How does Medicare supplement insurance work with Medicare?
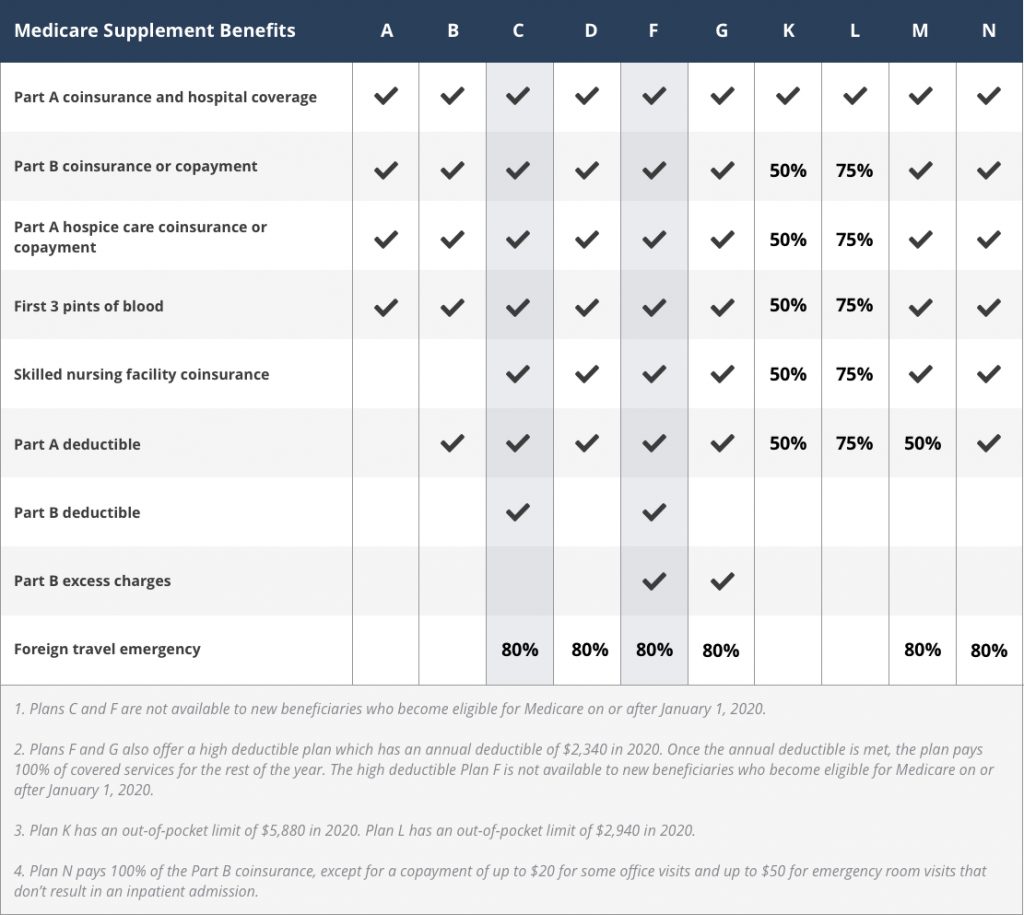
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people new to Medicare can no longer cover the Part B deductible.
How much do Medicare supplement plans cost?
Some Medicare Advantage plans have a monthly premium, but most people choose a $0 premium plan. Among those who do pay a premium, the average cost is $25 a month, which usually includes Part D coverage. You don’t have an annual deductible with Medicare Supplement plans unless you choose a high-deductible plan.
What is the difference between Medicare Advantage and Medicare supplement plans?
Most Medicare Advantage plans require you to use an approved provider network. On the other hand, a Medicare Supplement plan allows you to be treated by any provider that accepts Medicare. With the most popular Medicare Supplement plans , you only pay your monthly premium and your Part B deductible.
Do Medicare supplement plans pay 100% of out-of-pocket costs?
The most popular Medicare Supplement plans pay 100% of your out-of-pocket costs with Part A and Part B, except for the Part B deductible. All Medicare Advantage plans cap your annual out-of-pocket costs.

Which Medicare plan pays the most?
Plan F premiums are usually the highest of all Medicare Supplement plans. This makes sense because it offers the highest level of coverage.
