(NPs, CNSs, CNMs and CRNAs), and qualified psychologists. These practitioner services can be independently billed to Medicare and will be paid in addition to Medicares inpatient hospital payment. If these practitioners are employed by hospitals, their services remain separately billable to Medicare although
...
A doctor can be one of these:
- Doctor of Medicine (MD)
- Doctor of Osteopathic Medicine (DO)
- In some cases, a dentist, podiatrist (foot doctor), optometrist (eye doctor), or Doctor of Chiropractic (DC)
What types of doctors accept Medicare for payment?
Doctors that accept Medicare for payment fall into two categories. Those that "accept assignment" and those that do not. Every year, the Centers for Medicare and Medicaid (CMS) puts out a recommended physician fee schedule. 3 Doctors who agree to this fee schedule "accept assignment" and are called participating providers.
How do physician practitioners apply for Medicare?
Physicians and non-physician practitioners can apply for enrollment in the Medicare program or make a change in their enrollment information using either: n#TAB#The Internet-based Provider Enrollment, Chain and Ownership System (PECOS), or The paper enrollment application process (e.g., CMS-855).
Can an app bill Medicare directly to the patient?
If the APP bills directly to Medicare, with his/her name and NPI on the claim form, then the payment is reduced by to 85 percent of the MPFS allowable (a 15 percent reduction). The APP provides the entire service. The APP must be an employee of the physician/practice.
What services are covered by Medicare?
Medicare also covers services provided by other health care providers, like these: Physician assistants. Nurse practitioners. Clinical nurse specialists. Clinical social workers. Physical therapists. Occupational therapists. Speech language pathologists.

Can an NP bill Medicare?
NPs may bill Medicare Part B for services that would be considered physician services if performed by a physician, but which are performed by an NP and if that service is permitted by the NP's scope of practice. A service that does not meet Medicare's definition of a "physician service" will not be reimbursed.
Can physician assistants bill Medicare directly?
With these changes starting January 1st 2022, CMS is authorizing Medicare to make direct payments to physician assistants for services they perform under Medicare part B. As it stands right now, Medicare can only make payments to the employer or independent contractor.
What are professional services in Medicare?
Under PQRI, covered professional services are those paid under or based on the Medicare Physician Fee Schedule (PFS). To the extent that eligible professionals are providing services which get paid under or based on the PFS, those services are eligible for PQRI.
What are eligible professionals?
Eligible professional (EP) means a physician as defined in section 1861(r) of the Act, which includes, with certain limitations, all of the following types of professionals: (1) A doctor of medicine or osteopathy. (2) A doctor of dental surgery or medicine. (3) A doctor of podiatric medicine. (4) A doctor of optometry.
Can a nurse practitioner bill a consult?
Yes they can. When requested by a physician or other appropriate source, a consultation may be provided by a physician or qualified nonphysician practitioner (NPP).
Can a PA bill independently?
The PA may not independently bill for medical services. The PA may not advertise independently for their services. The PA may not pronounce a patient dead. The PA may not perform acupuncture.
Which is considered a nonphysician practitioner?
Nurse practitioners, clinical nurse specialists, and physician assistants are health care providers who practice either in collaboration with or under the supervision of a physician. We refer to them as non-physician practitioners.
How does Medicare reimburse physician services?
Traditional Medicare reimbursements Instead, the law states that providers must send the claim directly to Medicare. Medicare then reimburses the medical costs directly to the service provider. Usually, the insured person will not have to pay the bill for medical services upfront and then file for reimbursement.
Can a physician bill incident to another physician CMS?
The Centers for Medicare & Medicaid Services (CMS) has verified that a physician can bill for incident-to services rendered by another physician as long as all incident-to criteria is met.
Which healthcare professional is eligible to participate in the Medicare EHR Incentive Program?
Eligible professionals under the Medicaid EHR Incentive Program include: Physicians (primarily doctors of medicine and doctors of osteopathy) Nurse practitioner. Certified nurse-midwife.
Which of the following professionals were eligible for the Medicare EHR incentive program?
Eligible Professionals Doctors of medicine or osteopathy. Doctors of dental surgery or dental medicine. Doctors of podiatry. Doctors of optometry.
What is a Medicare eligible professional EP under meaningful use?
An EP (as defined under this section) who furnishes 90% or more of his or her covered professional services in a hospital setting in the year preceding the payment year. Meaningful EHR user (495.4):
What is Medicare application?
application is used to initiate a reassignment of a right to bill the Medicare program and receive Medicare payments (Note: only individual physicians and non-physician practitioners can reassign the right to bill the Medicare program).
What is NPI in Medicare?
The National Provider Identifier (NPI) will replace health care provider identifiers in use today in standard health care transactions. Suppliers must obtain their NPI prior to enrolling in the Medicare program. Enrolling in Medicare authorizes you to bill and be paid for services furnished to Medicare beneficiaries.
When did Medicare start covering nurse practitioners?
Medicare rules – Nurse Practitioner (NP) Services. Effective for services rendered after January 1 , 1998, any individual who is participating under the Medicare program as a nurse practitioner (NP) for the first time ever, may have his or her professional services covered if he or she meets the qualifications listed below, ...
When is NP payment effective?
Payment for NP services is effective on the date of service, that is, on or after January 1, 1998, and payment is made on an assignment-related basis only.
What is covered under Part B?
1. General. The services of an NP may be covered under Part B if all of the following conditions are met:
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.
What Do You Need to Bill and Submit Claims through CMS?
There are five things you’ll need when submitting a claim through CMS:
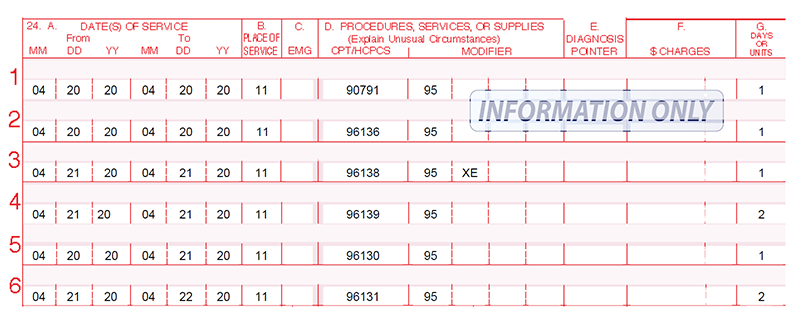
What Are CPT Codes?
Common Procedural Technology (CPT) codes are numbers assigned to every task and service a medical practitioner may provide to a patient including medical, surgical, and diagnostic services.
What Are ICD-10 Codes?
ICD-10 codes identify medical diagnoses, informing insurance companies what care you provided and why.
The Trickiness of Date of Service
While notating the date of service seems simple, it can be a bit tricky with time-related programs (CCM, RPM, BHI).
How Care Management Software Helps Ease the Billing and Claim Submission Process
Where most practitioners get tripped up in the billing and claim submission process is with assigning proper CPT and ICD-10 codes.
How ThoroughCare Simplifies the Billing Process
ThoroughCare is a care management software that is known to provide extensive tools to help practitioners successfully manage these programs.
What happens if a doctor doesn't accept Medicare?
If your doctor does not accept Medicare for payment, then you could be in trouble. In the case of a true medical emergency, he is obligated to treat you. Outside of that, you will be expected to pay for his services out of pocket. This can get expensive quickly.
How many doctors opted out of Medicare in 2010?
That means he agrees to accept Medicare as your insurance and agrees to service terms set by the federal government. 1 . In 2010, only 130 doctors opted out of Medicare but the number gradually increased each year, until it reached a high of 7,400 in 2016.
What is the limiting charge for Medicare?
Medicare has set a limit on how much those doctors can charge. That amount is known as the limiting charge. At the present time, the limiting charge is set at 15 percent, although some states choose to limit it even further. This charge is in addition to coinsurance. 5 Doctors who charge more than the limiting charge could potentially be removed ...
How much money was lost in Telemedicine fraud?
Federal indictments & law enforcement actions in one of the largest health care fraud schemes involving telemedicine and durable medical equipment marketing executives results in charges against 24 individuals responsible for over $1.2 billion in losses. Updated April 9, 2019.
Is preventive screening free?
Some preventive screening tests are free to you when you receive care through a participating provider. The rest of the time, Medicare pays 80 percent of the recommended cost and you pay a 20 percent coinsurance. 10 . Understanding how the system works will help you to make the most of your dollars.
Does Medicare cover non-participating doctors?
Medicare will cover 100 percent of the recommended fee schedule amount for participating providers but only 95 percent for non-participating providers.
Can non-participating suppliers charge you for medical equipment?
Sadly, the limiting charge only extends to healthcare providers. Non-participating suppliers of medical equipment, meaning they do not "accept assignment" or agree to the fee schedule, can charge you as much as they want. 6 This is the case even if the doctor who prescribed that equipment accepted assignment.
What are the three types of NPP billing?
Perform other services within the state scope of practice (state laws and regulations). For CMS, there are three types of NPP billing: Incident-to. Split/shared.
Who must be in the same office suite as the APP?
There must be a physician in the same office suite as the APP who is immediately available to provide assistance or direction to the APP. The APP must be employed, leased, or serving as an independent contractor of the physician or group, or a legal entity that employs or contracts the physician .
Can a physician see a patient and document a visit?
Usually one practitioner sees the patient and documents a note, and either the physician or APP follow up later on the same date, seeing the patient and documenting a visit note. Both visits can be combined and billed under the physician’s NPI number, which is most advantageous.
Is it better to bill under a physician or NPP?
It is more advantageous to bill under the physician, who is paid at 100 percent of the fee schedule allowable. The NPP and a physician share a visit, each performing and documenting a portion of the history, exam, and medical decision-making. The documentation may then be combined to arrive at a level of service.
Can an APP bill an incident to?
An APP may not bill incident-to for evaluation or management of a new patient or established patient with a new or worsening problem. Even though it is not required, it is recommended that the physician supervising co-sign the APP’s documentation to validate the incident-to service.
Can a private physician bill a shared visit?
A shared service between a hospital-employed APP and a private physician may not be billed as a shared visit. The physician may report the service that he/she performed and documented, but may not use the hospital employed APP’s documentation to determine the level of service.
Who is Deborah Grider?
Deborah Grider has 35 years of industry experience and is a recognized national speaker, consultant, and American Medical Association author who has been working with ICD-10 since 1990 and is the author of Preparing for ICD-10, Making the Transition Manageable, Principles of ICD-10, the ICD-10 Workbook, Medical Record Auditor, and Coding with Modifiers for the AMA. She is a senior healthcare consultant with Karen Zupko & Associates. Deborah is also the 2017 American Health Information Management Association (AHIMA) Literacy Legacy Award recipient. She is a member of the ICD10monitor editorial board and a popular panelist on Talk Ten Tuesdays.
