NEW YORK-- (BUSINESS WIRE)--Seventy-seven percent of employers spend 16 percent or more of their total healthcare budget on pharmacy benefits for their employees, with nearly five percent of employers spending more than 30 percent on pharmacy, according to the fifth annual “Prescription Drug Benefit Survey” by Buck Consultants
Buck Consultants
Buck is a global HR benefits and human resource consulting firm controlled by H.I.G. Capital.
How much does Medicare spend on prescription drugs?
Sep 02, 2021 · The program pays for about one-fifth of all healthcare spending in the United States, including 28 percent of prescription drug costs and 39 percent of home health spending (which includes in-home care by skilled nurses to support recovery and self-sufficiency in the wake of illness or injury).
What percentage of federal budget is spent on Medicare?
30 percent of total net spending on prescription drugs in both Medicare Part D and Medicaid, although they accounted for only about 1 percent of all prescriptions dispensed in each program. New drug development has emphasized specialty drugs and contributed to the increased
What does the Governor’s budget mean for pharmacy services?
Through the 1980s and early 1990s, 5 percent to 6 percent of all spending on health care services and supplies was on prescription drugs obtained in the retail market (that is, from pharmacies— either in stores or by mail order). By 2018, that share was 10 percent (see Figure 1).
Does Medicare cover drug out-of-pocket costs?
Apr 22, 2021 · Written by Diane Archer. With Medicare prescription drug spending, the 80-20 rule applies. A new Kaiser Family Foundation analysis by Juliette Cubanski and Tricia Neuman finds that a small portion of Medicare Part B and Part D prescription drugs make up a large percentage of Medicare drug costs. Cubanski and Neuman estimate that Medicare Part D drug spending …
What percentage does Medicare pay for prescription drugs?
Brand-name prescription drugs. Once you reach the coverage gap, you'll pay no more than 25% of the cost for your plan's covered brand-name prescription drugs. You'll pay this discounted rate if you buy your prescriptions at a pharmacy or order them through the mail.
How Much Does Part B spend on drugs?
In 2018, the Medicare program and its beneficiaries spent roughly $35 billion on drugs paid through Part B; from 2009 through 2018, Part B drug spending grew at an average annual rate of 12 percent.Jun 22, 2021
How much money is made through over the counter drugs?
For 2020, it is estimated that OTC sales in the United States reached between 36 and 37 billion U.S. dollars.
How much did the US spend on prescription drugs in 2020?
348.4 billion U.S. dollarsThe Centers for Medicare and Medicaid Services reported prescription drug expenditure in the United States came to some 348.4 billion U.S. dollars in 2020. This amount includes only retail drug spending, excluding nonretail.Dec 15, 2021
Does Medicare Part B pay for prescriptions?
Medicare Part B (Medical Insurance) includes limited drug coverage. It doesn't cover most drugs you get at the pharmacy. You'll need to join a Medicare drug plan or health plan with drug coverage to get Medicare coverage for prescription drugs for most chronic conditions, like high blood pressure.
What drugs does Medicare spend the most on?
Here are the 10 drugs Medicare spent the most money on in 2020 and whose prices increased in January 2022:Xarelto. ... Januvia. ... Trulicity. ... Imbruvica. Use: Cancer treatment. ... Jardiance. Use: Diabetes treatment. ... Humira (Cf) pen. Use: Rheumatoid arthritis, plaque psoriasis treatment. ... Ibrance. Use: Cancer treatment. ... Symbicort.More items...•Mar 10, 2022
Are OTC drugs less effective than prescription?
OTC drugs typically treat conditions that are easy to self-diagnose, such as headaches, colds and allergies, and can be purchased at grocery stores, drug stores, convenience stores and supermarkets. These drugs are not as potent as Rx drugs, and it is less likely that they can be misused or abused – but it can happen.
Who decides if a drug is a prescription or over the counter drug?
the Federal Drug Administration (FDA)Prescription drugs are regulated by the Federal Drug Administration (FDA) through the New Drug Application Process for approval for marketing in the United States. The FDA regulates OTC drugs through a drug monograph containing acceptable ingredients, doses, formulations and labeling requirements.
Why does a drug change from prescription to OTC?
After the Food, Drug, and Cosmetic Act, safety of the medications for consumers had to be proven. Medications always have some risks or possible side effects, but the federal drug administration makes a decision to switch to OTC based on how likely those risks can occur when a patient self medicates.
What percentage of healthcare is paid by the government?
Contrary to the notion that the country's health care is primarily a privately funded system, 71 percent of health care expenditures in California are paid for with public funds, according to a new analysis by the UCLA Center for Health Policy Research.Aug 31, 2016
What percentage of US GDP is healthcare?
19.7%In 2020, U.S. national health expenditure as a share of its gross domestic product (GDP) reached an all time high of 19.7%....U.S. national health expenditure as percent of GDP from 1960 to 2020.CharacteristicPercentage of GDP202019.7%201917.6%201817.6%201717.7%9 more rows•Jan 4, 2022
How much does the average American spend on healthcare 2021?
$5,952/YearIn 2021, Americans Will Spend An Average of $5,952/Year for Health Insurance. These numbers actually show a slight decrease – 1.59% – in premiums from the 2020 plan year, but most surprisingly is by how much costs vary by state.Nov 23, 2020
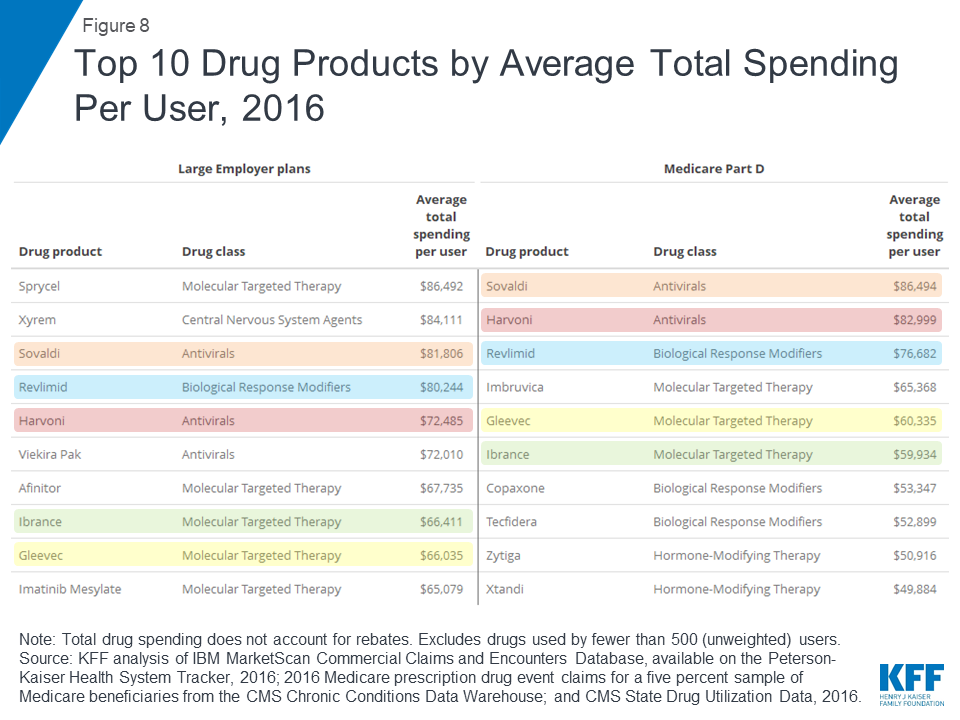
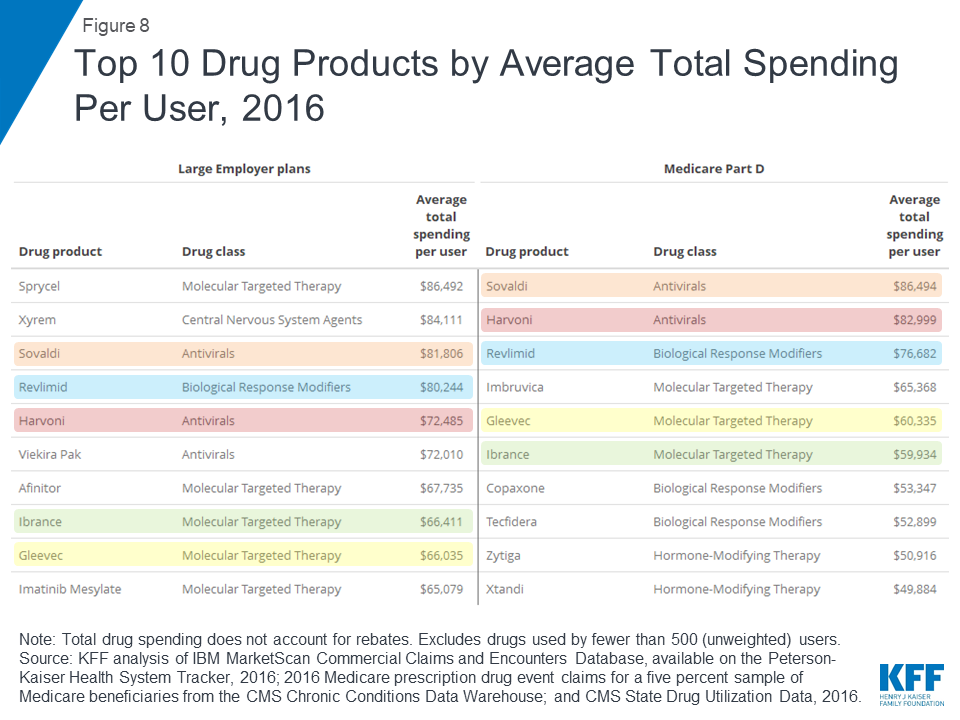
How much of Medicare was covered by prescription drugs in 2016?
Prescription drugs covered under both Part B and Part D accounted for 19% of all Medicare spending in 2016. 3. Ten drugs accounted for 17% of all Part D spending in 2016 (including both Medicare and out-of-pocket spending). 4.
How much did Medicare Part D spend in 2016?
Medicare Part D enrollees who did not receive low-income subsidies spent about $500 out of pocket on their prescriptions in 2016, on average, but 1 million enrollees with spending above the catastrophic threshold spent nearly $3,200 out of pocket. 8.
Is Medicare a private insurance?
Medicare is second only to private insurance as a major payer for retail prescription drugs. The program’s share of the nation’s retail prescription drug spending has increased from 18% in 2006 to 30% in 2017.
Can Medicare Part D pay out of pocket?
Medicare Part D enrollees can pay thousands of dollars out of pocket for specialty tier drugs, with the majority of costs for many specialty drugs occurring in the catastrophic phase of the benefit. 10. Many proposals to reduce prescription drug costs enjoy broad support among Democrats and Republicans.
What are the two types of Medicare Part D plans?
Two categories of plans participate in Medicare Part D: stand-alone prescription drug plans , which enroll beneficiaries who receive their other Medicare coverage through the traditional FFS program, and Medicare Advantage prescription drug plans. The plans compete for enrollees on the basis of premiums, benefit design, specific drugs covered, and quality of services.
What is specialty medicine?
Specialty drugs typically treat chronic, complex, or rare conditions, frequently have high prices, and may require special handling or monitoring of patients. From 2010 through 2015, such drugs accounted for a growing share of new drugs introduced to the market, and they were introduced at much higher prices than nonspecialty drugs. In 2015, brand-name specialty drugs accounted for about 30 percent of total net spending on prescription drugs in both Medicare Part D and Medicaid, although they accounted for only about 1 percent of all prescriptions dispensed in each program.
Does Medicaid cover outpatient pharmacy?
(The federal subsidy amount varies across states.) Medicaid outpatient pharmacy benefits may be delivered by Medicaid FFS, wherein states directly reimburse pharmacies for prescription drugs. Alternatively, states may contract with private managed care plans to administer the drug benefits together with medical benefits. Under the Medicaid program, beneficiaries generally have low cost sharing for prescription drugs. According to CMS, the federal share of Medicaid drug spending on outpatient pharmacy benefits, net of rebates, was $21 billion in 2015.33
How much did the NHE increase in 2019?
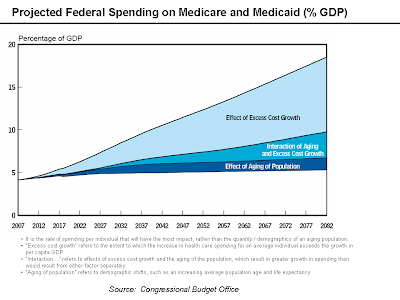
NHE grew 4.6% to $3.8 trillion in 2019, or $11,582 per person, and accounted for 17.7% of Gross Domestic Product (GDP). Medicare spending grew 6.7% to $799.4 billion in 2019, or 21 percent of total NHE. Medicaid spending grew 2.9% to $613.5 billion in 2019, or 16 percent of total NHE.
What was the per person spending for 2014?
In 2014, per person spending for male children (0-18) was 9 percent more than females. However, for the working age and elderly groups, per person spending for females was 26 and 7 percent more than for males. For further detail see health expenditures by age in downloads below.
How much did hospital expenditures grow in 2019?
Hospital expenditures grew 6.2% to $1,192.0 billion in 2019, faster than the 4.2% growth in 2018. Physician and clinical services expenditures grew 4.6% to $772.1 billion in 2019, a faster growth than the 4.0% in 2018. Prescription drug spending increased 5.7% to $369.7 billion in 2019, faster than the 3.8% growth in 2018.
How much did prescription drug spending increase in 2019?
Prescription drug spending increased 5.7% to $369.7 billion in 2019, faster than the 3.8% growth in 2018. The largest shares of total health spending were sponsored by the federal government (29.0 percent) and the households (28.4 percent). The private business share of health spending accounted for 19.1 percent of total health care spending, ...
How much did Utah spend on health care in 2014?
In 2014, per capita personal health care spending ranged from $5,982 in Utah to $11,064 in Alaska. Per capita spending in Alaska was 38 percent higher than the national average ($8,045) while spending in Utah was about 26 percent lower; they have been the lowest and highest, respectively, since 2012.
How much did Medicaid spend in 2019?
Medicaid spending grew 2.9% to $613.5 billion in 2019, or 16 percent of total NHE. Private health insurance spending grew 3.7% to $1,195.1 billion in 2019, or 31 percent of total NHE. Out of pocket spending grew 4.6% to $406.5 billion in 2019, or 11 percent of total NHE.
Which region has the lowest health care spending per capita?
In contrast, the Rocky Mountain and Southwest regions had the lowest levels of total personal health care spending per capita ($6,814 and $6,978, respectively) with average spending roughly 15 percent lower than the national average.
How much does Medicare Advantage pay in 2020?
However, 18 percent of beneficiaries in MA-PDs (2.8 million enrollees) pay at least $50 per month, including 6 percent who pay $100 or more per month, in addition to the monthly Part B premium. The MA-PD premium includes both the cost of Medicare-covered Part A and Part B benefits and Part D prescription drug coverage. Among MA-PD enrollees who pay a premium for their plan, the average premium is $63 per month. Altogether, including those who do not pay a premium, the average MA-PD enrollee pays $25 per month in 2020.
What is KFF enrollment dashboard?
KFF is now using the Medicare Enrollment Dashboard for enrollment data, from March of each year. In previous years, KFF has used the Medicare Advantage Penetration Files to calculate the number of Medicare beneficiaries eligible for Medicare.
What percentage of Medicare Advantage plans are high quality?
11. The majority (78%) of Medicare Advantage enrollees are in plans that receive high quality ratings (4 or more stars) and related bonus payments. In 2020, more than three-quarters (78%) of Medicare Advantage enrollees are in plans with quality ratings of 4 or more stars, an increase from 2019 (72%).
How many Medicare Advantage enrollees are in a plan that requires higher cost sharing than the Part A hospital
Nearly two-thirds (64%) of Medicare Advantage enrollees are in a plan that requires higher cost sharing than the Part A hospital deductible in traditional Medicare for a 7-day inpatient stay, and more than 7 in 10 (72%) are in a plan that requires higher cost sharing for a 10-day inpatient stay.
How much is the deductible for Medicare Advantage 2020?
In contrast, under traditional Medicare, when beneficiaries require an inpatient hospital stay, there is a deductible of $1,408 in 2020 (for one spell of illness) with no copayments until day 60 of an inpatient stay.
What percentage of Medicare beneficiaries are in Miami-Dade County?
Within states, Medicare Advantage penetration varies widely across counties. For example, in Florida, 71 percent of all beneficiaries living in Miami-Dade County are enrolled in Medicare Advantage plans compared to only 14 percent of beneficiaries living in Monroe County (Key West).
How many people will be enrolled in Medicare Advantage in 2020?
Enrollment in Medicare Advantage has doubled over the past decade. In 2020, nearly four in ten (39%) of all Medicare beneficiaries – 24.1 million people out of 62.0 million Medicare beneficiaries overall – are enrolled in Medicare Advantage plans; this rate has steadily increased over time since the early 2000s.
What are health care related taxes?
Many states levy licensing fees, assessments, or other mandatory payments on the provision of health care services or products. These are referred to as “health care‑related taxes.” Given its significant role in funding health care, the federal government has existing rules that regulate states’ health care‑related taxes to the extent that these are levied to draw down federal funds. The rules apply, for example, to taxes on direct health care services (such as hospital inpatient stays) as well as payers of health care services (such as health insurer revenue or enrollment).
What would the new rules do to prevent health care related taxes?
New Proposed Rules Would Prohibit Health Care‑Related Taxes From Placing an Undue Burden on Medicaid. As previously noted, the federal government already has rules that effectively prohibit health care‑related taxes if the tax burden falls too disproportionately on Medicaid as opposed to non‑Medicaid services. Under the proposed federal regulations, the federal government would add additional, nonstatistical tests beyond the existing statistical test to determine whether a health care‑related tax falls too disproportionately on Medicaid services. These additional tests would effectively prohibit health care‑related taxes that place different tax rates on taxpayers based on their levels of Medicaid (versus non‑Medicaid) activity. In addition, the new federal rule would give the federal government significant discretion—beyond the tests—to determine whether a proposed health care‑related tax places an undue burden on Medicaid as opposed to non‑Medicaid services.
What is the difference between brand name and generic?
A “brand‑name” drug is a drug that is sold under a trademarked name. Brand‑name drugs are often “innovator” drugs that enjoy patent protection, which prohibits nonowners of the patent from manufacturing and selling the drug without the owner’s consent. As such, brand‑name drugs are often single‑source drugs, meaning that the patent owner has no competitors offering an identical drug for sale within the drug market. A generic drug is a non‑brand‑name drug that is made with the same chemical combination as a currently or formerly available brand‑name drug that has had its patent and exclusivity period expire (usually after roughly 15 years of coming to market). Typically, generic drugs are multiple‑source drugs where multiple manufacturers compete to produce and sell drugs made of identical chemical combinations. Because brand‑name drugs often do not face any marketplace competition, they tend to be significantly more expensive than generic drugs.
Does DHCS use Medi-Cal?
In addition, DHCS uses the Medi‑Cal program’s purchasing power to negotiate state supplemental rebates from drug manufacturers on top of the federally required rebates, but primarily only for prescription drugs paid for through FFS. Both types of rebates lower the final cost of prescription drugs.
Is Medi-Cal a state or federal program?
Medi‑Cal, the state’s Medicaid program, is administered by the Department of Health Care Services (DHCS) and provides health care coverage to almost 13 m illion of the state’s low‑income residents. Coverage is cost‑free for most Medi‑Cal enrollees. Instead, Medi‑Cal costs generally are shared between the federal, state, and local (county) governments.
Does Medi-Cal cover pharmacy services?
Medi‑Cal Covers Pharmacy Services, Predominantly Through Managed Care . Under its pharmacy services benefit, Medi‑Cal covers prescription drugs and other medical products obtained from pharmacies for the nearly 13 m illion state residents enrolled in the program. For the vast majority of Medi‑Cal recipients, Medi‑Cal pays the entire cost of covered drugs and medical products. As shown in Figure 10, most Medi‑Cal pharmacy services utilization and a majority of spending occurs through managed care. Although Medi‑Cal managed care plans currently cover and pay for most prescription drugs in Medi‑Cal, certain therapeutic classes of drugs—primarily, expensive classes of drugs, such as those for hemophilia and HIV—are carved out of managed care and instead paid for directly by the state through FFS.
Can a state continue to finance Medi-Cal?
State May Be Unable to Continue Various Financing Mechanisms Without Significant Changes. If the draft regulations were finalized in their current or similar form, many of the state’s mechanisms for financing Medi‑Cal with non‑General Fund sources would be at risk of being disallowed. For financing mechanisms that are disallowed, the Legislature would need to make a choice as to whether to replace the non‑General Fund sources with General Fund, restructure the financing mechanism (where feasible) to make it compliant with the regulations (which would likely require either the state or other entities to increase their contribution toward Medi‑Cal costs), or reduce spending in the Medi‑Cal program to account for the lost funding.