
If you have Medicare as well as another type of insurance, your coverage is provided through a coordination of benefits. In some situations, Medicare will serve as your primary payer, which means Medicare pays first. Your other insurance coverage will then serve as your secondary payer.
What is Original Medicare and how does it work?
Original Medicare includes Medicare Part A (Hospital Insurance) and Medicare Part B (Medical Insurance). You pay for services as you get them. When you get services, you’ll pay a
What are the different parts of Medicare?
What are the parts of Medicare? The different parts of Medicare help cover specific services: Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
What does Medicare Part a hospital insurance cover?
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care. What Part B covers Learn about what Medicare Part B (Medical Insurance) covers, including doctor and other health care providers' services and outpatient care.
Who pays first Medicare or liability insurance?
If you have group health plan coverage through an employer who has less than 20 employees, Medicare pays first, and the group health plan pays second. If you have a group health plan through tribal self-insurance, Medicare pays first and the group health plan pays second. I've been in an accident where no-fault or liability insurance is involved.
Does Medicare come first or second?
You can have group health plan coverage or retiree coverage based on your employment or through a family member. After the coordination period ends, Medicare pays first and your group health plan (or retiree coverage) pays second.
Is Medicare always the primary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Does Medicare automatically forward claims to secondary insurance?
If a Medicare member has secondary insurance coverage through one of our plans (such as the Federal Employee Program, Medex, a group policy, or coverage through a vendor), Medicare generally forwards claims to us for processing.
Does Medicare coverage start the month you turn 65?
The date your coverage starts depends on which month you sign up during your Initial Enrollment Period. Coverage always starts on the first of the month. If you qualify for Premium-free Part A: Your Part A coverage starts the month you turn 65.
How do you determine which insurance is primary and which is secondary?
The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" to pay. The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer.
Can you have Medicare and employer insurance at the same time?
Yes, you can have both Medicare and employer-provided health insurance. In most cases, you will become eligible for Medicare coverage when you turn 65, even if you are still working and enrolled in your employer's health plan.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
How do Medicare crossover claims work?
1. What is meant by the crossover payment? When Medicaid providers submit claims to Medicare for Medicare/Medicaid beneficiaries, Medicare will pay the claim, apply a deductible/coinsurance or co-pay amount and then automatically forward the claim to Medicaid.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
What should I be doing 3 months before 65?
You can first apply for Medicare during the three months before your 65th birthday. By applying early, you ensure your coverage will start the day you turn 65. You can also apply the month you turn 65 or within the following three months without penalty, though your coverage will then start after your birthday.
How close to my 65th birthday should I apply for Medicare?
A: The best time to enroll is during the open enrollment window around your 65th birthday – preferably in the three months before the month you turn 65, so that you'll have Medicare coverage by the time you turn 65.
Does Medicare Part B have to start on the first of the month?
Part B (Medical Insurance) Generally, you're first eligible to sign up for Part A and Part B starting 3 months before you turn 65 and ending 3 months after the month you turn 65. (You may be eligible for Medicare earlier, if you get disability benefits from Social Security or the Railroad Retirement Board.)
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is Medicare for people 65 and older?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. at the start of each year, and you usually pay 20% of the cost of the Medicare-approved service, called coinsurance.
Do you pay Medicare premiums if you are working?
You usually don't pay a monthly premium for Part A if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A."
Does Medicare Advantage cover vision?
Most plans offer extra benefits that Original Medicare doesn’t cover — like vision, hearing, dental, and more. Medicare Advantage Plans have yearly contracts with Medicare and must follow Medicare’s coverage rules. The plan must notify you about any changes before the start of the next enrollment year.
