Part B of Medicare is intended to fill some of the gaps in medical insurance coverage left under Part A. After the beneficiary meets the annual deductible, Part B will pay 80% of the “reasonable charge” for covered services, the reimbursement rate determined by Medicare; the beneficiary is responsible for the remaining 20% as “co-insurance.”
What services are covered by Medicare Part A and B?
Services Covered by Medicare Part A & Part B. Medicare covers many tests, items and services like lab tests, surgeries, and doctor visits – as well as supplies, like wheelchairs and walkers. In general, Part A covers things like hospital care, skilled nursing facility care, hospice, and home health services.
How does Medicare Part B billing work?
An important thing to understand about Medicare Part B billing is that each person must pay a premium each month, and pay a yearly deductible and copay. As such, Part B is a lot like regular commercial insurance plans.
Should part B hospital services be billable to Medicare?
Hospitals have expressed concern about Medicare’s policy, arguing that all Part B hospital services provided should be billable to Medicare because they would have been reasonable and necessary if the beneficiary had been treated as an outpatient and not as an inpatient.
What does Part B of the Medicare card cover?
Part B covers things like: Clinical research Ambulance services Durable medical equipment (DME) Mental health Inpatient Getting a second opinion before surgery Limited outpatient prescription drugs
What part of the bill for services is the patient covered by Medicare Part B?
A more detailed description of services covered for beneficiaries in a Part B stay is found at §10.1 – Billing for Inpatient Services Paid Under Part B.
What is Medicare Part B responsible for?
For most services, Part B medical insurance pays only 80% of what Medicare decides is the approved charge for a particular service or treatment. You are responsible for paying the other 20% of the approved charge, called your coinsurance amount.
What is billed under Part B?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services. Part B also covers some preventive services.
Which of the following services are covered by Medicare Part B quizlet?
Part B helps cover medically-necessary services like doctors' services, outpatient care, durable medical equipment, home health services, and other medical services.
Is Medicare Part B fee for service?
Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles).
How do I bill for Medicare services?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Which of the following is not covered under Part B of a Medicare policy?
But there are still some services that Part B does not pay for. If you're enrolled in the original Medicare program, these gaps in coverage include: Routine services for vision, hearing and dental care — for example, checkups, eyeglasses, hearing aids, dental extractions and dentures.
How do I bill Medicare Part B for inpatient claims?
Hospitals must bill Part B inpatient services on a 12x Type of Bill. This Part B inpatient claim is subject to the statutory time limit for filing Part B claims described in the Medicare Claims Processing Manual, Chapter 1, Section 70.
What expenses will Medicare Part B pay quizlet?
part b covers doctor services no matter where recieved in the united states. covered doctor services include surgical services, diagnostic tests and x rays that are part of the treatment, medical supplies furnished in a doctors office, and services of the office nurse. You just studied 9 terms!
Which of the following services would not be covered under Medicare Part B quizlet?
