If you and your spouse (or other household members) are enrolled on the same Marketplace plan, but you’re the only one eligible for Medicare, you’ll cancel Marketplace coverage for just yourself. This way any others on the Marketplace application can keep Marketplace coverage. Find out how here.
Full Answer
What happens to my marketplace plan if my spouse gets Medicare?
Jun 04, 2018 · One of the most viable options for the majority of people is going to be to buy coverage through the marketplace, created by the Affordable Care Act, until the younger spouse turns 65. Insurance plans offered under the ACA are comprehensive and companies can’t refuse coverage based on pre-existing conditions.
How can I help my spouse qualify for Medicare?
Jul 31, 2015 · If you and your spouse (or other household members) are enrolled on the same Marketplace plan, but you’re the only one eligible for Medicare, you’ll cancel Marketplace coverage for just yourself. This way any others on the Marketplace application can keep Marketplace coverage.
Does Medicare cover my spouse's health insurance?
If someone gets Medicare but the rest of the people on the application want to keep their Marketplace coverage, you can end coverage for just some people on the Marketplace plan, like a spouse or dependents.
What happens when one spouse turns 65 and becomes eligible for Medicare?
As I understand it, the premium should stay the same when one spouse goes on Medicare, presuming the income stays the same, but you also have to then pay the Medicare premium. You come out behind because of that and also because the Medicare participant’s expenses won’t count toward the same out of pocket limit the rest of the family has on the Marketplace plan.

Why is it important to sign up for Medicare?
It’s important to sign up for Medicare when you’re first eligible because once your Medicare Part A coverage starts, you’ll have to pay full price for a Marketplace plan. This means you’ll no longer be eligible to use any premium tax credit or help with costs you might have been getting with your Marketplace plan.
What happens if you enroll in Medicare after the initial enrollment period?
Also, if you enroll in Medicare after your Initial Enrollment Period, you may have to pay a late enrollment penalty. It’s important to coordinate the date your Marketplace coverage ends with the effective date of your Medicare enrollment, to make sure you don’t have a break in coverage.
Can I switch from Marketplace to Medicare?
How to transition from the Marketplace to Medicare coverage. If you have a health plan through the Health Insurance Marketplace® and will soon have Medicare eligibility, it’s not too soon to start planning for your coverage to switch. If you have a Marketplace plan now, you can keep it until your Medicare coverage starts.
When does Medicare enrollment end?
For most people, the Initial Enrollment Period starts 3 months before their 65th birthday and ends 3 months after their 65th birthday.
When does Medicare pay late enrollment penalty?
If you enroll in Medicare after your Initial Enrollment Period ends, you may have to pay a Part B late enrollment penalty for as long as you have Medicare. In addition, you can enroll in Medicare Part B (and Part A if you have to pay a premium for it) only during the Medicare general enrollment period (from January 1 to March 31 each year).
Are there income limits for ACA subsidy eligibility?
Normally, subsidy eligibility only extends to households with income up to 400% of the poverty level, with no subsidies available for households with income above that point. But for 2021 and 2022, the American Rescue Plan has eliminated that income threshold.
Will we qualify for a subsidy?
The exchange will look to see what percentage of your total household income is necessary to cover the full-price cost of the benchmark plan for your wife. If it’s more than the percentage of income that people are expected to pay for their coverage, she’ll qualify for a premium subsidy.
What is the health insurance marketplace?
The Health Insurance Marketplace is designed for people who don’t have health coverage. If you have health coverage through Medicare, the Marketplace doesn't affect your Medicare choices or benefits. This means that no matter how you get Medicare, whether through.
When does Medicare Part A start?
For most people, the Initial Enrollment Period starts 3 months before their 65th birthday and ends 3 months after their 65th birthday month. Once your Medicare Part A coverage starts, you won’t be eligible for a premium tax credit or other savings for a Marketplace plan. If you kept your Marketplace plan, you’d have to pay full price.