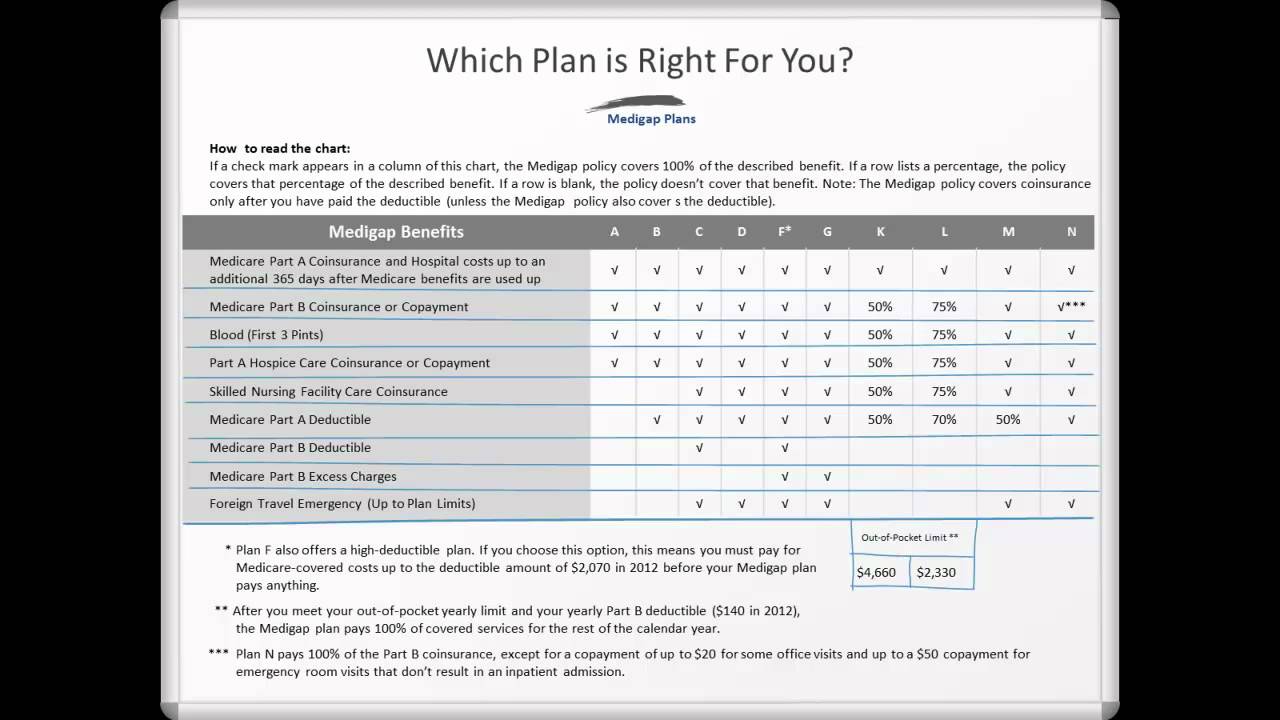
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like copayments, coinsurance, and deductibles.
Does Medicare cover prescription drugs?
Medicare drug coverage helps pay for prescription drugs you need. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage (this includes Medicare drug plans and Medicare Advantage Plans with drug coverage).
What do I need to know about Medicare?
What else do I need to know about Original Medicare? 1 You generally pay a set amount for your health care (#N#deductible#N#The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.#N#) before Medicare pays its share. Then, Medicare pays its share, and you pay your share (#N#coinsurance#N#An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).#N#/#N#copayment#N#An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug.#N#) for covered services and supplies. There's no yearly limit for what you pay out-of-pocket. 2 You usually pay a monthly premium for Part B. 3 You generally don't need to file Medicare claims. The law requires providers and suppliers to file your claims for the covered services and supplies you get. Providers include doctors, hospitals, skilled nursing facilities, and home health agencies.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. ) before Medicare pays its share. Then, Medicare pays its share, and you pay your share (. coinsurance.
What is Medicare Advantage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. .
What is a referral in health care?
referral. A written order from your primary care doctor for you to see a specialist or get certain medical services. In many Health Maintenance Organizations (HMOs), you need to get a referral before you can get medical care from anyone except your primary care doctor.
What is a coinsurance percentage?
Coinsurance is usually a percentage (for example, 20%). An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage.
Does Medicare cover assignment?
The type of health care you need and how often you need it. Whether you choose to get services or supplies Medicare doesn't cover. If you do, you pay all the costs unless you have other insurance that covers it.
Do you have to choose a primary care doctor for Medicare?
No, in Original Medicare you don't need to choose a. primary care doctor. The doctor you see first for most health problems. He or she makes sure you get the care you need to keep you healthy. He or she also may talk with other doctors and health care providers about your care and refer you to them.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
How much is the deductible for Medicare Part A?
