What plan provides both Medicare and Medicaid coverage?
What are dual health plans? Dual health plans are designed just for people who have both Medicaid and Medicare. They're a special type of Medicare Part C (Medicare Advantage) plan. Dual health plans combine hospital, medical and prescription drug coverage.Jan 17, 2020
When the patient is covered by both Medicare and Medicaid what would be the order of reimbursement?
Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
What are the benefits of Medicare?
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
What does Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Can I have both Medicare and Medicaid?
Some Americans qualify for both Medicare and Medicaid, and when this happens, it usually means they don't have any out-of-pocket healthcare costs. Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (about 12.3 million people).
Will Medicaid pay for my Medicare Part B premium?
Medicaid can provide premium assistance: In many cases, if you have Medicare and Medicaid, you will automatically be enrolled in a Medicare Savings Program (MSP). MSPs pay your Medicare Part B premium, and may offer additional assistance.
Can you switch back and forth between Medicare and Medicare Advantage?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
What are the advantages and disadvantages of Medicare and Medicaid?
The advantages of Medicare include cost savings and provider flexibility. Among the disadvantages are potentially high out-of-pocket costs. Once you qualify for Medicare, you have several options when it comes to enrolling in a plan.Jan 20, 2022
Is Medicare free for seniors?
You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and paid Medicare taxes for at least 10 years. You can get Part A at age 65 without having to pay premiums if: You are receiving retirement benefits from Social Security or the Railroad Retirement Board.
Does Medicare pay for food?
Medicare Part B (medical insurance) typically does not include home delivered meals or personal care as part of its home health service coverage. However, some Medicare Advantage plans may cover meal delivery service and transportation for non-medical needs like grocery shopping.
Does Medicare cover dental?
Dental services Medicare doesn't cover most dental care (including procedures and supplies like cleanings, fillings, tooth extractions, dentures, dental plates, or other dental devices). Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
Does Medicare Part A and B cover 100 percent?
All Medicare Supplement insurance plans generally pay 100% of your Part A coinsurance amount, including an additional 365 days after your Medicare benefits are used up. In addition, each pays some or all of your: Part B coinsurance.
What percentage of Medicare outlays are out of pocket?
For hospital care, only 3.1 percent was from out-of-pocket payments. The Part A program under Medicare accounts for about 70 percent of program outlays, although it is the Part B program that is responsible for about 70 percent of beneficiary liability in the form of deductibles and coinsurance under Medicare.
How many people were on medicaid in 1975?
In the past 10 years, the total number of Medicaid recipients has remained essentially the same. In 1975, there were 22.0 million recipients; in 1984, there were 21.4 million, the lowest number during this time period. The greatest number of recipients was in 1977, with 22.8 million.
What percentage of Medicare payments were in 1983?
As a percent of total Medicare payments, inpatient hospital payments in 1983 (64.6 percent) were slightly higher than in 1967; physicians’ payments in 1983 (25.6 percent) were a little less than in 1967. About 60 percent of physicians’ payments are for services to hospital inpatients.
What was the HHA rate in 1983?
HHA payments rose to 2.6 percent in 1983, from only 1.0 percent in 1967. Outpatient benefit payments, the fastest growing component of the Medicare program, rose from only 0.9 percent of Medicare benefit payments in 1967 to 6.4 percent in 1983.
What was the percentage of people seeing a doctor in 1980?
In 1980, the percent of persons seeing a physician during a year from low-, middle-, and high-income families was 76, 75, and 75 percent , respectively (National Center for Health Statistics and Health Care Financing Administration, 1980).
What was the life expectancy in 1900?
In 1900, life expectancy was only 49.2 years ; by 1984, it had increased to 74.7 years (Table 2). Declining death rates from heart disease, cerebrovascular disease, influenza, and other causes of death contributed to the growth in the elderly population (Rice and Feldman, 1983).
Why are elderly people vulnerable to changes in the health care system?