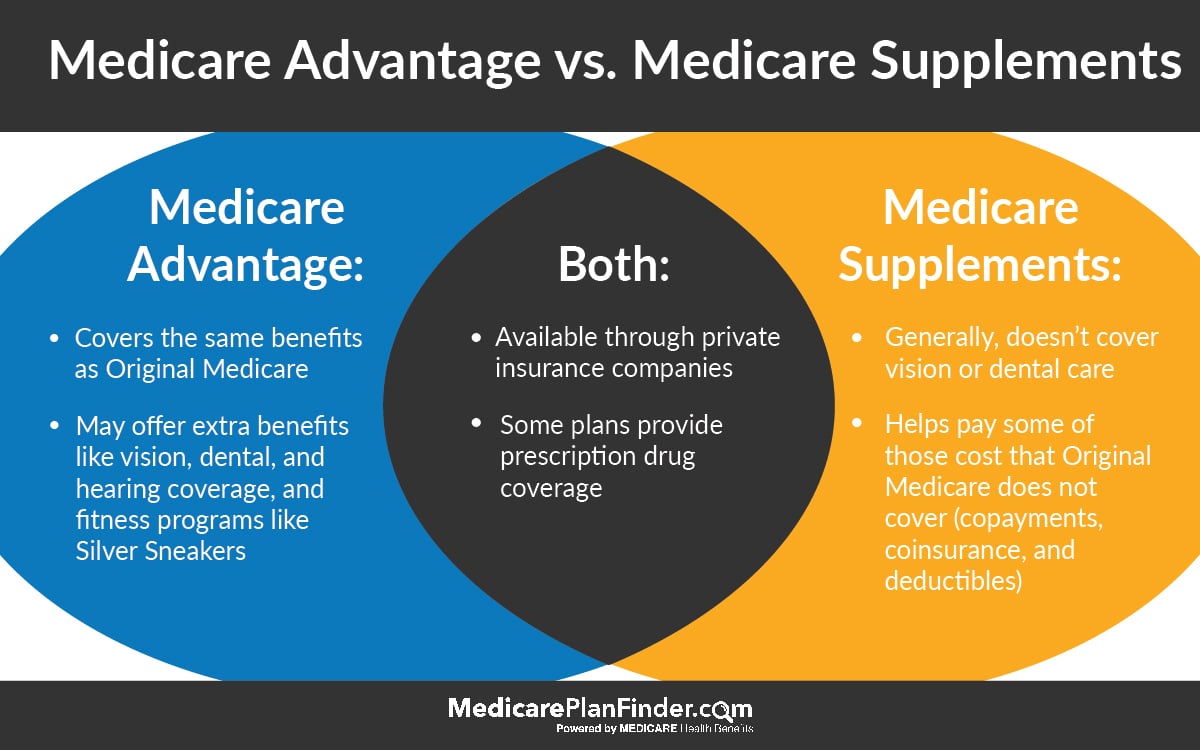
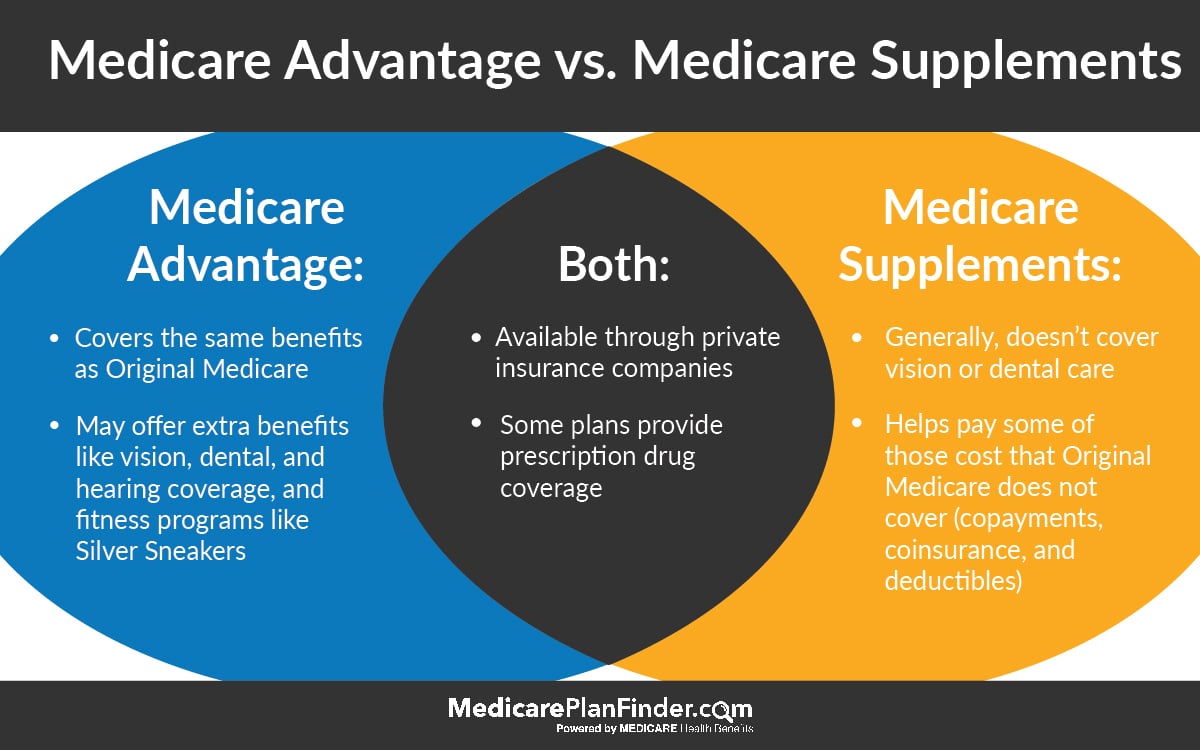
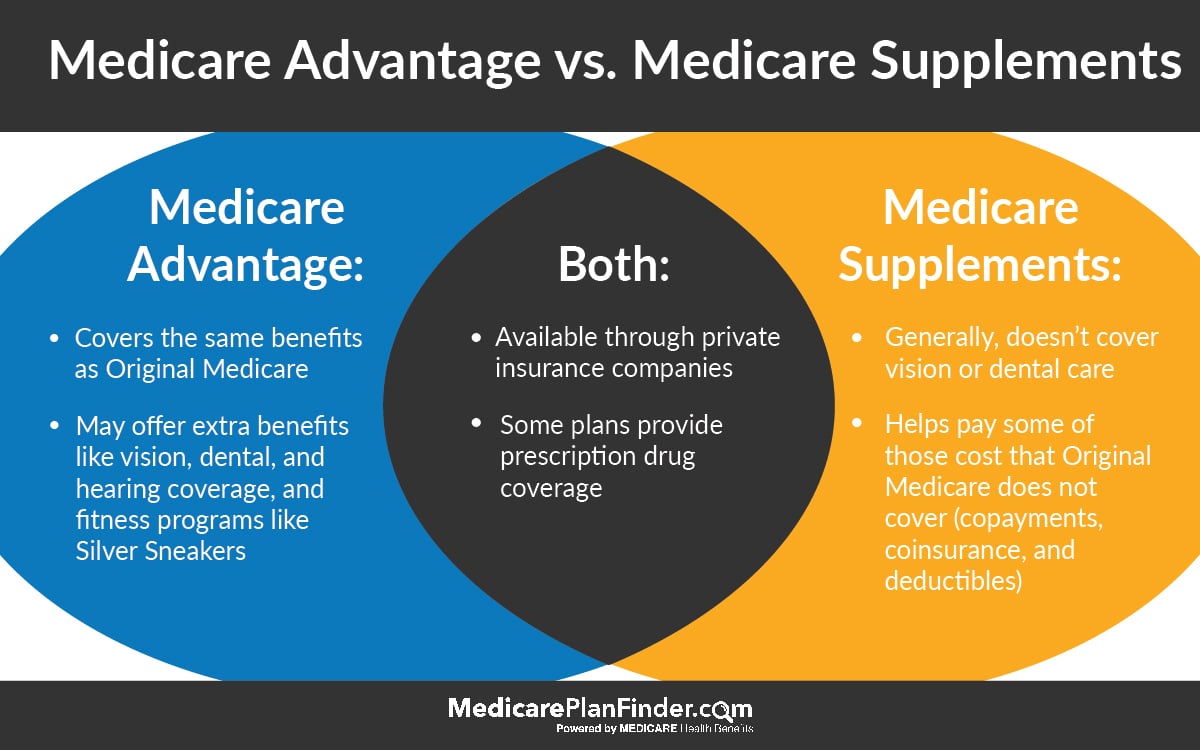
Which of the following is not covered by Medicare Part B? Medicare Part B covers outpatient services, rehab services, medical equipment (but not adaptive equipment), diagnostic tests, and preventative care. Eye, hearing and dental services are not covered by any part of Medicare and require supplemental insurance.
Which of the following preventive services are provided under Medicare Part B quizlet?
Medicare Part B covers an annual "wellness" preventive care visit during which the insured and the provider can develop or update a personalized plan for disease prevention. Clinical laboratory services, including blood tests, urinalysis, and some screening tests, are also covered for long-term nursing home residents.