Medicare Part A: $1,484. Medicare Part B: $203. As this shows, the deductible for Medicare Part A is lower than the average deductible for private insurance plans.
Why does Medicare cost more?
However, Medicare plans may cost more because they do not have an out-of-pocket limit, which is a requirement of all Medicare Advantage plans.
What is Medicare approved private insurance?
The health insurance that Medicare-approved private companies provide varies among plan providers, but it may include coverage for the following: assistance with Medicare costs, such as deductible, copays, and coinsurance. prescription drug coverage through Medicare Part D plans.
What is Medicare Advantage?
Medicare Advantage plans, which replace original Medicare , may offer coverage that more closely resembles that of a private insurance plan. Many Medicare Advantage plans offer dental, vision, and hearing care and prescription drug coverage.
How many employees does Medicare have?
For example, Medicare is the primary payer when a person has private insurance through an employer with fewer than 20 employees. To determine their primary payer, a person should call their private insurer directly.
What are the factors that affect the cost of private insurance?
Other factors affecting the cost of private insurance include: the age of the person. where they live. the benefits of the plan. the out-of-pocket expenses. Generally, private insurance costs more than Medicare. Most people qualify for a $0 premium on Medicare Part A.
Does Medicare cover copays?
A Medigap policy cover costs such as deductibles and copays, but the monthly premium for Medigap policies varies. Medicare premiums only cover one person. However, private insurers may extend coverage to other family members, such as dependents. Other factors affecting the cost of private insurance include:
How does private health insurance work?
Copays for services rendered and/or coinsurance are also highly likely. With all of these payments, the health insurance company will pay for you and their enrollees when they are sick. Typically, those with health insurance are relatively healthy and will not undergo significant costs but the way health insurance companies work is that the money is gathered and distributed amongst those that need it at that specific time. The bulk of the money goes to the smaller percentage of individuals who do undergo cost-heavy treatments.
Is Medicare a private insurance?
For many seniors, a combination of Medicare and private insurance provides them with the most comprehensive coverage at the most affordable rate. Medicare is known to have many gaps in their coverage and if you are not aware of these gaps, out-of-pocket expenses can be quick to add up. However, there is one privatized insurance plan that is approved for sale by the government that can provide this combination for optimal coverage and costs.
Is Medicare a government program?
As mentioned, Medicare is a government health insurance program that provides hospital coverage (Medicare Part A), outpatient services (Medicare Part B) and prescription drug coverage (Medicare Part D). It is important to realize that Medicare is not a health insurance company in itself. It is a government program that contracts private healthcare providers to offer medical services to seniors (and qualifying individuals under the age of 65) for an affordable rate. And if you choose Medicare Advantage, you’ll be paying a Medicare-approved private health insurance company who follows the guidelines set by Medicare in order to obtain your benefits.
How to learn more about Medicare?
How to Learn More About Your Medicare Options. Primary insurance isn't too hard to understand; it's just knowing which insurance pays the claim first. Medical billing personnel can always help you figure it out if you're having trouble. While it's not hard to understand primary insurance, Medicare is its own beast.
Is Medicare primary insurance in 2021?
Updated on July 13, 2021. Many beneficiaries wonder if Medicare is primary insurance. But, the answer depends on several factors. While there are times when Medicare becomes secondary insurance, for the most part, it’s primary. Let’s go into further detail about what “primary” means, and when it applies.
Is Medicare a primary or secondary insurance?
Mostly, Medicare is primary. The primary insurer is the one that pays the claim first, whereas the secondary insurer pays second. With a Medigap policy, the supplement is secondary. Medicare pays claims first, and then Medigap pays. But, depending on the other policy, you have Medicare could be a secondary payer.
Does Medicare pay your claims?
Since the Advantage company pays the claims, that plan is primary. Please note that Medicare WON’T pay your claims when you have an Advantage plan. Medicare doesn’t become secondary to an Advantage plan. So, you’ll rely on the Advantage plan for claim approvals.
Can you use Medicare at a VA hospital?
Medicare and Veterans benefits don’t work together; both are primary. When you go to a VA hospital, Veteran benefits are primary. Then, if you go to a civilian doctor or hospital, Medicare is primary. But, you CAN’T use Veterans benefits at a civilian doctor. Also, you can’t use Medicare benefits at the VA.
Is Medicare a part of tricare?
Medicare is primary to TRICARE. If you have Part A, you need Part B to remain eligible for TRICARE. But, Part D isn’t a requirement. Also, TRICARE covers your prescriptions. Your TRICARE will be similar to a Medigap plan; it covers deductibles and coinsurances.
Who pays first for healthcare?
When you have private insurance and Medicare, one of the two providers will pay for healthcare services first. The second provider may then potentially cover the remaining costs. Who pays first depends on your individual situation and the type of private insurance you have.
How does Medicare work with a group plan?
How Medicare works with your group plan’s coverage depends on your particular situation, such as: If you’re age 65 or older. In companies with 20 or more employees, your group health plan pays first. In companies with fewer than 20 employees, Medicare pays first. If you have a disability or ALS.
What is the difference between Cobra and tricare?
COBRA allows you to temporarily keep private insurance coverage after your employment ends. You’ll also keep your coverage if you’re on your spouse’s private insurance and their employment ends. TRICARE. TRICARE provides coverage for active and retired members of the military and their dependents.
What pays first for a company with fewer than 20 employees?
In companies with fewer than 20 employees, Medicare pays first. If you have a disability or ALS. In companies with 100 or more employees, your group health plan pays first. When a company has fewer than 100 employees, Medicare pays first. If you have ESRD.
How to contact the SSA about Medicare?
Contacting the SSA at 800-772-1213 can help you get more information on Medicare eligibility and enrollment. State Health Insurance Assistance Program (SHIP). Each state has its own SHIP that can aid you with any specific questions you may have about Medicare. United States Department of Labor.
What is the process called when you have both insurance and a primary?
When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer. Once the payment order is determined, coverage works like this: The primary payer pays for any covered services until the coverage limit has been reached.
What is health insurance?
Health insurance covers much of the cost of the various medical expenses you’ll have during your life. Generally speaking, there are two basic types of health insurance: Private. These health insurance plans are offered by private companies.
What is a Medigap plan?
Medigap plans (also known as Medicare Supplement Insurance), are private health insurance plans that help pay for the "gaps" in payment for Medicare-covered care left by traditional Medicare ; these include copayments, coinsurance, and deductibles. In many cases, someone with traditional Medicare must purchase a separate Part D drug plan as well as a Medigap plan to supplement their Medicare benefits. Medigap policies do not work with MA plans and it is illegal for anyone to sell an MA enrollee a Medigap policy unless they are switching to traditional Medicare.
What is Medicare Advantage Plan?
Individuals who have traditional Medicare, or a Medicare Advantage plan that does not include prescription drug coverage, who want Part D coverage, must purchase it separately. This is called a “stand-alone” Prescription Drug Plan (PDP). A Medicare Advantage plan that includes both health and drug coverage is referred to as a Medicare Advantage ...
What should be identified in MA preventive services?
All preventive services and extra benefits should be identified, as well as any limitations associated with visits or services. Determine where you are required to go for regular, non-urgent care. Check into the MA plan's physicians to determine if your physicians are in the plan’s network.
Does Medicare have a cap on out-of-pocket expenses?
You may also have to pay for deductibles, coinsurance and copays. Traditional Medicare has no out-of-pocket maximum or cap on what you may spend on health care. With traditional Medicare, you will have to purchase Part D drug coverage and a Medigap plan separately (if you choose to purchase one). Medicare Advantage.
Do you need to buy a Medigap plan?
Some beneficiaries have employer or union coverage that pays costs that traditional Medicare does not cover; those who do not may need to buy a Medigap plan. Other individuals may be eligible for Medicaid that can also cover such costs and may not need Medigap.
Does Medicare Part B require monthly premiums?
Medicare Part B requires the payment of a monthly premium. You must elect to either accept or decline this coverage, but be aware that there may be penalties for not enrolling during your initial enrollment period. For more details, see our Eligibility and Enrollment page. Medicare Advantage.
Does Medicare cover prescription drugs?
Traditional Medicare does not offer coverage for prescription drugs. In traditional Medicare you may have to buy a Medigap plan as well as a separate Part D prescription drug plan.
