Specifically, CMS
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…
Full Answer
What are the CMS eligibility targeting requirements for MTM programs?
Jun 21, 2021 · At least 50 percent of Medicare beneficiaries are enrolled in Medicare Advantage plans in two states (MN, FL) and Puerto Rico. Puerto Rico has the highest Medicare Advantage penetration, with 80 ...
What percentage of MTM programs use medical data to identify beneficiaries?
May 10, 2019 · • All MTM programs use drug claims data to identify eligible beneficiaries for their MTM programs in 2019. • In addition, 21% of MTM programs also use medical data to identify eligible beneficiaries (21.9% of MA-PDs, 6.7% of PDPs, and 27.7% of MMPs). This is an increase from 2018 for all contract types.
Is MTM considered an administrative cost by CMS?
The Henry J. Kaiser Family Foundation Headquarters: 185 Berry St., Suite 2000, San Francisco, CA 94107 | Phone 650-854-9400 Washington Offices and Barbara Jordan Conference Center: 1330 G …
Are Medicare Advantage plans still available in Minnesota?
May 22, 2020 · Requirements for Medication Therapy Management (MTM) Programs: Under 423.153 (d), a Part D sponsor must have established a MTM program that: Ensures optimum therapeutic outcomes for targeted beneficiaries through improved medication use. Reduces the risk of adverse events. Is developed in cooperation with licensed and practicing pharmacists …
What is a factor when determining a patient's eligibility for MTM services?
Which Medicare Part covers MTM?
What are the drug utilization management rules for Medicare?
What is a MTM function that techs can perform in most states?
What is the CMR portion of a medication therapy review MTM )?
Does Medicare pay for 99605?
What are the basic three components of utilization management?
What are Tier 4 and 5 drugs?
What is considered prescription drug management?
How much medication can eligible patients in federal disaster areas receive through Epap?
Which item should patients bring to their MTM appointment?
How can a pharmacy technician help out with MTM?
How many Medicare Advantage enrollees are in a plan that requires higher cost sharing than the Part A hospital
Nearly two-thirds (64%) of Medicare Advantage enrollees are in a plan that requires higher cost sharing than the Part A hospital deductible in traditional Medicare for a 7-day inpatient stay, and more than 7 in 10 (72%) are in a plan that requires higher cost sharing for a 10-day inpatient stay.
How many people will be enrolled in Medicare Advantage in 2020?
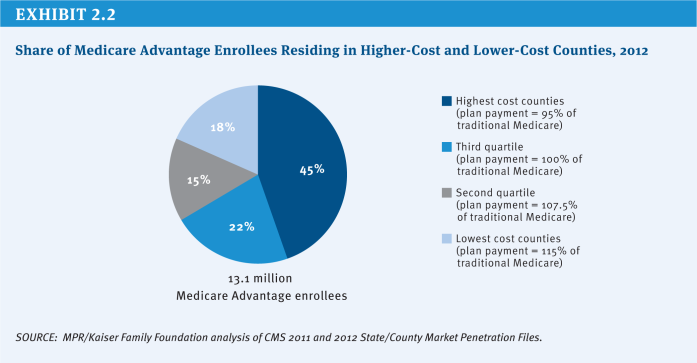
Enrollment in Medicare Advantage has doubled over the past decade. In 2020, nearly four in ten (39%) of all Medicare beneficiaries – 24.1 million people out of 62.0 million Medicare beneficiaries overall – are enrolled in Medicare Advantage plans; this rate has steadily increased over time since the early 2000s.
What are the companies that are part of Medicare Advantage?
Medicare Advantage enrollment is highly concentrated among a small number of firms. UnitedHealthcare and Humana together account for 44 percent of all Medicare Advantage enrollees nationwide, and the BCBS affiliates (including Anthem BCBS plans) account for another 15 percent of enrollment in 2020. Another four firms (CVS Health, Kaiser Permanente, Centene, and Cigna) account for another 23 percent of enrollment in 2020. For the fourth year in a row, enrollment in UnitedHealthcare’s plans grew more than any other firm, increasing by more than 500,000 beneficiaries between March 2019 and March 2020. This is also the first year that Humana’s increase in plan year enrollment was close to UnitedHealthcare’s, with an increase of about 494,000 beneficiaries between March 2019 and March 2020. CVS Health purchased Aetna in 2018 and had the third largest growth in Medicare Advantage enrollment in 2020, increasing by about 396,000 beneficiaries between March 2019 and March 2020.
How much is the deductible for Medicare Advantage 2020?
In contrast, under traditional Medicare, when beneficiaries require an inpatient hospital stay, there is a deductible of $1,408 in 2020 (for one spell of illness) with no copayments until day 60 of an inpatient stay.
What percentage of Medicare beneficiaries are in Miami-Dade County?
Within states, Medicare Advantage penetration varies widely across counties. For example, in Florida, 71 percent of all beneficiaries living in Miami-Dade County are enrolled in Medicare Advantage plans compared to only 14 percent of beneficiaries living in Monroe County (Key West).
What are the changes to Medicare 2020?
Changes for 2020 due to COVID-19: The COVID-19 stimulus package, the Coronavirus Aid, Relief, and Economic Security (CARES) Act, includes $100 billion in new funds for hospitals and other health care entities. The Centers for Medicare and Medicaid Services (CMS) has recently made $30 billion of these funds available to health care providers based on their share of total Medicare fee-for-service (FFS) reimbursements in 2019, resulting in higher payments to hospitals in some states than in others. Hospitals in states with higher shares of Medicare Advantage enrollees may have lower FFS reimbursement overall. As a result, some hospitals and other health care entities may be reimbursed less that they would if the allocation of funds took into account payments received on behalf of Medicare Advantage enrollees.
What is the analysis of Medicare Advantage 2020?
It also includes analyses of Medicare Advantage plans’ extra benefits and prior authorization requirements. The analysis also highlights changes pertaining to Medicare Advantage coverage that have occurred in 2020 in response to the COVID-19 crisis. 1. Enrollment in Medicare Advantage has doubled over the past decade.
Abstract
Medicare Part D prescription drug plans must offer medication therapy management to beneficiaries with multiple chronic conditions and high drug expenditures. However, plan sponsors have considerable latitude in setting eligibility criteria.
Study Data And Methods
We characterized the relationship between Part D contract-level eligibility criteria for medication therapy management and enrollment rates, using publicly available data from the CMS website. All data were for 2012, the latest year for which complete information was available at the time of writing.
Study Results
We analyzed 532 Part D contracts—464 MA-PD contracts with 145 sponsors and 68 PDP contracts with 56 sponsors—listed in the CMS Parts C and D reporting requirements public use files for 2012 11 (we excluded 32 contracts that failed CMS data validation checks and 19 contracts that reported having fewer than eleven enrollees in medication therapy management)..
Discussion
Our analysis showed that enrollment rates in medication therapy management varied widely across Part D sponsors in 2012, from below 0.2 percent of beneficiaries to nearly 60 percent. We demonstrated that this wide variation appears to be a function of which criteria sponsors selected for eligibility.
Conclusion
As currently designed, Part D sponsors have the freedom to offer medication therapy management services to broad or narrow segments of their enrollment pools. Most sponsors have chosen the latter option.
ACKNOWLEDGMENTS
This study was funded by Pharmaceutical Research and Manufacturers of America (PhRMA) and the National Association of Chain Drug Stores (NACDS). Samantha Dougherty is employed by PhRMA. Laura Miller is employed by the NACDS.
NOTES
1 Larrick AK . CY 2016 medication therapy management program guidance and submission instructions [Internet]. Baltimore (MD) : Centers for Medicare and Medicaid Services ; 2015 Apr 7 [cited 2016 Jul 12 ].
Summary
A new analysis from Avalere Health finds that less than half of all Medicare prescription drug (Part D) enrollees eligible for medication therapy management (MTM) programs receive these services.
Methodology
These findings are the result of an initial analysis of recently released plan data based on Part C and D Reporting Requirements as part of the Public Use File (PUF) by the Centers for Medicare and Medicaid Services (CMS).
Who can be used as support staff for MTM?
Non-Qualified MTM providers, such as pharmacy technicians, pharmacy students/interns, and case workers may be used as support staff to assist the qualified MTM providers. Multiple selections were allowed; not mutually exclusive.
What is a CMR?
A CMR is an interactive person -to-person or telehealth medication review and consultation conducted in real -time between the patient and/or other authorized individual, such as prescriber or caregiver, and the pharmacist or other qualified provider and is designed to improve patients’ knowledge of their prescriptions, over -the-counter (OTC) medications, herbal therapies and dietary supplements, identify and address problems or concerns that patients may have, and empower patients to self manage their medications and their health conditions.
How long does a CMR need to be in CMS?
An individualized, written summary in CMS’ Standardized Format must be provided following each CMR and should be provided within 14 calendar days. This applies whether the CMR is provided to the beneficiary, or to the beneficiary’s prescriber, caregiver, or other authorized representative who may take part in the CMR if the beneficiary cannot accept the offer to participate. The Standardized Format with detailed instructions for implementation, as well as frequently asked questions, are posted on the CMS MTM web page at www.cms.gov > Medicare > Prescription Drug Coverage Contracting > Medication Therapy Management
When is Part D required?
Pursuant to 42 CFR § 423.2265(b)(13), Part D sponsors are required by January 1, 2022 to include on their websites a separate section or page about the sponsor’s MTM program that provides the following: