
Medicare Part A
| Hospital stays (inpatient) | Examples of covered services include for ... |
| Home health services | Under Medicare Part A, home health servi ... |
| Hospice care | Medicare Part A benefits include hospice ... |
| Skilled nursing facility care | For skilled nursing facility care, Medic ... |
- Inpatient care in a hospital.
- Skilled nursing facility care.
- Nursing home care (inpatient care in a skilled nursing facility that's not custodial or long-term care)
- Hospice care.
- Home health care.
What services are covered by Medicare Part?
5 rows · Oct 16, 2021 · Medicare Part A. Covered services include (with limits and restrictions) inpatient care in ...
What is covered under Medicare Part?
What Part A covers. Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
What caregiving costs and services will Medicare cover?
Dec 10, 2019 · Part A typically covers only inpatient care. If you receive dialysis while you’re an inpatient at a Medicare-approved hospital, Part A will cover it. If you receive dialysis as an outpatient—or certain kinds of training and support for self-dialysis—you’ll need to enroll in Medicare Part B to get coverage.
What Services Medicare Part B will cover?
Services Covered by Medicare Part A & Part B. Eyeglasses (Limited) Medicare covers one pair of eyeglasses with standard frames (or one set of contact lenses) after cataract surgery that implants ... Diabetes Supplies. Diabetes screenings. Diabetes Self-Management Training. Blood. If the provider ...
What services are covered by Medicare Part A and B?
Part A (Hospital Insurance): Helps cover inpatient care in hospitals, skilled nursing facility care, hospice care, and home health care. Part B (Medical Insurance): Helps cover: Services from doctors and other health care providers.
What does Medicare Part A reimburse for?
Medicare Part A covers hospital services, hospice care, and limited home healthcare and skilled nursing care. All your Part A–related expenses are covered by Medicare if you receive them through a participating provider who accepts Medicare assignment.
What is billed under Medicare Part A?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
What's the difference between Medicare Part A and Part B?
Medicare Part A and Medicare Part B are two aspects of healthcare coverage the Centers for Medicare & Medicaid Services provide. Part A is hospital coverage, while Part B is more for doctor's visits and other aspects of outpatient medical care.
What is Medicare Part A deductible for 2021?
Medicare Part A Premiums/Deductibles The Medicare Part A inpatient hospital deductible that beneficiaries will pay when admitted to the hospital will be $1,484 in 2021, an increase of $76 from $1,408 in 2020.Nov 6, 2020
Who is eligible for Medicare Part B reimbursement?
How do I know if I am eligible for Part B reimbursement? You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B. 2.
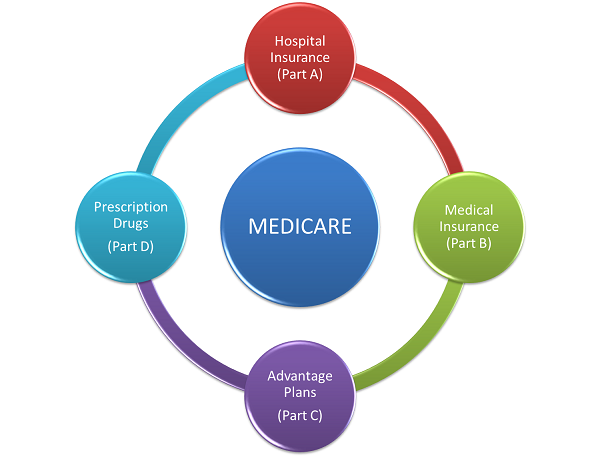
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
What is the difference between Medicare Part C and Part D?
Medicare part C is called "Medicare Advantage" and gives you additional coverage. Part D gives you prescription drug coverage.
What is covered by Medicare Part C?
What Does Medicare Part C Cover?Routine dental care including X-rays, exams, and dentures.Vision care including glasses and contacts.Hearing care including testing and hearing aids.Wellness programs and fitness center memberships.
Does Medicare Part B pay for prescriptions?
Medicare Part B (Medical Insurance) includes limited drug coverage. It doesn't cover most drugs you get at the pharmacy. You'll need to join a Medicare drug plan or health plan with drug coverage to get Medicare coverage for prescription drugs for most chronic conditions, like high blood pressure.
Is Medicare Part A and B free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.Jan 3, 2022
Do I need Part B Medicare?
Medicare Part B isn't a legal requirement, and you don't need it in some situations. In general, if you're eligible for Medicare and have creditable coverage, you can postpone Part B penalty-free. Creditable coverage includes the insurance provided to you or your spouse through work.
What services does Medicare cover?
Coverage includes many services, such as (but not limited to): Prescription drugs for pain relief and symptom management (in some cases, you may need to make a copayment) Medical, nursing, and social services. Short-term inpatient care. Homemaker services. Physical, occupational, and speech therapy.
What are covered services?
Covered services include (with limits and restrictions) inpatient care in hospitals, home health services, hospice care, and skilled nursing facility care. See the table below for an overview of Medicare Part A benefits and covered services.
What is private duty nursing?
