Does Medicare cover therapeutic services?
· If you are enrolled in Original Medicare (Part A and Part B) and your doctor recommends counseling for a mental health condition, these services are generally covered by Medicare both on an inpatient and outpatient basis. Your Medicare Part A and B deductibles, copays and coinsurance amounts may apply.
How much does Medicare pay for outpatient therapy?
· Medicare is a federal insurance program for people aged 65 and older or those below age 65 with specific health conditions. Medicare does provide coverage for therapy, as well as for other mental...
Does Medicare cover outpatient psychiatric treatment?
This law included two provisions related to Medicare payment for outpatient therapy services including physical therapy (PT), speech-language pathology (SLP), and occupational therapy (OT) services: Section 50202 of the BBA of 2018 repeals application of the Medicare outpatient therapy caps and its exceptions process while adding limitations to ensure payment for …
What does Medicare cover for mental health services?
You can call and speak with a counselor 24 hours a day, 7 days a week. Call 911 if you're in immediate medical crisis. Medicare Part B (Medical Insurance) helps pay for these outpatient mental health services: One depression screening per year.
Can Medicare be used for therapy?
Mental health and Medicare: Therapy coverage. Medicare pays for both inpatient and outpatient mental health care, including the cost of therapy. Some out-of-pocket expenses may apply. Medicare is a federal insurance program for people aged 65 and older or those below age 65 with specific health conditions.
Can a therapist bill Medicare?
Medicare currently recognizes psychiatrists, psychologists, clinical social workers and psychiatric nurses for outpatient mental health services. However, Medicare does not reimburse professional counselors for behavioral health services.
What are the 4 parts of the Medicare program?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Does Medicare reimburse me for psychotherapy?
Yes, Medicare covers mental health care, which includes counseling or therapy. Depending on your needs, mental health care can be provided in a variety of settings.
Is mental health covered by Medicare?
You must have Medicare Part B to be covered for outpatient mental health treatment, partial hospitalization, and annual depression screenings. Like inpatient care, Medicare will cover most of your outpatient treatment services but there are certain financial requirements you must meet before Medicare will pay.
How Much Does Medicare pay for 90837?
$132.69What is the difference between the “facility rate” and “nonfacility rate” for telehealth services?CodeService2021 Facility Rate90832Psychotherapy 30-minutes$68.7490837Psychotherapy 60-minutes$132.6996132Neuropsych Test Eval$106.0896158Hlth Bhvr Intrv Indvl$58.971 more row•Dec 10, 2021
What is the difference between Medicare A and B?
Part A (Hospital Insurance): Helps cover inpatient care in hospitals, skilled nursing facility care, hospice care, and home health care. Part B (Medical Insurance): Helps cover: Services from doctors and other health care providers.
What is the difference between Medicare Part C and D?
Medicare Part C is an alternative to original Medicare. It must offer the same basic benefits as original Medicare, but some plans also offer additional benefits, such as vision and dental care. Medicare Part D, on the other hand, is a plan that people can enroll in to receive prescription drug coverage.
What is Medicare Part B also known as?
Medicare Part B (also known as medical insurance) is an insurance plan that covers medical services related to outpatient and doctor care.
How many psychology sessions are under Medicare?
As such, Medicare rebates are available for psychological treatment by registered psychologists. Under this scheme, individuals diagnosed with a mental health disorder can access up to 10 individual Medicare subsidised psychology sessions per calendar year. As of October 9, 2020 this has been doubled to 20.
How much does Medicare cover for psychology?
Currently, the Medicare rebate is $129.55 per session with a Clinical Psychologist for up to 10 sessions per calendar year. Due to COVID-19, Medicare has approved an additional 10 sessions per calendar year for 2021, which means clients can potentially access up to 20 sessions per calendar year.
Does Medicaid cover therapy?
According to MentalHealth.gov, mental health services covered by Medicaid often include counseling, therapy, medication management, social work services, peer support and substance use disorder treatment. Since depression is a mental health issue, counseling can be covered if you qualify.
What does Medicare Part A pay for?
Medicare Part A pays for inpatient care a person receives when they are admitted to either a general or psychiatric hospital.
What is the difference between Medicare Part A and Part B?
Medicare Part A helps cover the hospitalization costs of mental health care, whilst Part B helps pay for therapy and partial hospitalization costs.
What is mental health?
A person’s mental health includes their mental, emotional, and social well-being. These functions affect feelings, thoughts, and actions, including how a person manages stress and makes friends. Mental health is important in every stage of life, and life events can trigger both physical and emotional responses.
How many reserve days do you have to use for Medicare?
all costs after lifetime reserve days have been used in full. A person has 60 lifetime reserve days to use during their lifetime. In Part B, there are out-of-pocket costs for diagnosis and treatment. A person must pay 20% of the Medicare-approved amount after the Part B deductible is met.
Does Medicare cover transportation?
During partial hospitalization Medicare does not cover: meals. transport. support groups (group therapy is covered) job skills testing or training that is not part of treatment. Medicare parts A and B do not cover prescribed medication taken at home, but a person can use Medicare Part D to help pay for these costs.
Does Medicare pay for depression screening?
Part B coverage. Medicare Part B pays for one depression screening each year. The screening must happen in the office of a primary care doctor or similar to ensure there is appropriate follow-up care. Part B also pays for single or group therapy by state-licensed experts.
What is a Medicare preventive visit?
When a person first enrolls in Medicare, they receive a Welcome to Medicare preventive visit. During this visit, a doctor reviews risks of depression. Yearly wellness visits can then include discussions with a person’s doctor on any changes to mental health that may have occurred since the last visit.
Spotlight
The Therapy Services webpage is being updated, in a new section on the landing page called “Implementation of the Bipartisan Budget Act of 2018”, to: (a) Reflect the KX modifier threshold amounts for CY 2021, (b) Add more information about implementing Section 53107 of the BBA of 2018, and (c) Note that the Beneficiary Fact Sheet has been updated.
Implementation of the Bipartisan Budget Act of 2018
This section was last revised in March 2021 to reflect the CY 2021 KX modifier thresholds. On February 9, 2018, the Bipartisan Budget Act of 2018 (BBA of 2018) (Public Law 115-123) was signed into law.
Other
On August 16, 2018, CMS issued a new Advance Beneficiary Notice of Noncoverage (ABN) Frequently Asked Questions (FAQ) document to reflect the changes of the Bipartisan Budget Act of 2018. Please find the document in the below Downloads section titled: “August 2018 ABN FAQs”.
What is a health care provider?
health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. to diagnose or treat your condition.
What is Medicare preventive visit?
A one-time “Welcome to Medicare” preventive visit. This visit includes a review of your possible risk factors for depression. A yearly “Wellness” visit. Talk to your doctor or other health care provider about changes in your mental health. They can evaluate your changes year to year.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. applies. If you get your services in a hospital outpatient clinic or hospital outpatient department, you may have to pay an additional. copayment.
Do you pay for depression screening?
You pay nothing for your yearly depression screening if your doctor or health care provider accepts assignment. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is Part B?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. helps pay for these outpatient mental health services: One depression screening per year. The screening must be done in a primary care doctor’s office or primary care clinic that can provide follow-up treatment and referrals. ...
Can you do individual and group psychotherapy with a doctor?
Individual and group psychotherapy with doctors or certain other licensed professionals allowed by the state where you get the services.
What is part B in physical therapy?
Physical therapy. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine. outpatient physical therapy.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B deductible applies.
What is Medicare Part A?
Medicare Part A and inpatient mental health care. Medicare Part A (hospital insurance) helpscover inpatient mental health services in either a general hospital or apsychiatric hospital. Medicare uses benefit periods to measure your use of hospital services. A benefit period starts the day of inpatient admittance and ends after 60 days in a row ...
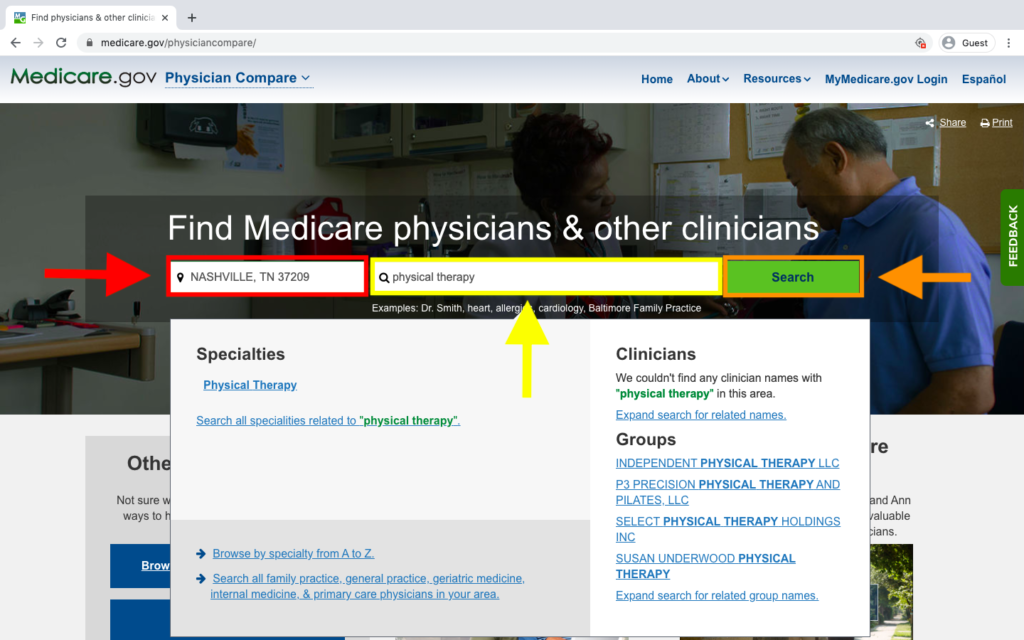
How to find a doctor who accepts Medicare?
You may want to visit the Centers for Medicare and Medicaid Services’ Physician Compare, to find a doctor who accepts Medicare services. A list of professionals or group practices in the specialty and geographic area you specify, along with detailed profiles, maps, and driving directions are available.
What is the purpose of reviewing details about the type and extent of coverage with your provider?
Be sure to review details about the type and extent of coverage with your provider to determine which particular services are covered and to what degree.
Do mental health insurance plans cover all medications?
Most plans have a list of drugs the plan covers. Although these plans are not required to cover all medications, most are required to cover medications which may be used for mental health care, such as: antidepressants. anticonvulsants.
What is a good opportunity to speak with your doctor about your mental health?
yearly wellness visits (which are a good opportunity to speak with your doctor about your mental health)
Does Part B pay for coinsurance?
Although coinsurance and deductibles may apply , Part B also helps pay for such services as:
How long can you be in a mental hospital?
For general hospitals, there’s no limit to the number of benefit periods you can have for mental health care. In a psychiatric hospital, you have a 190-day lifetime limit.
What does a therapist do?
Many therapists use a combination of skills and techniques to help you achieve relief from your symptoms and improve your day-to-day function. In the course of a session, these techniques may not be specified, and you may not notice any difference from one style of therapy to the next unless your therapist makes it clear what style they’re operating under for your session.
What is the most common form of therapy?
The most common forms of therapy include: Cognitive behavioral therapy . CBT has broad applicability and focuses on the personalized development of effective coping skills to counteract harmful patterns of thought and behaviors. Dialectical behavior therapy.
What is supportive therapy?
Supportive therapy. This patient-led style of therapy encourages you to identify personal obstacles and the resources necessary to help you overcome them. The therapist provides guidance and information to help you structure a plan and maintain your goals.
Which is more intense, psychoanalysis or supportive therapy?
Both of these techniques focus on your childhood and past experiences in order to illustrate deeply ingrained behaviors and beliefs that contribute to mental illness or emotional difficulties. Psychoanalysis is the more intense of the two styles and may involve several sessions in a week. Supportive therapy.
What is interpersonal therapy?
Interpersonal therapy. IPT helps you adjust to difficult or new circumstances as it relates to your social experiences and relationships with others. This can involve practicing important communication skills and developing better situational awareness.
What is psychotherapy?
As described by the American Psychiatric Association (APA), psychotherapy uses a number of techniques to help patients improve their mental health by addressing troublesome behaviors and emotional difficulties.
Does Medicare Supplement cover mental health?
Medigap (Medicare Supplement) plans may help reduce any cost-sharing expenses related to mental healthcare, but these are provided by private insurers and differ from state to state. Medicare Advantage plans are required to provide the same Part A and Part B benefits as Original Medicare, but many provide additional coverage.
How often does a PTA therapist have to reassess?
In addition to supervising the services provided by the PTA, the qualified therapist is still responsible for the initial assessment, plan of care, maintenance program development and modifications, and reassessment every 30 days. See more on Medicare payment for home health.
Does Medicare cover skilled maintenance therapy?
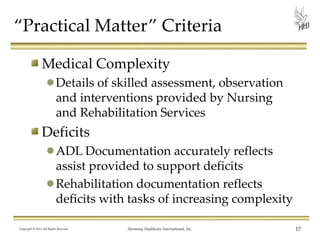
Medicare Coverage Issues. Skilled Maintenance Therapy Under Medicare. Medicare does indeed cover services to maintain or manage a beneficiary's current condition when no functional improvement is possible. There has been a longstanding myth that Medicare does not cover services to maintain or manage a beneficiary's current condition ...
Can a PTA work with Medicare?
PTs — and PTAs — are permitted to provide maintenance therapy services under Medicare Part A in home health and skilled nursing facility settings and across Part B settings. For Part A settings: Physical therapist assistants under the supervision of the PT are permitted to perform both rehabilitative and maintenance therapy services under a maintenance program established by a qualified therapist under the Medicare Part A home health or SNF benefit, if acting within the therapy scope of practice defined by state licensure laws. In addition to supervising the services provided by the PTA, the qualified therapist is still responsible for the initial assessment, plan of care, maintenance program development and modifications, and reassessment every 30 days. See more on Medicare payment for home health.
Is skilled maintenance covered by Medicare?
"Medical necessity" and "maintenance" do not mean the same thing. Medical necessity is required for all services covered under Medicare, as is the requirement that the services be skilled.
Does Medicare cover a patient's current condition?
There has been a longstanding myth that Medicare does not cover services to maintain or manage a beneficiary's current condition when no functional improvement is possible. The 2013 Jimmo vs. Sebelius settlement sought to dispel this fallacy and provide clarifications to safeguard against unfair denials by Medicare contractors for skilled therapy services that aid in maintaining a patient's current condition or to prevent or slow decline.
Is maintenance therapy necessary for Parkinson's?
When considering a patient for a maintenance program, it is not essential that they have a chronic, progressive diagnosis. Coverage is based on individualized assessment of the patient's condition and the need for skilled care to carry out a safe and effective maintenance program. In fact, the therapist can develop a maintenance program from the findings in an initial evaluation, such as for a patient with a chronic diagnosis of Parkinson disease. It is not necessary to establish rehabilitation or restorative therapy prior to the maintenance program, as long as the documentation justifies the need for skilled therapy to maintain function, or prevent or slow deterioration. Skilled maintenance therapy is covered in cases in which needed therapeutic interventions require a high level of complexity.
How much does Medicare pay for assistant surgery?
Paid only on assignment basis ● Paid at 85% of amount physician gets under Medicare PFS ● Medicare directly pays you for assistant-at- surgery services at 85% of 16% of the amount a physician gets under Medicare PFS
How long does Medicare cover IPF?
Medicare covers IPF patients for psychiatric conditions in specialty facilities for 90 days per illness with a 60-day lifetime reserve, and for 190 days of care in freestanding psychiatric hospitals (this 190-day limit doesn’t apply to certified psychiatric units). There are no further benefits once a patient uses 190 days of psychiatric hospital care.
Does Medicare cover CSW?
Legally authorized to practice medicine in the state where you provide services ● Medicare PFSMedicare doesn’t statutorily preclude the services, and they’re reasonable and necessary ● You provide services to diagnose and treat mental illnesses ● Medicare doesn’t pay CSW services to hospitalized patients with no CSW services coverage ● Medicare covers hospital outpatient CSW services and pays under the CSW benefit when billed by the hospital under CSW’s National Provider Identifier ● Medicare doesn’t cover CSW services to patients under PHP by a hospital outpatient department or Community Mental Health Center ● Medicare doesn’t cover CSW services to SNF inpatients and patients in Medicare-participating End-Stage Renal Disease facilities, or pay them under the CSW benefit if the services meet the respective participation requirements ● Medicare may cover incident to services CSWs provide for physicians, CPs, CNSs, NPs, PAs, or CNMs ● Medicare doesn’t cover services incident to your personal professional services ●
Does Medicare preclude medical services?
medicine in the state where you provide services ● Medicare doesn’t statutorily preclude the services, and they’re reasonable and necessary ● If the patient consents, you must attempt to consult their attending or primary care physician about provided services and either:
Does Medicare recognize BHI?
Medicare recognizes these Part B providers as eligible to provide diagnostic and BHI or SBIRT
What are health supplemental benefits?
health supplemental benefits may address areas like coping with life changes, conflict resolution, or grief counseling, all offered as individual or group sessions.
Does Part B cover self-administering?
but Part B covers some medications patients can’t self-administer. For other prescription coverage,