What is the difference between a Medicare Supplement and a Medicare Advantage plan?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.
What are the advantages and disadvantages of Medicare Supplement plans?
Medicare Advantage offers many benefits to original Medicare, including convenient coverage, multiple plan options, and long-term savings. There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling.
Which is better Medigap or Medicare Advantage plan?
Medicare Advantage is a money-saving choice if you are in good health with few medical expenses. Otherwise, Medigap is generally better for those with serious medical conditions. You cannot have Medicare Advantage and Medigap at the same time.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Can I switch from Medicare Advantage to Medicare Supplement?
Once you've left your Medicare Advantage plan and enrolled in Original Medicare, you are generally eligible to apply for a Medicare Supplement insurance plan. Note, however, that in most cases, when you switch from Medicare Advantage to Original Medicare, you lose your “guaranteed-issue” rights for Medigap.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
What is the downside to Medigap?
Some disadvantages of Medigap plans include: Higher monthly premiums. Having to navigate the different types of plans. No prescription coverage (which you can purchase through Plan D)
How Much Is Medigap per month?
In 2020, the average premium for Medicare supplemental insurance, or Medigap, was approximately $150 per month or $1,800 per year, according to Senior Market Sales, a full-service insurance organization.
Do Medigap plans have a maximum out-of-pocket?
Medigap plans don't have a maximum out-of-pocket because they don't need one. The coverage is so good you'll never spend $5,000 a year on medical bills.
Are Medigap policies worth it?
Depending on your health care needs, a Medigap policy can be a worthwhile investment. If you decide to get a Medigap policy, the best time to enroll is during the six-month Open Enrollment Period. If you're about to turn 65, your Medigap Open Enrollment period starts the first day of the month that you turn 65.
Why would someone choose a Medicare Advantage plan?
Under Medicare Advantage, you will get all the services you are eligible for under original Medicare. In addition, some MA plans offer care not covered by the original option. These include some dental, vision and hearing care. Some MA plans also provide coverage for gym memberships.
What is Medigap?
The Medigap definition is easy: Medigap and Medicare Supplement are the same thing. In this article, we’ll use “Medicare Supplement” to keep things simple.
What is Medicare Part C?
Here is another easy one. Medicare Part C and Medicare Advantage are the same thing. This article will use “Medicare Advantage”. So far, so good.
What is Medicare Supplement?
Medicare Supplement is just that, a supplement to Medicare coverage. In order to use Medicare Supplement, you must have Original Medicare coverage (Medicare Parts A and B).
What plan is more affordable?
Medicare Advantage plans will have lower out-of-pocket expenses because they manage the resources that you use. The cost of prescription drugs is usually included in the plan. Some plans offer other benefits too —such as vision, dental, and fitness programs. What you give up is the ability to see out-of-network providers at the same low cost.
What is an Enrollment Period?
If you just became eligible for Medicare, you can enroll in a Medicare Advantage plan right away.
Get started now
Interested in learning more about Medicare, Medigap, and Medicare Advantage plans? WebMD Connect to Care Advisors may be able to help.
What is Medicare Advantage?
Medicare Advantage plans negotiate contracts with networks doctors, hospitals, and other healthcare providers. The agreements they reach can help to keep their costs lower. This means that you must adhere to their networks or face substantially higher out of pocket costs.
How are Medicare Advantage Plans structured?
How Medicare Advantage Plans Are Structured. Medicare Advantage replaces your Medicare Part A and Part B services. Most of the time it replaces your Part D as well. A Medicare Advantage plan combines them into one coverage with a private insurance company. This is what is known as Part C of Medicare.
How long does it take to get a Medigap plan?
This period starts six months before you enroll in Part B of Medicare and continues the six months after. Medicare Advantage and Part D allow a 3-month open enrollment before and after your date of first coverage under Part B. You will likely have to be underwritten to get a Medigap plan once you are out of your Open Enrollment period.
How long does Medicare lock you in?
If you enroll in a Medicare Advantage plan, Medicare locks you into that plan until December 31st. Medicare Advantage plans and Part D prescription drug plans have only one window of opportunity each year for you to enroll. It happens from October 15 through December 7 each year. During that time, you can change plans or go from MAPD to original Medicare with a Medicare Supplement plan (or vice versa). There are Special Enrollment periods such as if you move out of your network coverage area. You have an Initial Enrollment Period three months before and three months after you first enroll in Part B of Medicare. Other than that, you cannot change plans or move back to original Medicare.