Private-duty nursing. A television or telephone in your room (if there is a separate charge for these items) Personal care items such as razors or slipper socks. A private room, unless medically necessary. Medicare Part B covers the doctor and emergency room services you get while you are in a hospital.
Does Medicare cover home health aides?
Part-time or intermittent home health aide services. There may be limits and restrictions to these covered services, and Medicare may cover certain other home health services. Your health care provider or your hospital discharge planner can give more information, based on the details of your care plan.
What is Medicare Part B?
Medicare Part B covers the doctor and emergency room services you get while you are in a hospital. Home health services. Under Medicare Part A, home health services are generally part-time and intermittent or temporary. These services may include (but aren’t limited to):
Does Medicare cover long term care?
Medicare doesn’t cover long-term care or custodial care in this setting. Transplants.
Does Medicare cover liver transplants?
Liver. Other transplants may be covered under Medicare Part B. If your doctor decides that you need a transplant, you may want to make sure Medicare covers it first. You can ask Medicare (or your Medicare Advantage plan, if you have one), or your health provider.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is Medicare Part A?
December 10, 2019. Medicare Part A is part of Original (traditional) Medicare and constitutes the federal government’s “hospital insurance.”. In short, Part A covers costs for inpatient services in the following situations: While that sounds pretty straightforward, this part of the Medicare program causes plenty of confusion.
How much does Medicare cover for home health?
Generally, you pay $0 for home health care services and 20% of the Medicare-approved amount for medical equipment. Your home health agency should be able to tell you exactly how much Medicare will cover. Alternatively, the agency should give you a notice called the “ Home Health Advance Beneficiary Notice of Noncoverage ” before providing ...
Who is Kathryn from Baby Boomers?
Kathryn is a Medicare and geriatric specialist who has appeared on Baby Boomers, OppLoans, and Best Company. Her readers don’t need a degree in government-speak to get the right coverage because Kathryn sifts through Medicare’s parts, plans, and premiums to distill only the most useful information. Her favorite place in the world is a hammock that swings peacefully between two crabapple trees somewhere in New Mexico’s Gila National Forest.
How long does a hospice patient live?
Your hospice doctor and regular doctor certify you have a terminal illness with a life expectancy of six months or less. You accept care for comfort purposes instead of a cure for your illness. You sign a statement saying you choose hospice care instead of other Medicare-covered treatments for your illness.
Does Medicare cover dialysis?
If you receive dialysis while you’re an inpatient at a Medicare-approved hospital, Part A will cover it. If you receive dialysis as an outpatient—or certain kinds of training and support for self-dialysis—you’ll need to enroll in Medicare Part B to get coverage.
Is eligibility.com a Medicare provider?
Eligibility.com is a DBA of Clear Link Technologies, LLC and is not affiliated with any Medicare System Providers.
What does Part A pay for?
What Part A pays for hospital care. You’ll have to meet your deductible and pay any coinsurance or copayments before coverage kicks in. Once it does, Part A covers 100% of approved hospital services. 1.
How many visits does Medicare cover?
Medicare will cover one visit per year with a primary care doctor in a primary care setting (like a doctor’s office) to help lower your risk for cardiovascular disease. During this visit, the doctor may discuss aspirin use (if appropriate), check your blood pressure, and give you tips to make sure you eat well.
What are the benefits of Medicare?
Medicare covers comprehensive programs that include exercise, education, and counseling for patients who meet at least one of these conditions: 1 A heart attack in the last 12 months 2 Coronary artery bypass surgery 3 Current stable angina pectoris (chest pain) 4 A heart valve repair or replacement 5 A coronary angioplasty (a medical procedure used to open a blocked artery) or coronary stenting (a procedure used to keep an artery open) 6 A heart or heart-lung transplant Medicare also covers intensive cardiac rehabilitation programs that are typically more rigorous or more intense than regular cardiac rehabilitation programs. Services are covered in a doctor’s office or hospital outpatient setting. You pay 20% of the Medicare-approved amount if you get the services in a doctor’s office. In a hospital outpatient setting, you also pay the hospital a copayment. The Part B deductible applies.
What is Medicare Part B?
Medicare Part B covers medically necessary services and preventative services. The partial-list of Medicare covered services below will help you learn about some of the services covered by Medicare and basic information about each. You can find out if your test, item, or service is covered by visiting Medicare.gov here.
How much does Medicare pay for ambulatory surgery?
Except for certain preventive services (for which you pay nothing if the doctor or other health care provider accepts assignment), you pay 20% of the Medicare-approved amount to both the ambulatory surgical center and the doctor who treats you, and the Part B deductible applies.
What is clinical research?
Clinical research studies test how well different types of medical care work and if they’re safe. Medicare covers some costs, like office visits and tests, in qualifying clinical research studies.
How many depression screenings does Medicare cover?
Medicare covers one depression screening per year . The screening must be done in a primary care setting (like a doctor’s office) that can provide follow-up treatment and referrals. You pay nothing for this screening if the doctor or other qualified health care provider accepts assignment.
Does Medicare cover diabetes screenings?
Diabetes screenings. Medicare covers these screenings if your doctor determines you’re at risk for diabetes . You may be eligible for up to 2 diabetes screenings each year. You pay nothing for the test if your doctor or other qualified health care provider accepts assignment.
