What are Tier 4 drugs?
Tier 4 These drugs are considered specialty drugs and are typically used to cover serious ...
What drugs are in Tier 1?
Tier 1 CO-PAY MEDICATION LIST 2021. Aspirin buffered tablet . Aspirin chewable tablet . Aspirin enteric coated tablet . Allopurinol tablet . Celecoxib capsule . Diclofenac tablet . Ibuprofen tablet . Meloxicam tablet . Naproxen tablet . Clopidogrel Bisulfate tablet . Warfarin Sodium tablet . Alendronate tablet . Atorvastatin tablet . Ezetimibe ...
What is a Tier 1 and Tier 2 drug?
Tier 1: The prescription drug tier which consists of the lowest cost tier of prescriptions drugs, most are generic. Tier 2: The prescription drug tier which consists of medium-cost prescription drugs, most are generic, and some brand-name prescription drugs. Tier 3
What is a Tier 4 prescription drug?
Tier 4 or Tier IV, also called specialty drugs: These are usually newly approved pharmaceutical drugs that your payer wants to discourage because of their expense. Tier IV is a newer designation, first used in 2009.

What are Tier 5 medications?
What does each drug tier mean?Drug TierWhat it meansTier 5Specialty. These are the most expensive drugs on the drug list. Specialty drugs are used to treat complex conditions like cancer and multiple sclerosis. They can be generic or brand name.5 more rows•Apr 27, 2020
What is a Tier 1 prescription?
There are typically three or four tiers: Tier 1: Least expensive drug options, often generic drugs. Tier 2: Higher price generic and lower-price brand-name drugs. Tier 3: Mainly higher price brand-name drugs. Tier 4: Highest cost prescription drugs.
What is a Tier 6 prescription?
The prescription drug tier which consists of some of the highest-cost prescription drugs, most are specialty drugs. Tier 6. The prescription drug tier which consists of the highest-cost prescription drugs, most are specialty drugs.
What does Tier 2 drug coverage mean?
4-tier plan: The levels are organized as follows: Level or Tier 1: Low-cost generic and brand-name drugs. Level or Tier 2: Higher-cost generic and brand-name drugs. Level or Tier 3: High-cost, mostly brand-name drugs that may have generic or brand-name alternatives in Levels 1 or 2.
What is the difference between Tier 1 and Tier 2 insurance?
Tier 1 usually includes a select network of providers that have agreed to provide services at a lower cost for you and your covered family members. Tier 2 provides you the option to choose a provider from the larger network of contracted PPO providers, but you may pay more out-of-pocket costs.
What tier drug is Metoprolol?
What drug tier is metoprolol typically on? Medicare prescription drug plans typically list metoprolol on Tier 1 of their formulary. Generally, the higher the tier, the more you have to pay for the medication. Most plans have 5 tiers.
What are the 4 standardized levels of Medicare prescription drug coverage?
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.
Who decides what tier a drug is?
Every plan creates its own formulary structure, decides which drugs it will cover and determines which tier a drug is on. One plan may cover a drug that another doesn't. The same drug may be on tier 2 in one plan's formulary and on tier 3 in a different plan's formulary. Formularies change.
What tier is amlodipine?
What drug tier is amlodipine typically on? Medicare prescription drug plans typically list amlodipine on Tier 1 of their formulary. Generally, the higher the tier, the more you have to pay for the medication. Most plans have 5 tiers.
How many tiers are there in Medicare Part D?
five-tierThe typical five-tier formulary design in Part D includes tiers for preferred generics, generics, preferred brands, non-preferred drugs, and specialty drugs.
What is the Doughnut hole for 2021?
For 2021, the coverage gap begins when the total amount your plan has paid for your drugs reaches $4,130 (up from $4,020 in 2020). At that point, you're in the doughnut hole, where you'll now receive a 75% discount on both brand-name and generic drugs.
What is a specialty tier drugs?
Specialty tier drugs—defined by Medicare as drugs that cost more than $670 per month in 2019—are a particular concern for Part D enrollees in this context.
