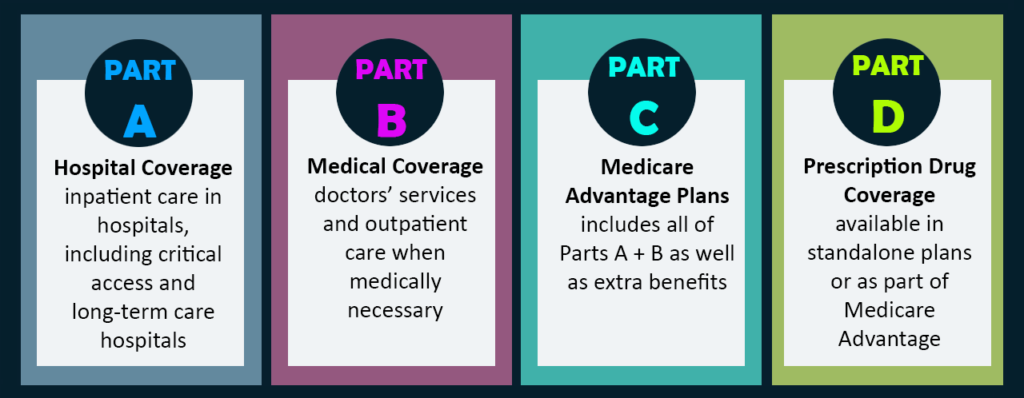
Medicare Part A and Medicare Part B are two aspects of healthcare coverage the Centers for Medicare & Medicaid Services provide. Part A is hospital coverage, while Part B is more for doctor's visits and other aspects of outpatient medical care.
What do the three parts of Medicare cover?
Part A provides inpatient/hospital coverage. Part B provides outpatient/medical coverage. Part C offers an alternate way to receive your Medicare benefits (see below for more information). Part D provides prescription drug coverage.
What is the difference between Medicare Part C and Part D?
Medicare part C is called "Medicare Advantage" and gives you additional coverage. Part D gives you prescription drug coverage.
What is Medicare Part B also known as?
Medicare Part B (also known as medical insurance) is an insurance plan that covers medical services related to outpatient and doctor care.
What is long term care hospital?
A long-term care hospital (generally you won’t pay more than you would pay for care in an acute care hospital) Skilled nursing facility (Medicare covered services include a semi-private room, meals, skilled nursing care and medications) Eligible home health services such as physical therapy and speech-language pathology.
How much will Medicare pay for long term care in 2021?
In 2021 under Medicare Part A, you generally pay $0 coinsurance for the first 60 days of each benefit period, once you have paid your Part A deductible.
What is Medicare Part D?
Original Medicare (Part A and Part B) covers some hospital and medical costs. Medicare Part D covers some prescription drugs. Medicare generally doesn’t cover long-term care except in certain circumstances. Medicare draws a line between medical care (which is generally covered) and what it calls “custodial care” which is generally not covered. Custodial care includes help bathing, eating, going to the bathroom, and moving around. However, Medicare may cover long-term care that you receive in: 1 A long-term care hospital (generally you won’t pay more than you would pay for care in an acute care hospital) 2 Skilled nursing facility (Medicare covered services include a semi-private room, meals, skilled nursing care and medications) 3 Eligible home health services such as physical therapy and speech-language pathology 4 Hospice care including nursing care, prescription drugs, hospice aid and homemaker services
How much is the Medicare deductible for 2021?
The deductible is $1,484 in 2021. Feel free to click the Compare Plans button to see a list of plan options in your area you may qualify for.
How much does a coinsurance policy cost for 61-90?
For days 61-90, you pay $371 per day of each benefit period. For days 91 and beyond you pay $742 coinsurance per each “lifetime reserve day” after day 90 for each benefit period and you only have up to 60 days over your lifetime. Beyond the lifetime reserve days you pay all costs until a new benefit period begins.
Why do seniors need long term care?
Chronic conditions such as diabetes and high blood also make you more likely to need long-term care. Alzheimer’s and dementia are very common among seniors and may be another reason to need long-term care. According to the Alzheimer’s foundation, one in three seniors dies with Alzheimer’s or another dementia.
Do you need long term care if you fall?
According to the U.S. Department of Health and Human Services, the need for long-term care often follows a fall. Preventing falls may delay your need for long-term care. Learn more about how to prevent falling. Chronic conditions such as diabetes and high blood also make you more likely to need long-term care.
What is Medicare Part A?
Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. covers the cost of long-term care in a. long-term care hospital. Acute care hospitals that provide treatment for patients who stay, on average, more than 25 days.
How long does an acute care hospital stay?
Acute care hospitals that provide treatment for patients who stay, on average, more than 25 days. Most patients are transferred from an intensive or critical care unit. Services provided include comprehensive rehabilitation, respiratory therapy, head trauma treatment, and pain management. .
When does the benefit period end?
The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins. ...
How long does it take to get discharged from a long term care hospital?
You’re transferred to a long-term care hospital directly from an acute care hospital. You’re admitted to a long-term care hospital within 60 days of being discharged from a hospital.
Do you have to pay a deductible for long term care?
Each day after the lifetime reserve days: All costs. *You don’t have to pay a deductible for care you get in the long-term care hospital if you were already charged a deductible for care you got in a prior hospitalization within the same benefit period.
Does Medicare Pay For A Skilled Nursing Facility?
