California: Then-Gov. Jerry Brown (D) on June 27, 2013, signed legislation that expanded the state's Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Full Answer
Which states have adopted the Medicaid expansion?
· Where States Stand on Medicaid Expansion. Updated Jan. 5, 2022. The map tracks implementation of the Affordable Care Act’s Medicaid expansion in all states. The map indicates whether states are using alternative approaches through demonstration waivers, and also features information about state legislation or citizen referendums, governors ...
What is the ACA Medicaid expansion?
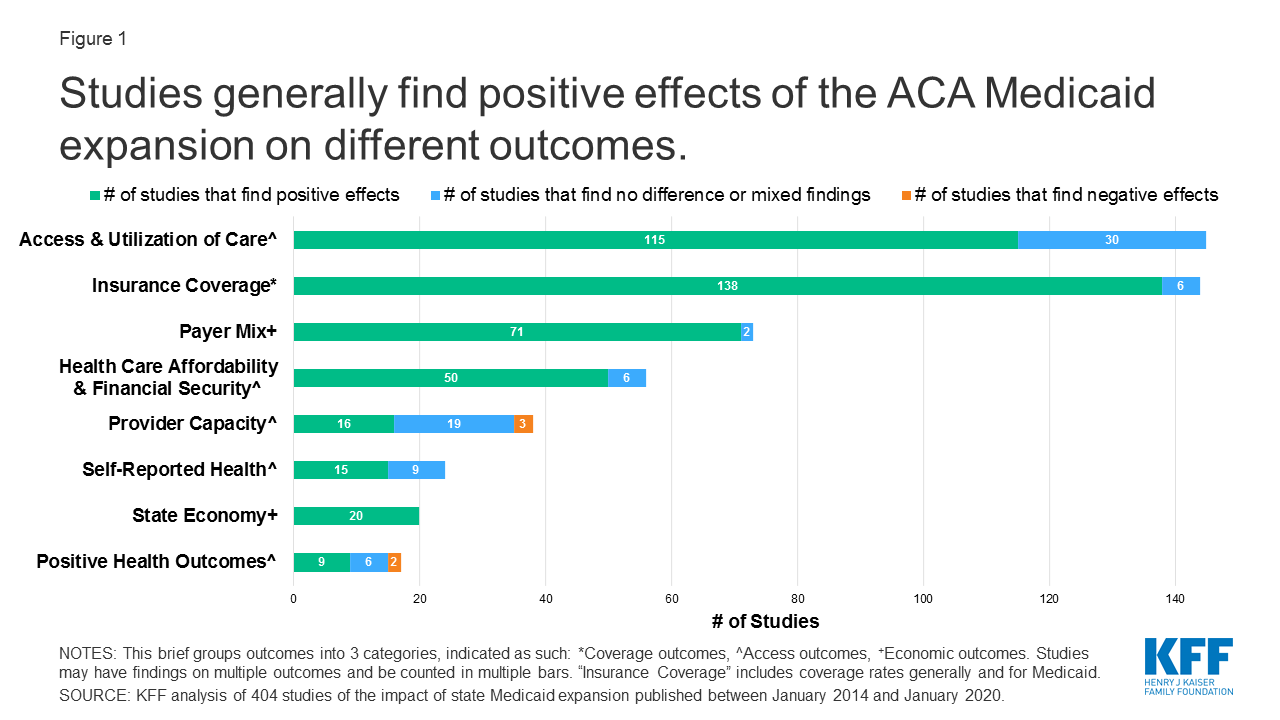
· have implemented the expansion: Michigan (April 1, 2014), New Hampshire (July 1, 2014), Pennsylvania (January 1, 2015), Indiana (February 1, 2015), Alaska (September 1, 2016), Virginia (January 1, 2019), Maine (January 10, 2019), Idaho (January 1, 2020), Utah (January 1, 2020), and Nebraska (October 1, 2020). (See Figure 1.)
What are States doing about health insurance expansion?
· Affordable Care Act Medicaid Expansion. Medicaid—a federal/state partnership with shared authority and financing—is a health insurance program for low-income individuals, …
Do all 50 states participate in the Medicaid program?
· There is no deadline for states to opt to expand Medicaid under the ACA, and debate continues in some states about whether to expand. In 2020, two states (Missouri and …

Which states have implemented the Medicaid expansion under the Affordable Care Act?
New Hampshire, Michigan, Indiana, Pennsylvania, Alaska, Montana, and Louisiana all expanded their Medicaid programs between 2014 and 2016. Expansion took effect in Virginia and Maine in 2019, in Utah, Idaho, and Nebraska in 2020, and in Oklahoma and Missouri in 2021.
Did the ACA require states to expand Medicaid?
If your state hasn't expanded Medicaid, your income is below the federal poverty level, and you don't qualify for Medicaid under your state's current rules, you won't qualify for either health insurance savings program: Medicaid coverage or savings on a private health plan bought through the Marketplace.
How many states opted out of the Affordable Care Act?
Twenty-four states have opted out of expanding Medicaid coverage under the Affordable Care Act.