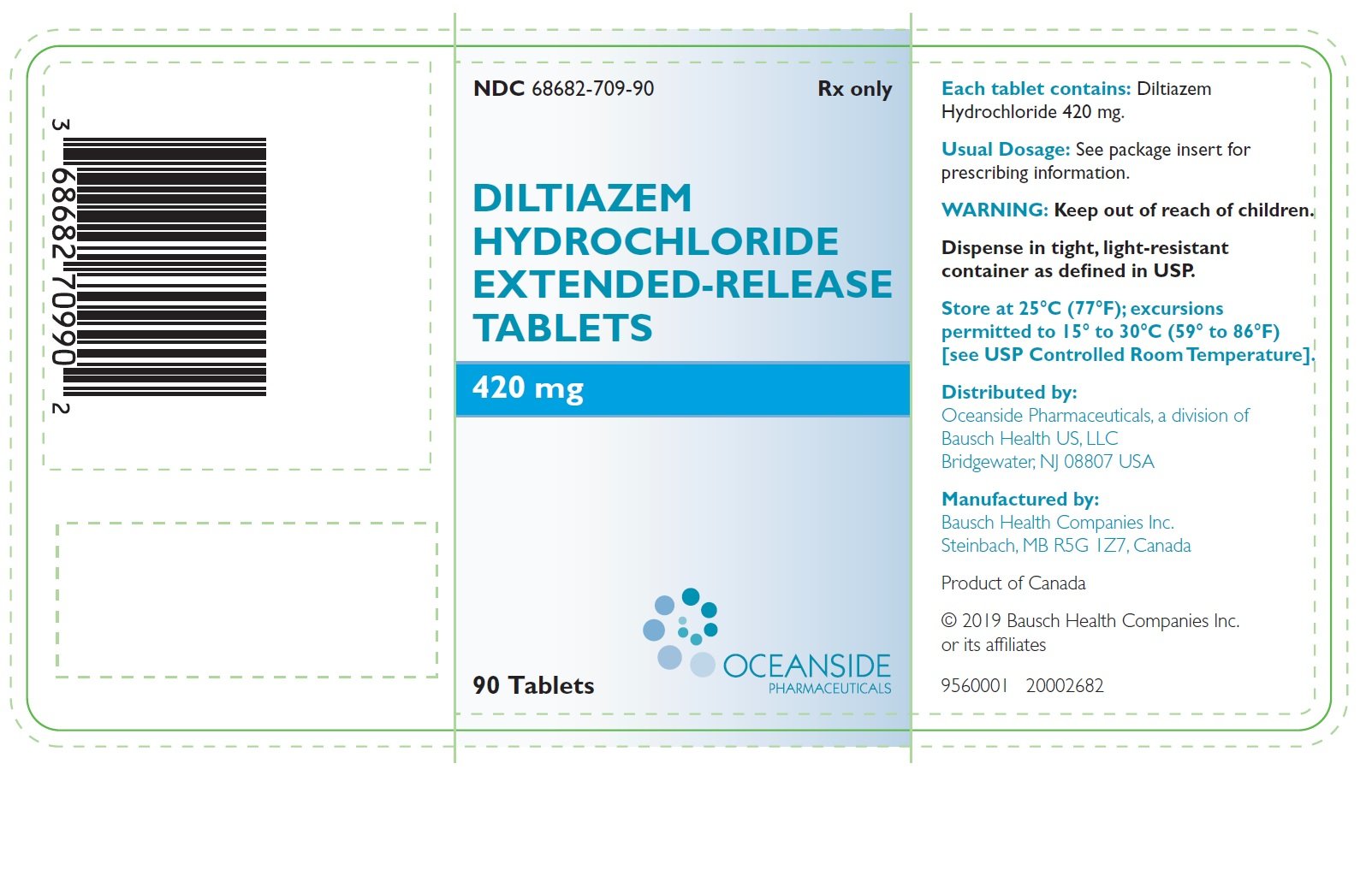
What tier is diltiazem ER?
Medicare prescription drug plans typically list diltiazem ER (Cardizem CD) on Tier 2 of their formulary. Generally, the higher the tier, the more you have to pay for the medication. Most plans have 5 tiers.
How much does Medicare cover for a donut hole?
FREE – $20. In the Donut Hole (also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for your drug. Therefore, you may pay more for your drug. Copay Range. $1. In the Post-Donut Hole (also called Catastrophic Coverage) stage, Medicare should cover most of the cost of your drug.
What are the tiers of Medicare?
Here's an example of a Medicare drug plan's tiers (your plan’s tiers may be different): Tier 1—lowest. copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug.
What is a tier in prescription drug coverage?
Tiers. To lower costs, many plans offering prescription drug coverage place drugs into different “. tiers. Groups of drugs that have a different cost for each group. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. ” on their formularies. Each plan can divide its tiers in different ways.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
What is a drug plan's list of covered drugs called?
A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary. Many plans place drugs into different levels, called “tiers,” on their formularies. Drugs in each tier have a different cost. For example, a drug in a lower tier will generally cost you less than a drug in a higher tier.
When will Medicare start paying for insulin?
Starting January 1, 2021, if you take insulin, you may be able to get Medicare drug coverage that offers savings on your insulin. You could pay no more than $35 for a 30-day supply. Find a plan that offers this savings on insulin in your state. You can join during Open Enrollment (October 15 – December 7, 2020).
What are the tiers of Medicare Part D?
The Medicare Part D tiers refer to how drugs are organized in a formulary. They include both generic and brand name drugs, covered for different prices. Most commonly there are tiers 1-5, with 1 covering the lowest-cost drugs and 5 covering the most expensive specialty medications.
What is Tier 1 Medicare?