Medicare does not cover the full amount of time in a skilled nursing facility beyond what is required by its regulations. Medicare covers SNF care as follows:
Does Medicare Pay For Home Health Care Coverage?
Medicare covers the expenses of having an agency give part-time or intermittent health care services in the patient’s home, but this coverage is limited, and the patient must need skilled assistance. The following conditions must be met to qualify for Medicare’s home health care benefit:
Medigap Does Not Pay For Long-Term Care
Medigap plans, like Medicare, only cover a portion of long-term care services. Medigap policies are meant to fill in the gaps in Medicare caused by the numerous deductibles, co-payments, and other similar restrictions. These plans strive to fill in where Medicare leaves off.
How To Pay For Long-Term Care At A Fraction Of The Cost
A long-term care annuity is a hybrid annuity that is set up to assist in paying for various long-term care services and facilities without causing retirement funds to be depleted. To create a tax-free long-Term Care Insurance benefit, an LTC annuity doubles (200%) or triples (300%) the investment (based on medical records).
How much does Medicare pay for skilled nursing?
If you qualify for short-term coverage in a skilled nursing facility, Medicare pays 100 percent of the cost — meals, nursing care, room, etc. — for the first 20 days. For days 21 through 100, you bear the cost of a daily copay, which was $170.50 in 2019.
How long does Medicare pay for a stroke?
If you’re enrolled in original Medicare, it can pay a portion of the cost for up to 100 days in a skilled nursing facility.
What is the 3 day rule for Medicare?
Two more things to note about the three-day rule: Medicare Advantage plans, which match the coverage of original Medicare and often provide additional benefits, often don’t have those same restrictions for enrollees. Check with your plan provider on terms for skilled nursing care.
Does Medicare cover nursing homes?
Under specific, limited circumstances, Medicare Part A, which is the component of original Medicare that includes hospital insurance, does provide coverage for short-term stays in skilled nursing facilities, most often in nursing homes.
Does Medicare cover long term care?
Of course, Medicare covers medical services in these settings. But it does not pay for a stay in any long-term care facilities or the cost of any custodial care (that is, help with activities of daily life, such as bathing, dressing, eating and going to the bathroom), except for very limited circumstances when a person receives home health services ...
Does observation count as time spent in a skilled nursing facility?
In both cases you are lying in a hospital bed, eating hospital food and being attended to by hospital doctors and nurses. But time spent under observation does not count toward the three-day requirement for Medicare coverage in a skilled nursing facility.
Does long term care insurance pay for veterans?
Long-term care insurance: Some people have long-term care insurance that might pay, depending on the terms of their policies. The VA: Military veterans may have access to long-term care benefits from the U.S. Department of Veterans Affairs.
What to do if you need long term care?
You may have other long-term care options (besides nursing home care) available to you. Talk to your family, your doctor or other health care provider, a person-centered counselor, or a social worker for help deciding what kind of long-term care you need. Before you make any decisions about long term care, talk to someone you trust ...
What is the program of all inclusive care for the elderly?
PACE (Program of All-inclusive Care for the Elderly) is a Medicare/Medicaid program that helps people meet health care needs in community. Learn more about PACE. Note. Visit LongTermCare.gov for information and resources to help you and your family plan for future long-term care needs.
What is hospice care?
Hospice is a program of care and support for people who are terminally ill. Hospice helps people who are terminally ill live comfortably. The focus is on comfort, not on curing an illness. Respite care is a very short inpatient stay given to a hospice patient so that their usual caregiver can rest.
What is an ADU in a house?
Accessory Dwelling Unit (ADU) An ADU (sometimes called an "in-law apartment," "accessory apartment," or a "second unit") is a second living space within a home or on a lot. It has a separate living and sleeping area, a place to cook, and a bathroom.
What are some examples of services and programs that may be available in your community?
Examples of the services and programs that may be available in your community are: Adult day services. Adult day health care (which offers nursing and therapy) Care coordination and case management (including transition services to leave a nursing home)
What is a person centered counselor?
A person-centered counselor. A social worker. If you’re in a hospital, nursing home, or working with a home health agency (HHA), you can get support to help you understand your options or help you arrange care. Talk to: A discharge planner. A social worker.
What is subsidized senior housing?
Subsidized senior housing. There are state and federal programs that help pay for housing for some seniors with low to moderate incomes. Some of these housing programs also offer help with meals and other activities, like housekeeping, shopping, and doing the laundry.

Some Short-Term Stays Qualify
- Under specific, limited circumstances, Medicare Part A, which is the component of original Medicare that includes hospital insurance, does provide coverage for short-term stays in skilled nursing facilities, most often in nursing homes. Your doctor might send you to a skilled nursing facility for specialized nursing care and rehabilitation after a hospital stay. If you had a stroke or …
What’s A ‘Qualifying Hospital Stay’?
- Another important rule: You must have had a “qualifying hospital stay,” meaning you were formally admitted as an inpatient to the hospital for at least three consecutive days. You cannot have been in “observation” status. In both cases you are lying in a hospital bed, eating hospital food and being attended to by hospital doctors and nurses. But time spent under observation does not co…
Who Pays For Long-Term Care?
- Medicare doesn’t pay anything toward the considerable cost of staying in a nursing home or other facility for long-term care. So who or what does? Here are some options. 1. Private pay:Many individuals and families simply pay out of pocket or tap assets such as property or investments to finance their own or a loved one’s nursing home care. If they use up those resources, Medicaid …