How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
How much will Medicare cost in 2021?
Most people don't pay a monthly premium for Part A (sometimes called " premium-free Part A "). If you buy Part A, you'll pay up to $471 each month in 2021. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $471. If you paid Medicare taxes for 30-39 quarters, the standard Part A premium is $259.
How long does a SNF benefit last?
The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins. You must pay the inpatient hospital deductible for each benefit period. There's no limit to the number of benefit periods.
How much is the Part B premium for 91?
Part B premium. The standard Part B premium amount is $148.50 (or higher depending on your income). Part B deductible and coinsurance.
How long do you have to pay late enrollment penalty?
In general, you'll have to pay this penalty for as long as you have a Medicare drug plan. The cost of the late enrollment penalty depends on how long you went without Part D or creditable prescription drug coverage. Learn more about the Part D late enrollment penalty.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
How much does Medicare typically cost?
Medicare protects people aged 65 and older and younger people with disabilities from financial hardship by providing health insurance. But it comes with out-of-pocket costs. How much Medicare costs depends on how each individual uses it and the choices they make about coverage.
How much does the average Medicare beneficiary spend out of pocket?
What you spend out of pocket may be totally different than what a family member or friend with Medicare pays. But, on average, people spend more than $5,000 out of pocket annually — or more than $400 per month — on their Medicare costs, according to the Kaiser Family Foundation (KFF).
What do you pay with Medicare Part A?
If you go to the hospital, after paying your Part A deductible, inpatient hospital care is covered under the following conditions:
What do you pay with Medicare Part B?
Unlike Part A, qualified Medicare enrollees must pay a monthly premium for Part B.
What is observation status, and how does it affect your Medicare costs?
A confusing and potentially costly scenario that some hospitalized patients encounter is what’s called observation status. Even though you’re at the hospital, you may sometimes still be considered an outpatient for the first day or two (or longer in extraordinary cases).
What do you pay for Medicare drug coverage (Part D)?
You’ll want to consider additional coverage for medications if you don’t already have coverage of equal value. You do this to avoid the Part D late enrollment penalty. You can buy a Medicare Part D plan — while keeping Parts A and B — or a Medicare Advantage plan instead.
Medigap: Covering your out-of-pocket costs
With original Medicare, there’s no annual out-of-pocket maximum. So if you need a lot of care, your out-of-pocket costs can add up. For that reason, about half of Medicare enrollees have supplemental coverage. Some get it through their employer, others have Medicaid, and many use Medicare supplement insurance known as Medigap.
What happens if you don't enroll in Medicare?
If you don’t enroll in a Medicare drug plan when you’re first eligible, you may pay a late enrollment penalty if you join a plan later. You’ll have to pay this penalty for as long as you have Medicare prescription drug coverage. However, you won’t pay a penalty if you get Extra Help or other eligible prescription drug plan coverage.NOTE: The Medicare prescription drug plan late enrollment penalty is different than the Medicare Part B late enrollment penalty. If you don’t enroll in Part B when you’re first eligible for it, you may have to pay a late enrollment penalty for as long as you have Part B coverage. Also, you may have to wait to enroll, which will delay Part B coverage.
Do you have to pay late enrollment penalty for Part B?
when you’re first eligible for it, you may have to pay a late enrollment penalty for as long as you have Part B coverage. Also, you may have to wait to enroll, which will delay Part B coverage.
Do you have to assist someone with the application for Medicare?
with their Medicare prescription drug plan costs. If you assist someone with the application, you must
How long does Medicare cover ESRD?
If you're entitled to Medicare only because of ESRD, your Medicare coverage ends 36 months after the month of the kidney transplant.
What happens if you get a drug that Part B doesn't cover?
If you get drugs that Part B doesn’t cover in a hospital outpatient setting, you pay 100% for the drugs, unless you have Medicare drug coverage (Part D) or other drug coverage. In that case, what you pay depends on whether your drug plan covers the drug, and whether the hospital is in your plan’s network. Contact your plan to find out ...
What is formulary in insurance?
If you have drug coverage, check your plan's. formulary. A list of prescription drugs covered by a prescription drug plan or another insurance plan offering pre scription drug benefits. Also called a drug list. to see what outpatient drugs it covers. Return to search results.
Does Medicare pay for osteoporosis?
Injectable osteoporosis drugs: Medicare helps pay for an injectable drug if you’re a woman with osteoporosis who meets the criteria for the Medicare home health benefit and has a bone fracture that a doctor certifies was related to post-menopausal osteoporosis.
Does Medicare cover transplant drugs?
Medicare covers transplant drug therapy if Medicare helped pay for your organ transplant. Part D covers transplant drugs that Part B doesn't cover. If you have ESRD and Original Medicare, you may join a Medicare drug plan.
Does Medicare cover infusion pumps?
Drugs used with an item of durable medical equipment (DME) : Medicare covers drugs infused through DME, like an infusion pump or a nebulizer, if the drug used with the pump is reasonable and necessary.
Does Medicare pay for nutrition?
Parenteral and enteral nutrition (intravenous and tube feeding): Medicare helps pay for certain nutrients if you can’t absorb nutrition through your intestinal tract or take food by mouth.
What is the second most popular Medicare plan?
Medigap Plan G is, in fact, the second-most popular Medigap plan. 17 percent of all Medigap beneficiaries are enrolled in Plan G. 2. The chart below shows the average monthly premium for Medicare Supplement Insurance Plan G for each state in 2018. 3.
Which states have the lowest Medicare premiums?
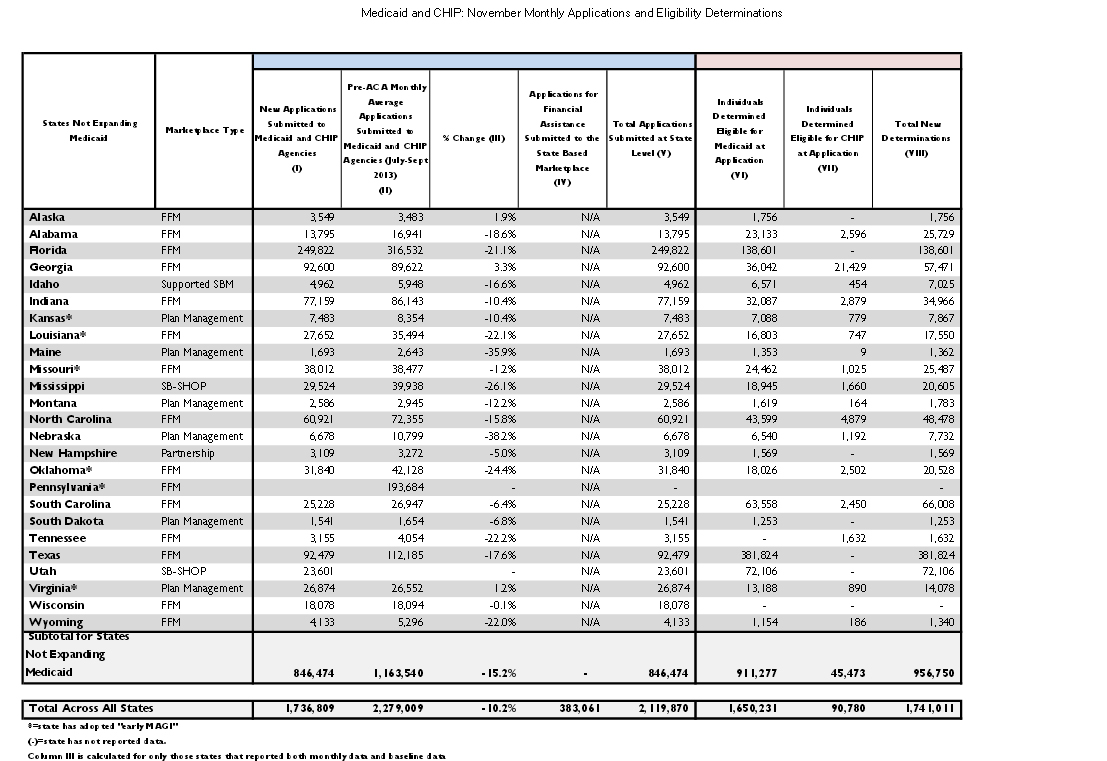
Florida, South Carolina, Nevada, Georgia and Arizona had the lowest weighted average monthly premiums, with all five states having weighted average plan premiums of $17 or less per month. The highest average monthly premiums were for Medicare Advantage plans in Massachusetts, North Dakota and South Dakota. *Medicare Advantage plans are not sold in ...
How to contact Medicare Advantage 2021?
New to Medicare? Compare Medicare plan costs in your area. Compare Plans. Or call. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 to speak with a licensed insurance agent.
What Determines Medicare Part D Premiums?
Medicare Part D premiums are the monthly fee you pay for coverage. Medicare Part D prescription drug plans are sold by private insurance companies that contract with Medicare.
What Is the Medicare Part D Deductible?
The Medicare Part D deductible is the amount of money you have to pay out of your own pocket for your prescriptions each year before your prescription drug plan starts paying its share.
Medicare Part D Copays and Coinsurance
Once you pay your Medicare Part D deductible, you will only pay a portion of the cost for your prescriptions for the rest of the year. These payments will be in the form of either a copayment or coinsurance.
Help Covering Medicare Part D Costs
If you have limited income and resources, a program called Extra Help may be able to help you with Medicare Part D prescription drug costs, including premiums, coinsurance and your deductible.
How much does myalept cost?
Myalept is self-administered once a day, and patients typically use 14 vials per month at a list price of $5,297 per vial. Since Myalept is the only option to control this rare condition, there are no more affordable drugs available. Myalept increased in price this February, from $71,306 to $74,159 per year.
What is list price?
List price is the price of a drug that is set by the manufacturer. Prices reflect list prices for each medication's most common 30-day prescription. *Quantity of dose may depend on weight or body surface area of the individual, meaning that list price can vary. Prices shown are for a typical patient being treated with the medication.
How much does Acthar cost?
Seventeen years and one new manufacturer later, the list price for one vial of Acthar (a typical monthly supply) now runs at $39,864.
How much is Cinryze?
Manufactured by Takeda, Cinryze has a list price of $45,465 for a typical one-month supply of 16 vials. Cinryze is used to treat hereditary angioedema, a rare, life-threatening genetic condition that causes swelling in various parts of the body including the hands, face, and throat. Takeda increased the price for one vial of Cinryze from $2,759 to $2,842 in January.
Do drugs in the top 20 continue to increase?
The majority of drugs in the top-20 list continue to undergo annual price increases.
Can you get financial assistance through Horizon?
For those looking to save, patients may be able to get financial assistance through Horizon Patient Services.
How many people are in Medicare Advantage?
22 million Medicare beneficiaries (34% of all Medicare enrollees) are enrolled in a type of private Medicare plan called a Medicare Advantage plan. Another 20.6 million are enrolled in a stand-alone Medicare prescription drug plan (PDP).
How many stars does Medicare have?
Quality is important to consumers, and in eight states, at least 75% of their MAPD plans score four stars or better for quality measures by the Centers for Medicare and Medicaid Services.
How many MAPD plans are there in Washington?
Also, there are 118 MAPD plans available in Washington (the average is 62 per state), and nearly 70% of all MAPD plans in Washington are ranked 4 stars or higher by Medicare (the average is 59% of plans in each state).
How much is the PDP premium in Nevada in 2021?
The average PDP premium in Nevada is $38.17 in 2021 ($3 lower than the national average), and the average PDP deductible is $349.83 ($7 higher than the national average). 23% of the state's PDPs were rated 4 stars or higher by Medicare, which is well above the national average of 12% of plans per state.
How much does Medicare Part D cost?
Medicare Part D Prescription Drug Plan beneficiaries in the state pay an average monthly premium of $37.84 for their drug coverage. This dollar amount is right around the national average, and the average PDP deductible is roughly $44 higher than the national average at $366.80.
How much is the MAPD deductible?
The $137.50 average MAPD drug deductible is some $30 lower than the nationwide average. This general affordability of plans is in addition to having 65% of the state’s plans being rated four stars or higher for quality by Medicare, which is comfortably above the national average of 59%.
What is the MAPD premium for 2021?
The average MAPD premium in 2021 is $41.27 (around $8 higher than the national average), and the average MAPD drug coverage deductible is $169.15 for the year, which is very close to the national average. 69% of Vermont MAPD plans are rated 4 stars or higher by Medicare.
Who said patients should have access to the lowest price possible at the pharmacy?
Daniel Nam , executive director of federal programs at America’s Health Insurance Plans, a trade group, agreed that “patients should have access to the lowest price possible at the pharmacy.” But he said Medicare’s warning, contained in a letter this month, takes aim at an increasingly rare occurrence. Gag order clauses are “not something they are incorporating into their contracts,” he said.
Does Medicare mention annual handbook?
But details may be hard to find: Medicare’s website and annual handbook don’t mention it.
Do insurers punish pharmacists for violating gag orders?
Kala Shankle, policy and regulatory affairs director for the National Community Pharmacists Association, which represents 22,000 independent pharmacies, said insurers have punished pharmacists who violate gag orders by dropping them from the plan’s network.
Is gag order a typical pharmacy benefit?
Pharmacy benefit managers also said gag orders are not typical. “If it is happening, it is very much an outlier,” said Mark Merritt, president and CEO of the Pharmaceutical Care Management Association.
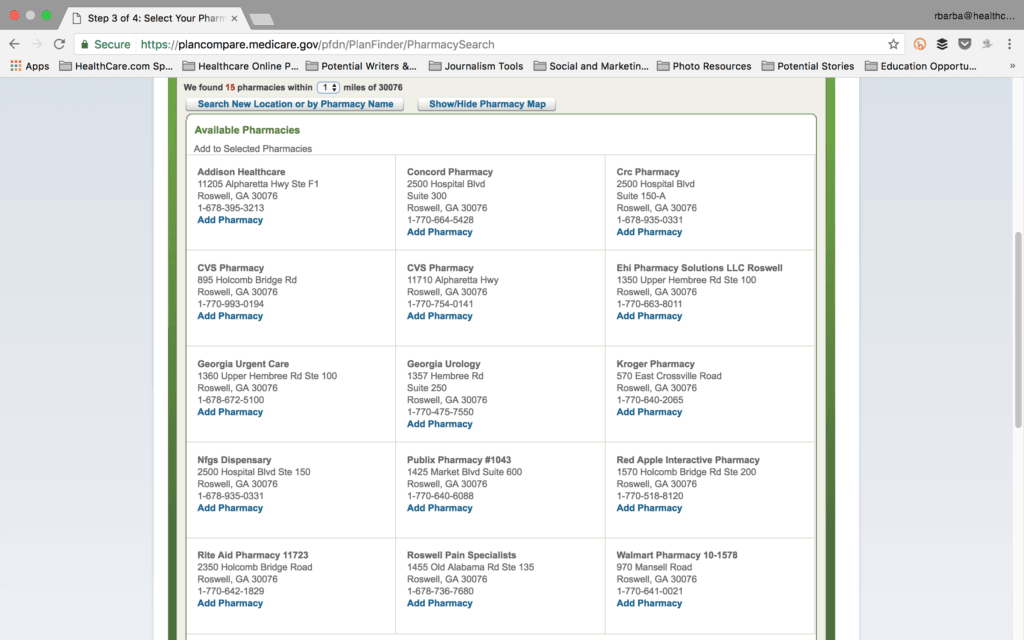
Can Medicare overpay for prescriptions?
That doesn’t mean people with Medicare drug coverage are destined to overpay for prescriptions . Under a little-known Medicare rule, they can pay a lower cash price for prescriptions instead of using their insurance. But first, they must ask the pharmacist about that option, said Julie Carter, federal policy associate at the Medicare Rights Center, a patient advocacy group.