How does Medicare reimburse a hospital?
You may think that the hospital simply sends Medicare a bill; however, the reimbursement process is actually much more intricate. What Part of Medicare Provides Coverage for Hospital Treatment? If you receive care as an inpatient in a hospital, Medicare Part A will help to provide coverage for care.
Does Medicare Part a cover hospital care?
Learn about Medicare Part A coverage for inpatient hospital, skilled nursing facility (SNF), and long-term hospital care. Medicare Part A coverage–hospital care | Medicare Skip to main content Home What Medicare covers
What does Medicare pay for inpatient hospital stays?
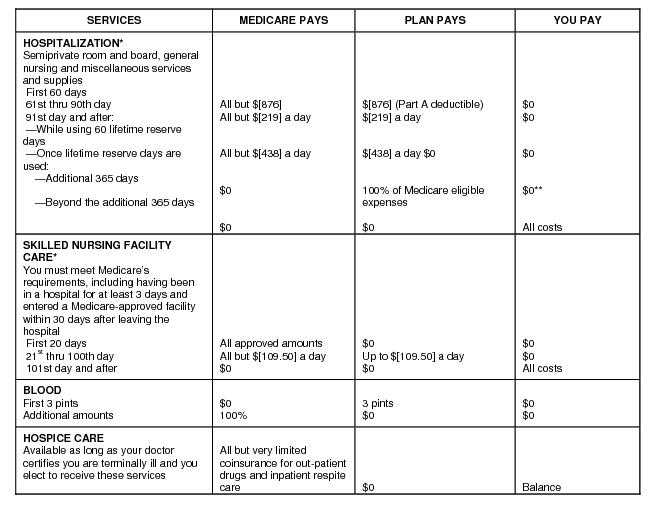
Medicare pays for inpatient hospital stays of a certain length. Medicare covers the first 60 days of a hospital stay after the person has paid the deductible. The exact amount of coverage that Medicare provides depends on how long the person stays in the hospital or other eligible healthcare facility.
What does Medicare Part a pay for?
If admitted into a hospital, Medicare Part A will help pay for: 1 the hospital room 2 nursing services 3 meals 4 medications 5 medical supplies 6 durable medical equipment used while in hospital care, like wheelchairs, walkers, and crutches 7 diagnostic testing 8 rehabilitation services provided while an inpatient
Which part of Medicare coverage would pay for hospitalizations?
Part APart A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
Does Medicare Part A pay 100 of hospitalization?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
Which part of Medicare covers both inpatient and outpatient?
Part BPart A provides inpatient/hospital coverage. Part B provides outpatient/medical coverage. Part C offers an alternate way to receive your Medicare benefits (see below for more information). Part D provides prescription drug coverage.
How does Medicare Part A pay hospitals?
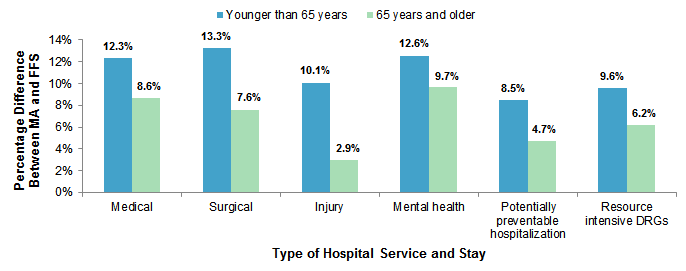
Inpatient hospitals (acute care): Medicare pays hospitals per beneficiary discharge, using the Inpatient Prospective Payment System. The base rate for each discharge corresponds to one of over 700 different categories of diagnoses—called Diagnosis Related Groups (DRGs)—that are further adjusted for patient severity.
What is the difference between Part C and Part D Medicare?
Medicare Part C and Medicare Part D. Medicare Part D is Medicare's prescription drug coverage that's offered to help with the cost of medication. Medicare Part C (Medicare Advantage) is a health plan option that's similar to one you'd purchase from an employer.
What is the difference between Medicare Part A and B?
If you're wondering what Medicare Part A covers and what Part B covers: Medicare Part A generally helps pay your costs as a hospital inpatient. Medicare Part B may help pay for doctor visits, preventive services, lab tests, medical equipment and supplies, and more.
What is Medicare Part C used for?
Medicare Part C covers the inpatient care typically covered by Medicare Part A. If you are a Medicare Part C subscriber and are admitted to the hospital, your Medicare Advantage plan must cover a semi-private room, general nursing care, meals, hospital supplies, and medications administered as part of inpatient care.
What does Medicare Part D include?
The Medicare Part D program provides an outpatient prescription drug benefit to older adults and people with long-term disabilities in Medicare who enroll in private plans, including stand-alone prescription drug plans (PDPs) to supplement traditional Medicare and Medicare Advantage prescription drug plans (MA-PDs) ...
What is Medicare Part B known as?
Medicare Part B (medical insurance) is part of Original Medicare and covers medical services and supplies that are medically necessary to treat your health condition. This can include outpatient care, preventive services, ambulance services, and durable medical equipment.
Does Medicare cover hospital stay?
Medicare generally covers 100% of your medical expenses if you are admitted as a public patient in a public hospital. As a public patient, you generally won't be able to choose your own doctor or choose the day that you are admitted to hospital.
How many days will Medicare pay for hospital stay?
90 daysMedicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.
What is not covered under Medicare Part A?
Medicare Part A will not cover long-term care, non-skilled, daily living, or custodial activities. Certain hospitals and critical access hospitals have agreements with the Department of Health & Human Services that lets the hospital “swing” its beds into (and out of) SNF care as needed.
What are Medicare covered services?
Medicare-covered hospital services include: Semi-private rooms. Meals. General nursing. Drugs as part of your inpatient treatment (including methadone to treat an opioid use disorder) Other hospital services and supplies as part of your inpatient treatment.
What does Medicare Part B cover?
If you also have Part B, it generally covers 80% of the Medicare-approved amount for doctor’s services you get while you’re in a hospital. This doesn't include: Private-duty nursing. Private room (unless Medically necessary ) Television and phone in your room (if there's a separate charge for these items)
What is an inpatient hospital?
Inpatient hospital care. You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury. The hospital accepts Medicare.
What is Medicare Part A?
Medicare Part A, the first part of original Medicare, is hospital insurance. It typically covers inpatient surgeries, bloodwork and diagnostics, and hospital stays. If admitted into a hospital, Medicare Part A will help pay for:
How much does Medicare Part A cost in 2020?
In 2020, the Medicare Part A deductible is $1,408 per benefit period.
How long does Medicare Part A deductible last?
Unlike some deductibles, the Medicare Part A deductible applies to each benefit period. This means it applies to the length of time you’ve been admitted into the hospital through 60 consecutive days after you’ve been out of the hospital.
How many days can you use Medicare in one hospital visit?
Medicare provides an additional 60 days of coverage beyond the 90 days of covered inpatient care within a benefit period. These 60 days are known as lifetime reserve days. Lifetime reserve days can be used only once, but they don’t have to be used all in one hospital visit.
What is the Medicare deductible for 2020?
Even with insurance, you’ll still have to pay a portion of the hospital bill, along with premiums, deductibles, and other costs that are adjusted every year. In 2020, the Medicare Part A deductible is $1,408 per benefit period.
How long do you have to work to qualify for Medicare Part A?
To be eligible, you’ll need to have worked for 40 quarters, or 10 years, and paid Medicare taxes during that time.
Does Medicare cover hospital stays?
Medicare Part A can help provide coverage for hospital stays. You’ll still be responsible for deductibles and coinsurance. A stay at the hospital can make for one hefty bill. Without insurance, a single night there could cost thousands of dollars. Having insurance can help reduce that cost.