What is a medical social service?
Medical social services. Part-time or intermittent home health aide services (personal hands-on care) Injectible osteoporosis drugs for women. Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
What is intermittent skilled nursing?
Intermittent skilled nursing care (other than drawing blood) Physical therapy, speech-language pathology, or continued occupational therapy services. These services are covered only when the services are specific, safe and an effective treatment for your condition.
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
Do you have to be homebound to get home health insurance?
You must be homebound, and a doctor must certify that you're homebound. You're not eligible for the home health benefit if you need more than part-time or "intermittent" skilled nursing care. You may leave home for medical treatment or short, infrequent absences for non-medical reasons, like attending religious services.
What are non-covered services?
Medical and hospital services are sometimes required to treat a condition that arises as a result of services that are not covered because they are determined to be not reasonable and necessary or because they are excluded from coverage for other reasons. Services "related to" non-covered services (e.g., cosmetic surgery, non-covered organ transplants, non-covered artificial organ implants, etc.), including services related to follow-up care and complications of non-covered services which require treatment during a hospital stay in which the non-covered service was performed, are not covered services under Medicare. Services "not related to" non-covered services are covered under Medicare.
What is an admission order for Medicare Part A?
At the time that each Medicare Part A fee-for-service patient is admitted to an IRF, a physician must generate admission orders for the patient's care. These admission orders must be retained in the patient’s medical record at the IRF.
What is IRF benefit?
The IRF benefit is not to be used as an alternative to completion of the full course of treatment in the referring hospital. A patient who has not yet completed the full course of treatment in the referring hospital is expected to remain in the referring hospital, with appropriate rehabilitative treatment provided, until such time as the patient has completed the full course of treatment. Though medical management can be performed in an IRF, patients must be able to fully participate in and benefit from the intensive rehabilitation therapy program provided in IRFs in order to be transferred to an IRF. IRF admissions for patients who are still completing their course of treatment in the referring hospital and who therefore are not able to participate in and benefit from the intensive rehabilitation therapy services provided in IRFs will not be considered reasonable and necessary. Conversely, the IRF benefit is not appropriate for patients who have completed their full course of treatment in the referring hospital, but do not require intensive rehabilitation. Medicare benefits are available for such patients in a less-intensive setting.
Is there a reduction to payment or an adjustment to the end of year settlement?
Additionally, under DRGs, there no longer is a reduction to payment or an adjustment to the end of year settlement.
Does Medicare require IRF forms?
Medicare now requires that the IRF patient assessment instrument (IRF-PAI) forms be included in the patient’s medical record at the IRF (either in electronic or paper format). The information in the IRF-PAIs must correspond with all of the information provided in the patient’s IRF medical record.
What happens if a beneficiary does not qualify for Medicare?
When a beneficiary has an effective election on file with CMS but does not have a condition that would qualify for Medicare Part A inpatient hospital or posthospital extended care services if the beneficiary were an inpatient of a hospital or a resident of a SNF that is not an RNHCI, then services furnished in an RNHCI are not covered by Medicare. A Medicare claim for services that were furnished to that beneficiary would be treated as a claim for noncovered services. If the beneficiary only needs assistance with activities of daily living, then the beneficiary's condition could not be considered as meeting the Medicare Part A requirements. Prior to submitting a claim to Medicare it is the responsibility of the RNHCI’s utilization review committee to determine that the beneficiary meets the Medicare Part A requirements.
Is a broken leg covered by Medicare?
A beneficiary was hospitalized for a non-covered service and broke a leg while in the hospital. Services related to care of the broken leg during this stay is a clear example of "not related to" services and are covered under Medicare.
Can you transfer financial liability to a patient?
To transfer potential financial liability to the patient, you must give written notice to a Fee-for-Service Medicare patient before furnishing items or services Medicare usually covers but you don’ t expect them to pay in a specific instance for certain reasons, such as no medical necessity .
Does Medicare cover non-physician services?
Medicare normally excludes coverage for non-physician services to Part A or Part B hospital inpatients unless those services are provided either directly by the hospital/SNF or under an arrangement that the hospital/SNF makes with an outside source.
Does Medicare cover personal comfort items?
Medicare doesn’t cover personal comfort items because these items don’t meaningfully contribute to treating a patient’s illness or injury or the functioning of a malformed body member. Some examples of personal comfort items include:
Does Medicare cover dental care?
Medicare doesn’t cover items and services for the care, treatment, filling, removal, or replacement of teeth or the structures directly supporting the teeth, such as preparing the mouth for dentures, or removing diseased teeth in an infected jaw. The structures directly supporting the teeth are the periodontium, including:
Does Medicare cover exceptions?
This booklet outlines the 4 categories of items and services Medicare doesn’t cover and exceptions (items and services Medicare may cover). This material isn’t an all-inclusive list of items and services Medicare may or may not cover.
What are the factors that determine Medicare coverage?
Medicare coverage is based on 3 main factors 1 Federal and state laws. 2 National coverage decisions made by Medicare about whether something is covered. 3 Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is Part B?
Part B covers 2 types of services. Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