Tier 1 is the least expensive of the Medicare Part D tiers, and includes the lower-cost preferred generic drugs. Preferred drugs means a certain set of types of medications that have been approved by the insurance company to be in this low-cost grouping. Generic refers to non-name brand versions of each type of drug.
What is Medicare Advantage Plan?
Some Medicare Advantage plans, known as Medicare Advantage Prescription Drug Plans (MAPD), include Part D coverage. In MAPD plans, the portion of the plan that covers drugs will follow the same standards as stand-alone prescription drug plans. So, you will want to check the plan’s formulary to see how your medications are covered.
What is tier 6 insurance?
Tier 6 tends to refer to a few generic drugs for diabetes and high cholesterol available with some specific insurance plans . Tier 6 is designed to offer an affordable option for some of the most commonly needed drugs, and tend to cover only those specific drugs.
Does Medicare Part D cost more than tier 1?
Medicare Part D tiers 1 and 2 are often set up to exempt you from paying a deductible, whereas with drugs in the higher tiers you may have to pay the full drug cost until you meet the deductible, then pay a copay/coinsurance.
What is a drug tier?
Drug tiers are how we divide prescription drugs into different levels of cost.
How much does a tier 1 drug cost?
Preferred generic. These are commonly prescribed generic drugs. For most plans, you’ll pay around $1 to $3 for drugs in this tier. Tier 2. Generic. These are also generic drugs, but they cost a little more than drugs in Tier 1. For most plans, you’ll pay around $7 to $11 for drugs in this tier.
What is tier 4 in Medicare?
Tier 4. Nonpreferred drug. These are higher-priced brand name and generic drugs not in a preferred tier. For most plans, you’ll pay around 45% to 50% of the drug cost in this tier. Tier 5. Specialty. These are the most expensive drugs on the drug list.
What is specialty drug?
Specialty drugs are used to treat complex conditions like cancer and multiple sclerosis. They can be generic or brand name. For most plans, you’ll pay 25% to 33% of the retail cost for drugs in this tier. Tier 6.
What Is a Drug Formulary?
A drug formulary is the list of prescription drugs covered by your plan. It includes both generic and brand name medications.
What Are Drug Tiers?
Medications from the drug formulary are placed on tiers. The lowest tier has the lowest prices, with costs rising along with the tiers.
How Are Drugs Priced on the Tiers?
Prescription drug pricing varies according to the insurer. However, generally speaking, you pay either a co-pay, which is a set dollar amount, or co-insurance, which is a percentage of the drug cost.
Other Prescription Drug Plan Restrictions
In addition to the formulary and tier pricing, your insurer may place other restrictions on coverage. The most common are step therapy and prior authorization.
Why Do PDPs Have These Restrictions?
The goal of drug formularies, tier pricing, and other restrictions is to help lower costs for both you and your insurance company.
What Happens When the Formulary Changes?
Insurance companies add and remove medications from the drug formulary throughout the year, not just during Annual Enrollment. That means that you may suddenly discover a medication you've taken for years is no longer covered.
Saving Money on Your Prescriptions
The easiest way to save money on your prescriptions is to follow your plan's rules. And understanding your PDP's drug formulary, tier pricing, and other restrictions is the first step toward working within those guidelines.
What is a drug tier?
Drug tiers are a way for insurance providers to determine medicine costs. The higher the tier, the higher the cost of the medicine for the member in general. If you look at your insurance card, you’ll see the copay values for all the tiers under your insurance plan.
What are the different tiers of medicine?
What do different drug tiers mean? Under your insurance plan, the prescription medicines available to you are split into tiers, which then determine your cost. Medicines are typically placed into 1 of 5 tiers—from Tier 1 (generics) to Tier 5 (highest-cost medicines)—depending on their strength, type or purpose.
What is a 4 tier plan?
4-tier plan: Covered prescription drugs are assigned to 1 of 4 different levels with corresponding copayment or coinsurance amounts. The levels are organized as follows: Level or Tier 1: Low-cost generic and brand-name drugs. Level or Tier 2: Higher-cost generic and brand-name drugs.
What is the copay value for tier 1?
Copay values could be as little as $0 for generic medicines in Tier 1, while the percentage you pay will rise as you move toward Tier 5. Specialty drugs are high-cost/high-technology drugs that often require special dispensing conditions and may be listed in the highest tier or not listed within any tier.
What is a level 2 drug?
Level or Tier 2: Nonpreferred and low-cost generic drugs. Level or Tier 3: Preferred brand-name and some higher-cost generic drugs. Level or Tier 4: Nonpreferred brand-name drugs and some nonpreferred, highest-cost generic drugs. Level or Tier 5: Highest-cost drugs including most specialty medications.
What are the levels of a drug plan?
Level or Tier 2: Brand-name drugs, including preferred and nonpreferred options. Level or Tier 3: Highest-cost drugs. 4-tier plan: