Medicare Part A covers these services:
- Inpatient care in a hospital
- Skilled nursing facility care
- Inpatient care in a skilled nursing facility (not custodial or long-term care)
- Hospice care
- Home health care
- Inpatient care in a hospital.
- Skilled nursing facility care.
- Nursing home care (inpatient care in a skilled nursing facility that's not custodial or long-term care)
- Hospice care.
- Home health care.
What does Medicare Part a cover exactly?
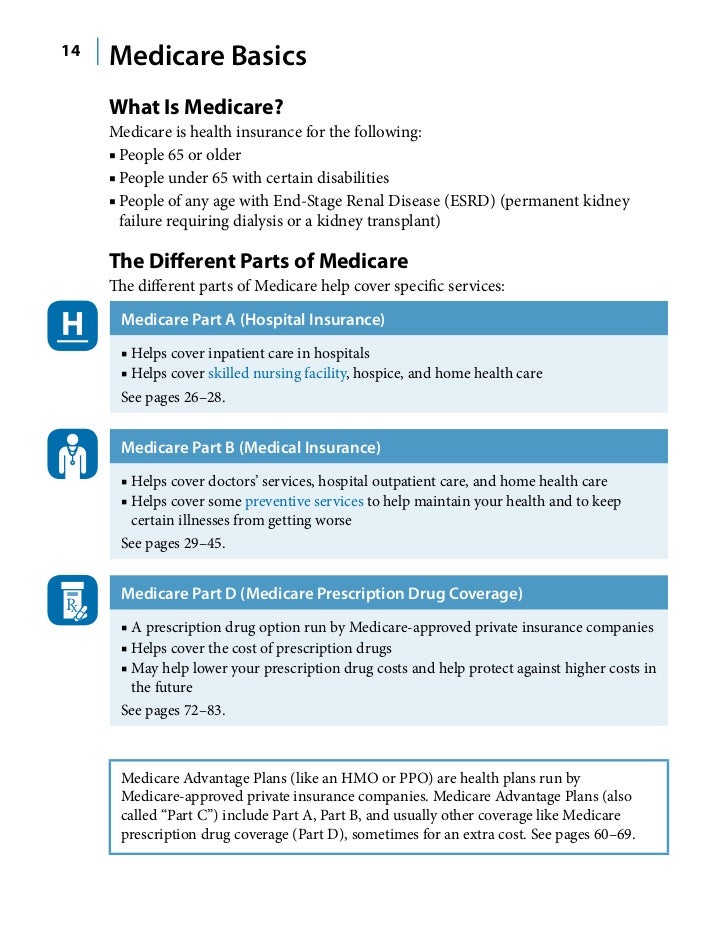
- Medicare Part A provides basic hospitalization coverage.
- Medicare part B covers outpatient care like doctor’s visits and diagnostic tests.
- Medicare Part C (Medicare Advantage) is a private option that combines Part A and Part B coverage and offers additional benefits.
- Medicare Part D is prescription drug coverage.
What is the difference between Medicare Part an and Part B?
Summary:
- Both Medicare Part A and B are federally funded plans that come with different coverages.
- Part A is free, and the patients need not pay a premium for the coverage. People have to pay some premium for availing themselves of the Part B coverage.
- Part A can be called hospital insurance whereas Part B can be termed as medical insurance.
What is Medicare Part A coverage?
When you have an Advantage plan, Medicare Parts A and Part B do not act as secondary coverage for your Advantage plan. You don't get healthcare services from both, because when you choose a Medicare Advantage plan you are deselecting CMS as the administrator of your healthcare needs.
What does Medicare Part a pay?
What does Medicare Part A pay for? May 8, 2021 / 1 min read / Written by Jason B. Print Article As Medicare Part A, or hospital insurance, primarily covers hospital stays. You will receive benefit coverage when you or a loved one is checked into a hospital, or other inpatient facility, for care.

What services are included in Medicare Part A?
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
What services are not covered under Medicare Part A?
What's not covered by Part A & Part B?Long-Term Care. ... Most dental care.Eye exams related to prescribing glasses.Dentures.Cosmetic surgery.Acupuncture.Hearing aids and exams for fitting them.Routine foot care.
What does Medicare Part A and B consist of?
Part A (Hospital Insurance): Helps cover inpatient care in hospitals, skilled nursing facility care, hospice care, and home health care. Part B (Medical Insurance): Helps cover: Services from doctors and other health care providers.