Did the ACA expand Medicare?
Obamacare's expanded Medicare preventive coverage applies to all Medicare beneficiaries, whether they have Original Medicare or a Medicare Advantage plan.
Why did Florida not expand Medicaid?
However, the U.S. Supreme Court ruled in 2012 that the withholding of funds for existing Medicaid programs was unconstitutional. Medicaid expansion was left as an option for states, and Florida did not implement it. As of August 2020, Florida is one of 12 states that have not expanded Medicaid.
How many states have not expanded Medicaid?
12 statesIncreases are from pre-ARPA policy and are presented for 12 states that have not expanded Medicaid: Alabama, Florida, Georgia, Kansas, Mississippi, North Carolina, South Carolina, South Dakota, Tennessee, Texas, Wisconsin, and Wyoming. Data: Urban Institute's Health Insurance Policy Simulation Model (HIPSM), 2021.
Which is a reason some states have not expanded Medicaid to cover more of their needy residents following passage of the ACA?
(The cap on Medicaid eligibility under the ACA is 138 percent of the poverty level, which is currently less than $28,000/year for a family of three.) The lack of a work requirement is purportedly one of the reasons some states still haven't expanded Medicaid coverage.
What are the cons of the Affordable Care Act?
Cons:The cost has not decreased for everyone. Those who do not qualify for subsidies may find marketplace health insurance plans unaffordable. ... Loss of company-sponsored health plans. ... Tax penalties. ... Shrinking networks. ... Shopping for coverage can be complicated.
Is Obamacare in every state?
Is the ACA available in all states? Prior to the ACA being enacted, the CDC estimated that 48 million Americans were without health insurance. But now the ACA guarantees basic health coverage, making quality health coverage available no matter what state you reside in.
What did the Affordable Care Act do for Medicare?
Medicare Premiums and Prescription Drug Costs The ACA closed the Medicare Part D coverage gap, or “doughnut hole,” helping to reduce prescription drug spending. It also increased Part B and D premiums for higher-income beneficiaries. The Bipartisan Budget Act (BBA) of 2018 modified both of these policies.
What happens to the ACA subsidy when one person goes on Medicare?
Individual market plans no longer terminate automatically when you turn 65. You can keep your individual market plan, but premium subsidies will terminate when you become eligible for premium-free Medicare Part A (there is some flexibility here, and the date the subsidy terminates will depend on when you enroll).
How did the ACA expand coverage?
The Affordable Care Act's (ACA) Medicaid expansion expanded Medicaid coverage to nearly all adults with incomes up to 138% of the Federal Poverty Level ($17,774 for an individual in 2021) and provided states with an enhanced federal matching rate (FMAP) for their expansion populations.
What is the Affordable Care Act?
Medicaid—a federal/state partnership with shared authority and financing—is a health insurance program for low-income individuals, children, their parents, the elderly and people with disabilities. Medicaid pays for health care for more than 74.5 million people nationally.
Do all states have to meet the federal minimum requirements for Medicaid?
However, eligibility for Medicaid benefits varies widely among the states - all states must meet federal minimum requirements, but they have options for expanding Medicaid beyond the minimum federal guidelines, the details are outlined here.
Is Medicaid expansion a waiver?
A number of states implemented Medicaid expansion through an approved Section 1115 Waiver. For more information on Medicaid waivers click here.
How many people are eligible for Medicaid in non-expansion states?
If all states expanded Medicaid, those in the coverage gap and those who are instead eligible for Marketplace coverage would bring the number of nonelderly uninsured adults eligible for Medicaid to more than 4.3 million people in the twelve current non-expansion states. The potential number of people who could be reached by Medicaid expansion varies by state (Table 1).
How much will the ACA cost in 2021?
It also is unlikely that people who fall into the coverage gap will be able to afford ACA coverage, as they are not eligible for premium subsidies: in 2021, the national average unsubsidized premium for a 40-year-old non-smoking individual purchasing coverage through the Marketplace was $436 per month for the lowest-cost silver plan and $328 per month for a bronze plan, which equates to nearly eighty percent of income for those at the lower income range of people in the gap (below 41% FPL) and nearly a third of income for those at the higher income range of people in the gap.
Is Medicaid expansion limited in 2021?
However, in the 12 states that have not adopted the Medicaid expansion as of January 2021, Medicaid eligibility for adults remains limited. At a time when many are losing income and potentially health coverage during a health crisis, these eligibility gaps leave many without an affordable coverage option and could contribute to growth in ...
Will the ACA expand Medicaid?
There is no deadline for states to opt to expand Medicaid under the ACA, and debate continues in some states about whether to expand. In 2020, two states (Missouri and Oklahoma) adopted the Medicaid expansion via ballot initiatives, and both states plan to implement expansion in mid-2021 (these states are considered Medicaid expansion states in this analysis). In addition, there will be new federal focus on encouraging expansion, either through legislative or Administrative actions. Biden has proposed creating a Medicare-like public option plan, which would be available to anyone and automatically cover people with low incomes in states that have not expanded Medicaid. Other possible legislative actions include reinstating the 100% matching for states that newly adopt the expansion for a period of time (the current match rate for the expansion is 90%). The Biden Administration could also can revise current demonstration waiver policy or promote new waivers to focus on expanding coverage. Whether, and to what extent, these actions are implemented and extend Medicaid to people currently in the coverage gap will be a key policy issue for the upcoming year.
What is the uninsured rate in 2019?
In 2019 the uninsured rate in non-expansion states was nearly double that of expansion states (15.5% vs. 8.3%). By definition, people in the coverage gap have limited family income and live below the poverty level.
Why do people fall into the Medicaid coverage gap?
At a time when many need health care services due to the health care crisis or face loss of financial security due to the economic downturn, millions fall into the Medicaid coverage gap due to their state’s decision not to expand eligibility.
What would happen if Medicaid didn't expand?
If states that are currently not expanding their programs adopt the Medicaid expansion, all of the nearly 2.2 million adults in the coverage gap would gain Medicaid eligibility. In addition, 1.8 million uninsured adults with incomes between 100 and 138% of poverty 6 (most of whom are currently eligible for Marketplace coverage) would also gain Medicaid eligibility (Figure 3 and Table 1). Though most of these adults are eligible for substantial tax credits to purchase Marketplace coverage, 7 Medicaid coverage would likely provide more comprehensive benefits and lower premiums or cost-sharing than they would face under Marketplace coverage. For example, research from early implementation of the ACA showed that coverage of behavioral health services, prescription drugs, rehabilitative and habilitative services, and long-term services and supports may be more limited in the Marketplace compared to Medicaid. 8,9 In addition, research examining the population with incomes between 100-138% FPL in expansion and non-expansion states finds that Medicaid expansion coverage produced far greater reductions than subsidized Marketplace coverage in average total out-of-pocket spending, average out-of-pocket premium spending, and average cost-sharing spending.
Which state has the largest Medicaid gap?
As a result, Texas has the biggest coverage gap in the country, with an estimated 761,000 residents ineligible for Medicaid and also ineligible for premium subsidies to offset the cost of private coverage in the exchange. Studies and reports studies show lagging health outcomes and a nationally high uninsured rate at least partly due to ...
Why is Texas refusing to expand Medicaid?
By refusing Medicaid expansion under the ACA, Texas has already missed out on billions in federal funding that would otherwise have flowed to the state to provide medical care for their low-income residents. And in addition, the state’s emergency rooms are providing $5.5 billion in uncompensated care each year, treating patients who don’t have health insurance. If Medicaid eligibility had been expanded, uncompensated care would have dropped considerably, so hospitals and business groups across the state have been pressuring lawmakers to relent on their opposition to Medicaid expansion.
What percentage of poverty is Medicaid?
As the ACA was written, it called for Medicaid expansion in every state for legally present residents with incomes up to 133 percent of poverty (138 percent, with the built-in 5 percent income disregard).
Is Medicaid expansion in Texas?
The Texas Institute of Health Care Quality and Efficiency board has recommended Medicaid expansion as a solution to what they called an “unacceptable” number of people without health insurance in Texas. State lawmakers only meet in odd-numbered years in Texas.
Who sponsored HB3791?
Texas Medicaid history. During the 2013 legislative session, Republican John Zerwas sponsored HB3791, which would have directed the state to craft a “ Texas solution ” to Medicaid expansion. But it did not pass.
Did Texas miss Medicaid expansion?
Missing out on billions in federal funding. By refusing Medicaid expansion under the ACA, Texas has already missed out on billions in federal funding that would otherwise have flowed to the state to provide medical care for their low-income residents.
Do Texas residents qualify for medicaid?
They don’t qualify for Medicaid, but their incomes are under the poverty level which means they are not eligible for subsidies in the exchange. Prior to 2014, Texas had the highest uninsured rate in the country, and that is still the case.
How many states have not expanded Medicaid?
Today, twelve states have still not expanded Medicaid. The biggest are Texas, Florida, and Georgia, but there are a few outside the South, including Wyoming and Kansas. There are more than 2 million people across the United States who have no option when it comes to health insurance. They're in what's known as the "coverage gap" — they don't ...
How much does the federal government cover for Medicaid?
Essentially, the federal government will cover 90% of the costs of the newly eligible population, and an additional 5% of the costs of those already enrolled.
What are the political and logistical challenges of Medicaid?
The political and logistical challenges would be tough, policy analysts say. Logistically, such a plan would require counties and cities to create new infrastructure to run a Medicaid program, Rudowitz notes, and the federal government would have to oversee how well these new local programs complied with all of Medicaid's rules.
Who introduced the Cover Now Act?
The COVER Now Act, introduced by Rep. Lloyd Doggett, D-Texas, would empower local jurisdictions to expand Medicaid. So, if you live in Austin, Texas, maybe you could get Medicaid, even if someone in Lubbock still couldn't. The political and logistical challenges would be tough, policy analysts say.
Does Briana Wright have health insurance?
Briana Wright is one of those people. She's 27, lives near Jackson, Miss., works at McDonalds, and doesn't have health insurance.