What is a Medigap plan?
Under a Medigap plan, Medicare first pays its portion of the bill and then sends the remainder of the bills to your Medicare supplement company to pay their portion. This is done electronically through what is called the crossover system.
What are the different types of Medicare insurance?
There are two types of private plans that you can purchase that will help fill the gaps of Medicare – Medicare supplements (Medigap) or Medicare Advantage. These two plans are very different and it is imperative that you understand the differences.
How much does Medicare cover in 2021?
If you go with Medicare alone with no additional coverage, you will quickly learn that there are a lot of gaps that Medicare does not cover – a Part A deductible ($1,484 in 2021) that you must pay to the hospital to cover you for up to 60 days of hospital care.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
Does Medigap cover everything?
Medigap policies don't cover everything. Medigap policies generally don't cover. long-term care. Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
What Is Supplemental Health Insurance?
Supplemental insurance is any coverage that goes beyond what is included in your standard health care plan. Depending on the type of plan you buy, supplemental insurance may help cover some out-of-pocket costs (such as deductibles, coinsurance or copays) or pay a lump sum of cash in the event of a specific event or illness.
What Is Medicare Supplement Insurance?
Medicare Supplement Insurance, also known as Medigap, is only available to people enrolled in Original Medicare (Part A and Part B). You may not have a Medicare Supplement Insurance plan and a Medicare Advantage plan (Part C) at the same time.
Have Questions About Medicare Supplement Insurance?
You can call to speak with a licensed insurance agent today to learn more about Medicare Supplement Insurance, including plans available where you live.
Is it better to have Medicare Advantage or Medicare Supplement (Medigap)?
Whether you choose to apply for a Medicare Advantage plan vs. a Medicare Supplement insurance plan depends on your needs. Here are a few factors to consider when deciding whether Medicare Advantage or Medicare Supplement is better for you:
Can you have a Medicare Advantage plan and a Medicare Supplement plan?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.
Can you change from a Medicare Advantage plan to a Medicare Supplement plan?
During the Annual Enrollment Period, which runs from October 15 to December 7 each year, you are free to reconsider your Medicare coverage. If you decide you want to try a Medicare Supplement plan vs. Medicare Advantage plan, you can make that change during this period. 4
What percentage of Medicare supplement is paid?
After this is paid, your supplement policy pays your portion of the remaining cost. This is generally 20 percent. Some policies pay your deductibles The deductible is a set amount which you must pay before Medicare begins covering your health care costs.
How many people does Medicare Supplement cover?
Keep in mind that, just like Medicare, Medicare Supplement plans are individual insurance policies. They only cover one person per plan. If you want coverage for your spouse, you must purchase a separate plan.
What is Medicare Supplement?
Medicare supplement insurance policies help fill in the gaps left by Original Medicare health care insurance. For many people, Medicare Supplement, also known as Medigap, insurance helps them economically by paying some of the out-of-pocket costs associated with Original Medicare.
How long does it take to get a Medigap plan?
When you turn 65 and enroll in Part B, you will have a 6-month Initial Enrollment Period to purchase any Medigap plan sold in your state. During this time, you have a “guaranteed issue right” to buy any plan available. They are required to accept you and cannot charge you more due to any pre-existing conditions.
How long does Medicare cover travel?
Each plan varies in what it covers, but all plans pay for Medicare Part A (hospital insurance) coinsurances for up to 365 days beyond the coverage that Medicare offers. Some of the plans cover a percentage of the cost for emergency health care while traveling abroad.
How old do you have to be to qualify for medicare?
To be eligible for Medicare, you must be at least 65 years old, a citizen of the United States or permanent legal resident for at least five consecutive years. Also, you, or your spouse, must have worked and paid federal taxes for at least ten years (or 40 quarters).
Does Medicare cover long term care?
Most plans do not cover long-term care, vision, dental, hearing care, or private nursing care. All Medicare Supplement insurance coverage comes with a monthly premium which you pay directly to your provider. How much you pay depends on which plan you have.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).