When is open enrollment for Medicare?
During the Medicare Open Enrollment Period (October 15–December 7) , you can review your current Medicare health and prescription drug coverage to see if it still meets your needs. Take a look at any cost, coverage, and benefit changes that'll take effect next year.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
What is Medicare health plan?
Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan. Medicare health plans include all Medicare Advantage Plans, Medicare Cost Plans, and Demonstration/Pilot Programs.
What is a PACE plan?
Programs of All-inclusive Care for the Elderly (PACE) organizations are special types of Medicare health plans. PACE plans can be offered by public or private companies and provide Part D and other benefits in addition to Part A and Part B benefits. , you won’t have to make any changes to your current Medicare coverage.
Does Medicare count as a qualifying health insurance?
Medicare counts as qualifying health coverage and meets the law (called the individual Shared Responsibility Payment) that required people to have health coverage if they can afford it. If you had Medicare for all of 2018 (or for earlier plan years), check the box on your federal income tax form for that year.
How long can you keep Cobra insurance?
The COBRA law allows people who have left or lost a job to continue coverage through their former employer for up to 18 months by paying the full premiums. If eligible, spouses and dependent children can receive this coverage, even if departing employees don't take it themselves.
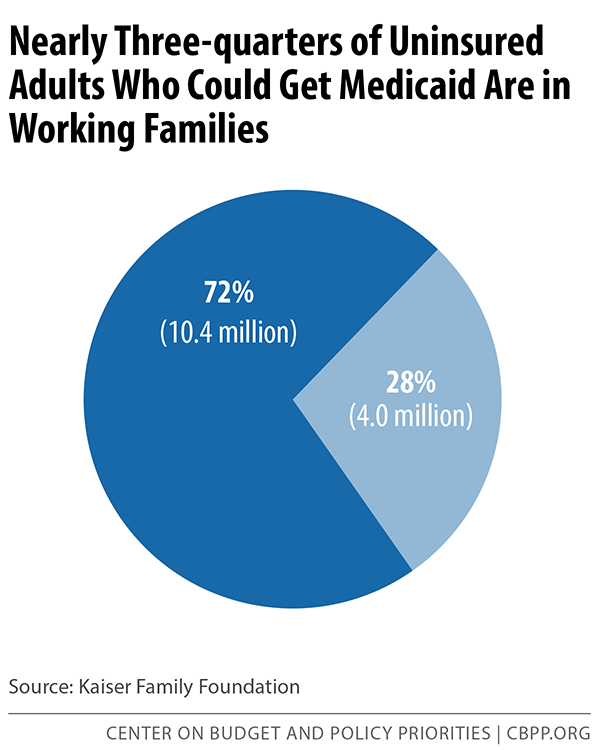
What is the ACA eligibility for Medicaid?
The ACA gives states the option to expand Medicaid eligibility to people with incomes of up to 138 percent of the federal poverty level ($17,236 in 2020).
What is individual insurance?
Individual insurance. This is insurance you buy on your own. Even though it's called "individual" — to distinguish it from "group" employer insurance — you can purchase a family policy that will cover you, your spouse and any dependent children. This type of insurance is often costly, especially for people older than 50.
How many people are on medicaid?
Jointly funded by the federal and state governments, Medicaid is the nation's public health insurance program for people with limited income and financial resources, serving nearly 65 million people as of late 2019.
When is open enrollment for ACA?
Open enrollment for ACA plans only runs from November 1 to December 15 in most states, but people who are losing their current health coverage may qualify for a special enrollment period. Depending on your income and the plan you choose, you may be eligible for subsidies (in the form of tax credits) to reduce your premiums.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What happens if a group health plan doesn't pay?
If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment. Medicare may pay based on what the group health plan paid, what the group health plan allowed, and what the doctor or health care provider charged on the claim.
What is a copayment?
A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug. or a. deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.