Which of the following is Medicare Part B also known as?
medical insuranceMedicare Part B (also known as medical insurance) is an insurance plan that covers medical services related to outpatient and doctor care.
Why would Medicare allow additional Part B payments?
Specifically, the proposed rule would allow additional Part B payment when a Medicare Part A claim is denied because the beneficiary should have been treated as an outpatient, rather than being admitted to the hospital as an inpatient. The proposed rule, Medicare Program; Part B Inpatient Billing in Hospitals, proposes that if ...
How long after the date of service can a hospital bill?
Also under current policy, the hospital may only bill for the limited list of Part B inpatient ancillary services and those services must be billed no later than 12 months after the date of service.
What is the reasonable and necessary standard for Medicare?
The “reasonable and necessary” standard is a prerequisite for Medicare coverage in the Social Security Act. The statutory timely filing deadline, under which claims must be filed within 12 months of the date of service, would continue to apply to the Part B inpatient claims. Also on March 13, CMS Acting Administrator Marilyn Tavenner issued an ...
What is CMS 1455?
PROPOSED RULE (CMS-1455-P) AND ADMINISTRATOR RULING (CMS-1455-R) On March 13, 2013, the Centers for Medicare & Medicaid Services (CMS) released a proposed rule that would allow Medicare to pay for additional hospital inpatient services under Medicare Part B. Specifically, the proposed rule would allow additional Part B payment when ...
Does Medicare pay for inpatient services?
Under longstanding Medicare policy, Medicare only pays for a limited number of ancillary medical and other health services as inpatient services under Part B when a Part A claim submitted by a hospital for payment of an inpatient admission is denied as not reasonable and necessary. Hospitals have expressed concern about Medicare’s policy, arguing that all Part B hospital services provided should be billable to Medicare because they would have been reasonable and necessary if the beneficiary had been treated as an outpatient and not as an inpatient.
Does the hospital rule cover self audits?
The Ruling does not cover hospital self-audits or situations where Part A payment cannot be made because the beneficiary has exhausted or is not entitled to Part A benefits. The Ruling only addresses Part A claims denied because the inpatient admission was not reasonable and necessary.
Should Medicare bill Part B?
Hospitals have expressed concern about Medicare’s policy, arguing that all Part B hospital services provided should be billable to Medicare because they would have been reasonable and necessary if the beneficiary had been treated as an outpatient and not as an inpatient. Last year, in response to hospitals’ concerns, ...
What is Medicare Part B for eyeglasses?
Other preventative services are also covered under Medicare Part B: Preventive shots, including the flu shot during flu season, and three Hepatitis B shots, if you're considered at risk.
How long does it take for Medicare to pay Part B?
Like other commercial insurances, you should send Medicare Part B claims directly to Medicare for payment, with an expected turnaround of about 30 days. Unlike typical commercial insurance, Medicare can pay either the provider or the patient, depending on the assignment.
What is CMS in Medicare?
CMS, the Centers for Medicare and Medicaid Services, governs all parts of Medicare, including Part B. CMS holds a great amount of influence over the way insurance companies pay doctors, as well as the services that doctors provide. This is, in large part, because of Medicare Part B restrictions. Every type of healthcare service eligible ...
Why is Medicare important?
Because Medicare is a service provided for the elderly, disabled, and retired, the patients who are covered by Medicare will usually have limited financial resources . Because of this, it's very important to make sure that your office bills and codes within all Part B guidelines and provides only approved Part B services.
What is medically necessary?
Medically Necessary Services: These include services and supplies needed to treat your medical condition. To be covered, the service also has to be within the standards of medical practice. This means that holistic or naturopathic treatments wouldn't be covered.
What are the services that are considered medically necessary?
These services include: Home health services, only when they are medically necessary, and of limited duration. Chiropractic services, only if it is to correct spinal subluxation. Ambulance services, only if a different type of transportation would endanger the patient's health.
What is Part C?
Part C combines Parts A and B (and sometimes D), and is managed by private insurance companies as approved by Medicare. Part D is a prescription drug coverage program which is also managed by private insurance companies as approved by Medicare. Each of these parts provides a different type of coverage, with different limitations ...
What does Medicare cover?
Medicare covers many tests, items and services like lab tests, surgeries, and doctor visits – as well as supplies, like wheelchair s and walkers. In general, Part A covers things like hospital care, skilled nursing facility care, hospice, and home health services. Medicare Part B covers medically necessary services and preventative services.
How many visits does Medicare cover?
Medicare will cover one visit per year with a primary care doctor in a primary care setting (like a doctor’s office) to help lower your risk for cardiovascular disease. During this visit, the doctor may discuss aspirin use (if appropriate), check your blood pressure, and give you tips to make sure you eat well.
How often does Medicare cover pelvic exam?
Part B covers pap tests and pelvic exams to check for cervical and vaginal cancers. As part of the pelvic exam, Medicare also covers a clinical breast exam to check for breast cancer. Medicare covers these screening tests once every 24 months. Medicare covers these screening tests once every 12 months if you’re at high risk for cervical or vaginal cancer, or if you’re of child-bearing age and had an abnormal pap test in the past 36 months.
How often does Medicare cover mammograms?
Medicare covers screening mammograms to check for breast cancer once every 12 months for all women with Medicare who are 40 and older. Medicare covers one baseline mammogram for women between 35–39. You pay nothing for the test if the doctor or other qualified health care provider accepts assignment.
How many depression screenings does Medicare cover?
Medicare covers one depression screening per year . The screening must be done in a primary care setting (like a doctor’s office) that can provide follow-up treatment and referrals. You pay nothing for this screening if the doctor or other qualified health care provider accepts assignment.
How much does Medicare pay for chemotherapy?
For chemotherapy given in a doctor’s office or freestanding clinic, you pay 20% of the Medicare-approved amount, and the Part B deductible applies. For chemotherapy in a hospital inpatient setting covered under Part A, see hospital care (inpatient care).
How much does Medicare pay for ambulatory surgery?
Except for certain preventive services (for which you pay nothing if the doctor or other health care provider accepts assignment), you pay 20% of the Medicare-approved amount to both the ambulatory surgical center and the doctor who treats you, and the Part B deductible applies.
When do hospitals report Medicare beneficiaries?
If the beneficiary is a dependent under his/her spouse's group health insurance and the spouse retired prior to the beneficiary's Medicare Part A entitlement date, hospitals report the beneficiary's Medicare entitlement date as his/her retirement date.
What is secondary payer?
Medicare is the Secondary Payer when Beneficiaries are: 1 Treated for a work-related injury or illness. Medicare may pay conditionally for services received for a work-related illness or injury in cases where payment from the state workers’ compensation (WC) insurance is not expected within 120 days. This conditional payment is subject to recovery by Medicare after a WC settlement has been reached. If WC denies a claim or a portion of a claim, the claim can be filed with Medicare for consideration of payment. 2 Treated for an illness or injury caused by an accident, and liability and/or no-fault insurance will cover the medical expenses as the primary payer. 3 Covered under their own employer’s or a spouse’s employer’s group health plan (GHP). 4 Disabled with coverage under a large group health plan (LGHP). 5 Afflicted with permanent kidney failure (End-Stage Renal Disease) and are within the 30-month coordination period. See ESRD link in the Related Links section below for more information. Note: For more information on when Medicare is the Secondary Payer, click the Medicare Secondary Payer link in the Related Links section below.
Does Medicare pay for black lung?
Federal Black Lung Benefits - Medicare does not pay for services covered under the Federal Black Lung Program. However, if a Medicare-eligible patient has an illness or injury not related to black lung, the patient may submit a claim to Medicare. For further information, contact the Federal Black Lung Program at 1-800-638-7072.
Does Medicare pay for the same services as the VA?
Veteran’s Administration (VA) Benefits - Medicare does not pay for the same services covered by VA benefits.
Is Medicare a primary or secondary payer?
Providers must determine if Medicare is the primary or secondary payer; therefore, the beneficiary must be queried about other possible coverage that may be primary to Medicare. Failure to maintain a system of identifying other payers is viewed as a violation of the provider agreement with Medicare.