When a patient uses Medicare as their primary insurance company, is the hospital required to choose appropriate and accurate diagnoses that
When a patient uses Medicare as their primary insurance company, the hospital is required to choose appropriate and accurate diagnoses that apply to the patient so that they can bill for the associated care.
What is Medicare insurance?
Medicare insurance is one of the most popular options for those who qualify, and the number of people using this insurance continues to grow as life expectancy continues to increase. Medicare policies come available with many different parts, including Part A, Part B, Part C, and Part D.
How long do you have to pay coinsurance for hospital?
As far as out-of-pocket costs, you will be responsible for paying your deductible, coinsurance payments if your hospital stay is beyond 60 days, and for any care that is not deemed medically necessary. However, the remainder of the costs will be covered by your Medicare plan.
Does Medicare pay flat rate?
This type of payment system is approved by the hospitals and allows Medicare to pay a simple flat rate depending on the specific medical issues a patient presents with and the care they require. In addition, In some cases, Medicare may provide increased or decreased payment to some hospitals based on a few factors.
Does Medicare cover inpatient care?
If you receive care as an inpatient in a hospital, Medicare Part A will help to provide coverage for care. Part A Medicare coverage is responsible for all inpatient care , which may include surgeries and their recovery, hospital stays due to illness or injury, certain tests and procedures, and more. As far as out-of-pocket costs, you will be ...
What is partial hospitalization?
Partial hospitalization provides a structured program of outpatient psychiatric services as an alternative to inpatient psychiatric care. It’s more intense than care you get in a doctor’s or therapist’s office. You get this treatment during the day, and you don't have to stay overnight.
What is assignment in Medicare?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. . You also pay. coinsurance.
What is coinsurance in hospital?
coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%). for each day of partial hospitalization services you get in a hospital outpatient setting or community mental health center, and the Part B.
What is original Medicare?
Your costs in Original Medicare. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
Does Medicare cover meals?
. Medicare doesn't cover: Meals.
Does Medicare cover partial hospitalization?
Individual patient training and education about your condition. Medicare only partial hospitalization coverage only applies if the doctor and the program accept. assignment.
What's covered?
If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain facilities or for patients with certain conditions.
2 ways to find out if Medicare covers what you need
Talk to your doctor or other health care provider about why you need certain services or supplies. Ask if Medicare will cover them. You may need something that's usually covered but your provider thinks that Medicare won't cover it in your situation. If so, you'll have to read and sign a notice.
What is covered by Medicare before a hospital stay?
This coverage includes: general nursing care. a semi-private room. hospital equipment and services. meals. medication that is part of inpatient hospital treatment.
What is Medicare Part A?
Medicare Part A. Out-of-pocket expenses. Length of stay. Eligible facilities. Reducing costs. Summary. Medicare is the federal health insurance program for adults aged 65 and older, as well as for some younger people. Medicare pays for inpatient hospital stays of a certain length. Medicare covers the first 60 days of a hospital stay after ...
What is the best Medicare plan?
We may use a few terms in this piece that can be helpful to understand when selecting the best insurance plan: 1 Deductible: This is an annual amount that a person must spend out of pocket within a certain time period before an insurer starts to fund their treatments. 2 Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. 3 Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
How much does Medicare pay for skilled nursing in 2020?
Others, who may have long-term cognitive or physical conditions, require ongoing supervision and care. Medicare Part A coverage for care at a skilled nursing facility in 2020 involves: Day 1–20: The patient spends $0 per benefit period after meeting the deductible. Days 21–100: The patient pays $176 per day.
How much is the deductible for Medicare 2020?
This amount changes each year. For 2020, the Medicare Part A deductible is $1,408 for each benefit period.
How long does Medicare cover hospital stays?
Medicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual’s reserve days. Medicare provides 60 lifetime reserve days. The reserve days provide coverage after 90 days, but coinsurance costs still apply.
How long does a psychiatric hospital stay in Medicare?
Medicare provides the same fee structure for general hospital care and psychiatric hospital care, with one exception: It limits the coverage of inpatient psychiatric hospital care to 190 days in a lifetime.
Does Medicare Cover Ambulance Services
Medicare will pay for ambulance services under specific circumstances, but it’s important to know what these are to avoid hefty bills.
Figuring Out How Much Money A Hospital Gets Paid For A Given Drg
In order to figure out how much a hospital gets paid for any particular hospitalization, you must first know what DRG was assigned for that hospitalization.
Does Medicare Cover Treatment For Covid
Patients who get seriously ill from the virus may need a variety of inpatient and outpatient services. Medicare covers inpatient hospital stays, skilled nursing facility stays, some home health visits, and hospice care under Part A.
Hospital Stay Coverage Under Medicare Advantage
You may choose to receive your Medicare Part A and Part B coverage through a local Medicare Advantage plan. Medicare Advantage plans are offered by private insurance companies that are approved by Medicare and cover at least the same level of benefits as Original Medicare Part A and Part B .
Examples Of How Er Costs Vary Among Medicare Advantage Plans
The way a Medicare Advantage plan bills you for a trip to the ER and how much you owe can vary from plan to plan.
When Can You Sign Up For Medicare Part A
Medicare Part A enrollment comes with a seven-month Initial Enrollment Period for signup. This includes the three months before and after the month you turn 65, plus the month of your birthday. For instance, if you turn 65 in April, your Initial Enrollment Period stretches from January through July. 13
What Happens If Medicare Beneficiaries In Private Plans Need To Receive Care From Out
Plans that provide Medicare-covered benefits to Medicare beneficiaries, including stand-alone prescription drug plans and Medicare Advantage plans, typically have provider networks and limit the ability of enrollees to receive Medicare-covered services from out-of-network providers, or charge enrollees more when they receive services from out-of-network providers or pharmacies.
What is partial hospitalization?
Eligibility. Takeaway. Partial hospitalization is an intensive outpatient program to help treat substance abuse or mental health conditions. Medicare will pay for this program when it’s provided by a Medicare-approved facility and is necessary for your recovery. Your costs will vary depending on the specific program and on your Medicare plan.
What is Medicare approved amount?
The Medicare-approved amount is a set amount for treatment that a facility has agreed to accept from Medicare as payments. It’s often lower than the price you’d pay without insurance at all. So, not only are you only responsible for 20 percent, you’re responsible for 20 percent of a lower total amount.
How much is Medicare Part B 2021?
When you use Medicare Part B, you’ll first need to meet your yearly deductible. In 2021 the deductible is $203. Once you meet the deductible, you’ll pay a coinsurance of 20 percent of the Medicare-approved cost of your treatment and Medicare will pay the other 80 percent.
Is Medicare Part B covered by Medicare Advantage?
Any prescriptions administered to you while you’re at the facility of your partial hospitalization program will be covered under Medicare Part B or your Medicare Advantage plan. If you need to take any prescriptions at home, you’ll need a separate prescription drug plan.
Does Medicare cover partial hospitalization?
Medicare will cover parti al hospitalization as long as it meets certain requirements. In order to be covered you’ll need to: receive your care at a Medicare-approved facility. receive your care under the supervision of a licensed physician.
Does Medicare cover intensive care?
During the day, you’ll receive intensive therapy under the care of licensed professionals. Medicare will provide coverage if you need this level of care, although your costs will vary depending on your Medicare plan and the facility where you receive treatment. Share on Pinterest. Justin Paget/Getty Images.
Does Medicare Part D cover prescriptions?
Medicare Part D is stand-alone prescription coverage and will cover any prescriptions you need to take at home. A Medicare supplement (Medigap) plan can also help cover some of your treatment. Medigap plans help you cover the out-of-pocket costs of using original Medicare, such as copayments and deductibles.