The elderly who are in poorer than average health are also vulnerable to changes in the health care system. As health care becomes oriented to a more competitive market system, insurers and providers of prepaid capitated systems may seek to enroll the healthiest and, hence, lowest users of health care resources.
What is the Medicare and Medicaid program?
Another Medicare and Medicaid program is PACE, or Programs of All-Inclusive Care for the Elderly. PACE helps older Medicare beneficiaries to seek health care within their community, in their home and at PACE facilities. Some of the things that can be covered by PACE include: Adult day primary care. Dental care.
How old do you have to be to get medicaid?
Be at least 65 years old or having a qualifying disability. Be a U.S. citizen or permanent legal resident. Be eligible for benefits through Social Security or the Railroad Retirement Board. Generally speaking, Medicaid provides health insurance to low-income individuals and families, children and pregnant women.
What is partial dual eligibility?
Partial dual eligibility includes those who receive assistance from Medicaid in order to help pay for Medicare costs such as premiums, coinsurance or deductibles. Partial dual eligibles fall into one of four categories of eligibility for Medicare Savings Programs.
What is QMB in Medicare?
Qualified Medicare Beneficiary (QMB) Program. This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance and copayments. Eligibility requires: Income of no more than $1,061 per month for an individual in 2019, or $1,430 per month for a married couple.
What is a special needs plan?
A Medicare special needs plan is a certain type of Medicare Advantage plan that is designed for people with specific health conditions or circumstances. A D-SNP is built for the specific needs of dual eligibles. All Medicare SNPs (including Medicare D-SNPs) provide prescription drug coverage.
What is an annual special enrollment period?
An annual Special Enrollment Period to enroll in a Part D plan or switch to a new one. Elimination of Part D late enrollment penalties. You automatically qualify for Extra Help if you are enrolled in Medicaid, Supplemental Security Income or a Medicare Savings Program.
Is Medicare the same as Medicaid?
Medicare eligibility is consistent for everyone across the U.S., no matter what state you live in. Medicaid is for people of any age who meet certain income qualifications. Medicaid is administered by state governments, and eligibility requirements can differ between states.
What is an appeal in Medicare?
An appeal is an action you can take if you disagree with a coverage or payment decision by Medicare, your Medicare health plan, or your Medicare drug plan. If you decide to file an appeal, ask your doctor, health care provider, or supplier for any information that may help your case. Keep a copy of everything you send to Medicare or your plan as part of the appeal.
Does Medicare cover opioids?
Counseling and therapy services are covered in person and by virtual delivery (using 2-way audio/video communication technology). Talk to your doctor or other health care provider to find out where you can go for these services. For more information, visit Medicare.gov/coverage/opioid-use-disorder-treatment- services.
Can you get help with Medicare if you have limited income?
If you have limited income and resources, you may be able to get help from your state to pay your Medicare costs (like premiums, deductibles, and coinsurance) if you meet certain conditions.
Does Medicare cover alcohol abuse?
Medicare covers one alcohol misuse screening per year for adults with Medicare (including pregnant women) who use alcohol, but don’t meet the medical criteria for alcohol dependency. If your health care provider determines you’re misusing alcohol, you can get up to 4 brief face-to-face counseling sessions per year (if you’re competent and alert during counseling). You must get counseling in a primary care setting (like a doctor’s oce).
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
What is a D-SNP?
Depending on where you live and your eligibility, you may be able to enroll in a special type of Medicare Advantage plan called a Dual-eligible Medicare Special Needs Plan (D-SNP). A D-SNP can offer benefits that Original Medicare (Parts A and B) don’t cover, such as dental, hearing, vision and more.
What services does Medicaid cover for freestanding birth centers?
Medicaid is also required to cover the following services for children: Dental care. Physical therapy. Eye care and eyeglasses.
Why is my medicaid denied?
Aside from not meeting the financial or demographic requirements, some common reasons for a denied Medicaid application include: Incomplete application or documents. Failure to respond to a request within a timely manner. Late filing.
What are optional benefits for Medicaid?
Optional benefits that may or may not be covered depending on the state include: Prescription drugs (although technically an optional benefit, every state Medicaid program provides at least some prescription drug coverage) Physical and occupational therapy . Dental and eye care for adults. Hospice. Chiropractic care. Prosthetics.
What are the disadvantages of not getting medicaid?
Some other disadvantages of Medicaid include: Eligibility differs by state, so you may not qualify where you live but otherwise would if you lived in a different state.
What is a failure to respond to a request within a timely manner?
Failure to respond to a request within a timely manner. Late filing. Disability not proven or otherwise not medically qualified. Don’t forget that mistakes can be made on behalf of Medicaid, and you have a right to appeal Medicaid’s decision concerning your coverage.
Does medicaid cover diapers?
But there are some things that Medicaid does not cover. Medicaid is not required to provide coverage for private nursing or for caregiving services provided by a household member. Things like bandages, adult diapers and other disposables are also not usually covered, and neither is cosmetic surgery or other elective procedures.
What is MMAI network?
Providers of all specialties and localities are encouraged to be part of this important initiative by joining one or more of the MMAI Plan networks. As a network provider, you will be able to provide care to new and existing Medicare-Medicaid dually eligible patients while benefitting from simpler reimbursement systems and a team-based approach to care.
What is Medicare and Medicaid alignment in Illinois?
The Illinois Medicare-Medicaid Alignment Initiative (MMAI) is a demonstration designed to improve health care for dually eligible beneficiaries in Illinois. Jointly administered by the Centers for Medicare & Medicaid Services (CMS) and the Illinois Department of Healthcare and Family Services (HFS), MMAI allows eligible beneficiaries in Illinois to receive their Medicare Parts A and B benefits, Medicare Part D benefits, and Medicaid benefits from a single Medicare-Medicaid Plan, also known as a MMAI plan. By integrating and coordinating individuals’ health care benefits, the demonstration aims to:
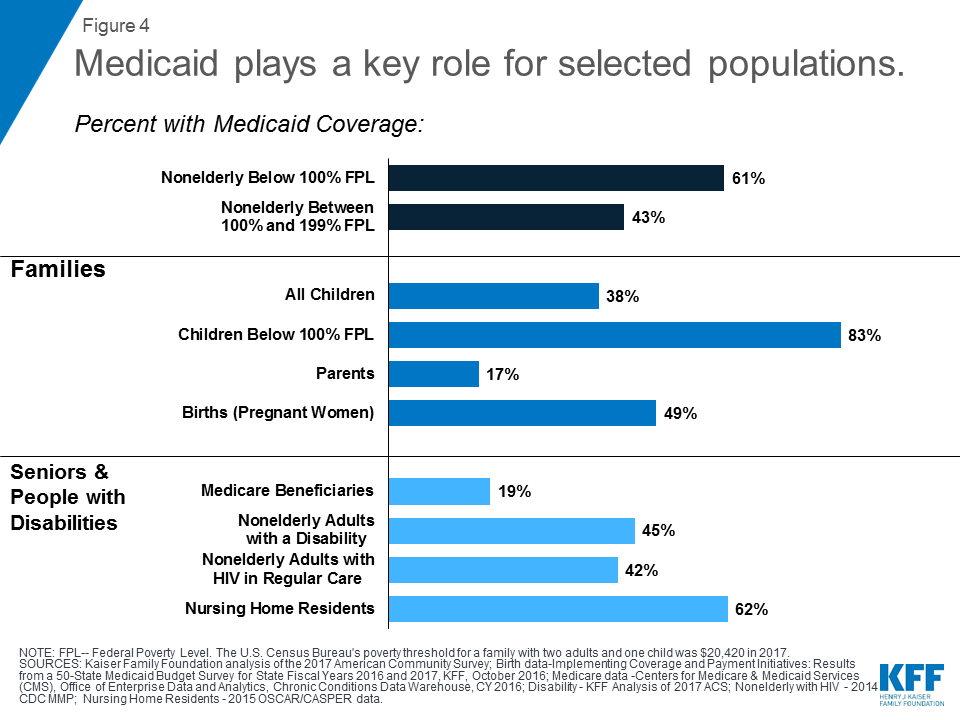
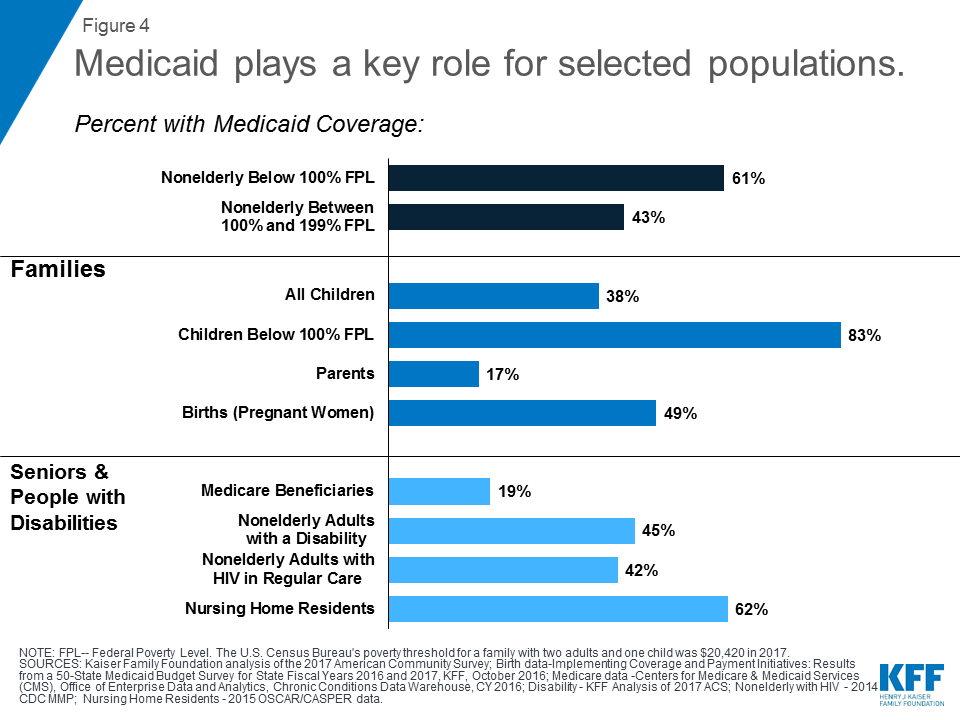
What is Medicaid coverage?
Medicaid is the single largest source of health coverage in the United States. To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, ...
How many people are covered by medicaid?
Medicaid is a joint federal and state program that, together with the Children’s Health Insurance Program (CHIP), provides health coverage to over 72.5 million Americans, including children, pregnant women, parents, seniors, and individuals with disabilities. Medicaid is the single largest source of health coverage in the United States.
What is Medicaid Spousal Impoverishment?
Spousal Impoverishment : Protects the spouse of a Medicaid applicant or beneficiary who needs coverage for long-term services and supports (LTSS), in either an institution or a home or other community-based setting, from becoming impoverished in order for the spouse in need of LTSS to attain Medicaid coverage for such services.
What is dual eligible for Medicare?
Eligibility for the Medicare Savings Programs, through which Medicaid pays Medicare premiums, deductibles, and/or coinsurance costs for beneficiaries eligible for both programs (often referred to as dual eligibles) is determined using SSI methodologies..
What is MAGI for Medicaid?
MAGI is the basis for determining Medicaid income eligibility for most children, pregnant women, parents, and adults. The MAGI-based methodology considers taxable income and tax filing relationships to determine financial eligibility for Medicaid. MAGI replaced the former process for calculating Medicaid eligibility, ...
How long does medicaid last?
Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
Does Medicaid require income?
Certain Medicaid eligibility groups do not require a determination of income by the Medicaid agency. This coverage may be based on enrollment in another program, such as SSI or the breast and cervical cancer treatment and prevention program.