What is the difference between Medicare Part A and B?
If you're wondering what Medicare Part A covers and what Part B covers: Medicare Part A generally helps pay your costs as a hospital inpatient. Medicare Part B may help pay for doctor visits, preventive services, lab tests, medical equipment and supplies, and more.
What is included in Part A?
In general, Part A covers:Inpatient care in a hospital.Skilled nursing facility care.Nursing home care (inpatient care in a skilled nursing facility that's not custodial or long-term care)Hospice care.Home health care.
Does Medicare Part A cover 100%?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
What is covered by Medicare Part C?
Medicare Part C outpatient coveragedoctor's appointments, including specialists.emergency ambulance transportation.durable medical equipment like wheelchairs and home oxygen equipment.emergency room care.laboratory testing, such as blood tests and urinalysis.occupational, physical, and speech therapy.More items...
What is Medicare Part C called?
A Medicare Advantage is another way to get your Medicare Part A and Part B coverage. Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are offered by Medicare-approved private companies that must follow rules set by Medicare.
How do you get Medicare Part C?
To be eligible for a Medicare Part C (Medicare Advantage) plan:You must be enrolled in original Medicare (Medicare parts A and B).You must live in the service area of a Medicare Advantage insurance provider that's offering the coverage/price you want and that's accepting new users during your enrollment period.
Why do I need Medicare Part C?
Medicare Part C provides more coverage for everyday healthcare including prescription drug coverage with some plans when combined with Part D. A Medicare Advantage prescription drug (MAPD) plan is when a Part C and Part D plan are combined. Medicare Part D only covers prescription drugs.
Does Medicare Part A cover emergency room visits?
Does Medicare Part A Cover Emergency Room Visits? Medicare Part A is sometimes called “hospital insurance,” but it only covers the costs of an emergency room (ER) visit if you're admitted to the hospital to treat the illness or injury that brought you to the ER.
Is Medicare Part A free at age 65?
You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and paid Medicare taxes for at least 10 years. You can get Part A at age 65 without having to pay premiums if: You are receiving retirement benefits from Social Security or the Railroad Retirement Board.
What is Medicare Part A?
December 10, 2019. Medicare Part A is part of Original (traditional) Medicare and constitutes the federal government’s “hospital insurance.”. In short, Part A covers costs for inpatient services in the following situations: While that sounds pretty straightforward, this part of the Medicare program causes plenty of confusion.
What is the home health advance notice?
Alternatively, the agency should give you a notice called the “ Home Health Advance Beneficiary Notice of Noncoverage ” before providing noncovered services or supplies.
What does Part A pay for?
What Part A pays for hospital care. You’ll have to meet your deductible and pay any coinsurance or copayments before coverage kicks in. Once it does, Part A covers 100% of approved hospital services. 1.
How long does a hospice patient live?
Your hospice doctor and regular doctor certify you have a terminal illness with a life expectancy of six months or less. You accept care for comfort purposes instead of a cure for your illness. You sign a statement saying you choose hospice care instead of other Medicare-covered treatments for your illness.
How long do you have to stay in the hospital for skilled nursing?
For Part A to cover your skilled nursing costs, you must spend a minimum of three days as an inpatient (not under “observation”) in the hospital first. While you’re there, your doctor must determine that you require follow-up care that you cannot receive at home.
How many midnights are covered by Medicare?
Part A covers much of your care if you’re admitted to a hospital for at least "two midnights." In other words, you're covered if your hospital stay runs for at least two nights in a row.
What is the number to call for a Licensed Agent?
Call a Licensed Agent: 833-271-5571. In short, if you’re in the hospital for things like injuries, hip replacements, or heart attacks and strokes, you’ll be covered under Part A’s hospital care rules.
How often does Medicare cover pelvic exam?
Part B covers pap tests and pelvic exams to check for cervical and vaginal cancers. As part of the pelvic exam, Medicare also covers a clinical breast exam to check for breast cancer. Medicare covers these screening tests once every 24 months. Medicare covers these screening tests once every 12 months if you’re at high risk for cervical or vaginal cancer, or if you’re of child-bearing age and had an abnormal pap test in the past 36 months.
How often does Medicare cover mammograms?
Medicare covers screening mammograms to check for breast cancer once every 12 months for all women with Medicare who are 40 and older. Medicare covers one baseline mammogram for women between 35–39. You pay nothing for the test if the doctor or other qualified health care provider accepts assignment.
What does Medicare cover?
Medicare covers many tests, items and services like lab tests, surgeries, and doctor visits – as well as supplies, like wheelchair s and walkers. In general, Part A covers things like hospital care, skilled nursing facility care, hospice, and home health services. Medicare Part B covers medically necessary services and preventative services.
How many depression screenings does Medicare cover?
Medicare covers one depression screening per year . The screening must be done in a primary care setting (like a doctor’s office) that can provide follow-up treatment and referrals. You pay nothing for this screening if the doctor or other qualified health care provider accepts assignment.
How much does Medicare pay for chemotherapy?
For chemotherapy given in a doctor’s office or freestanding clinic, you pay 20% of the Medicare-approved amount, and the Part B deductible applies. For chemotherapy in a hospital inpatient setting covered under Part A, see hospital care (inpatient care).
How much does Medicare pay for ambulatory surgery?
Except for certain preventive services (for which you pay nothing if the doctor or other health care provider accepts assignment), you pay 20% of the Medicare-approved amount to both the ambulatory surgical center and the doctor who treats you, and the Part B deductible applies.
How many visits does Medicare cover?
Medicare will cover one visit per year with a primary care doctor in a primary care setting (like a doctor’s office) to help lower your risk for cardiovascular disease. During this visit, the doctor may discuss aspirin use (if appropriate), check your blood pressure, and give you tips to make sure you eat well.
How many days of home health care is covered by Medicare?
You are covered for up to 100 days of daily care or an unlimited amount of intermittent care. To qualify for Part A coverage, you must have spent at least three consecutive days as a hospital inpatient within 14 days of receiving home health care.
How long does Medicare cover inpatient care?
You are covered for up to 90 days each benefit period in a general hospital, plus 60 lifetime reserve days. Medicare also covers up to 190 lifetime days in a Medicare-certified ...
How long do you have to be in hospital to qualify for SNF?
To qualify, you must have spent at least three consecutive days as a hospital inpatient within 30 days of admission to the SNF, and need skilled nursing or therapy services. Home health care: Medicare covers services in your home if you are homebound and need skilled care.
Does Medicare pay for the cost of care?
Keep in mind that Medicare does not usually pay the full cost of your care, and you will likely be responsible for some portion of the cost-sharing (deductibles, coinsurances, copayments) for Medicare-covered services.
What is a medical social service?
Medical social services. Part-time or intermittent home health aide services (personal hands-on care) Injectible osteoporosis drugs for women. Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
What is intermittent skilled nursing?
Intermittent skilled nursing care (other than drawing blood) Physical therapy, speech-language pathology, or continued occupational therapy services. These services are covered only when the services are specific, safe and an effective treatment for your condition.
What is an ABN for home health?
The home health agency should give you a notice called the Advance Beneficiary Notice" (ABN) before giving you services and supplies that Medicare doesn't cover. Note. If you get services from a home health agency in Florida, Illinois, Massachusetts, Michigan, or Texas, you may be affected by a Medicare demonstration program. ...
What is the eligibility for a maintenance therapist?
To be eligible, either: 1) your condition must be expected to improve in a reasonable and generally predictable period of time, or 2) you need a skilled therapist to safely and effectively make a maintenance program for your condition , or 3) you need a skilled therapist to safely and effectively do maintenance therapy for your condition. ...
Can you get home health care if you attend daycare?
You can still get home health care if you attend adult day care. Home health services may also include medical supplies for use at home, durable medical equipment, or injectable osteoporosis drugs.
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
Do you have to be homebound to get home health insurance?
You must be homebound, and a doctor must certify that you're homebound. You're not eligible for the home health benefit if you need more than part-time or "intermittent" skilled nursing care. You may leave home for medical treatment or short, infrequent absences for non-medical reasons, like attending religious services.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is private nursing care?
Private nursing care. A television or telephone in your room, and personal items like razors or slipper socks, unless the hospital or skilled nursing facility provides these to all patients at no additional charge.
What services are paid for under Part B?
The following services are paid for under Part B instead of Part A: All physicians’ services — including those provided by doctors, surgeons and anesthetists in the hospital or a skilled nursing facility, or as part of the home health care or hospice benefits.
What is not covered by Part A?
Part A does not cover the following: A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care.
Can you get Medicare for a stay in a nursing home?
If you have been in the hospital “under observation” — even for longer than three days — you do not qualify for Medicare coverage of a stay in a skilled nursing facility. The costs of staying as a long-term resident in a nursing home or assisted living facility.