Fill out a "Redetermination Request Form [PDF, 100 KB]" and send it to the Medicare contractor at the address listed on the MSN. Follow the instructions for sending an appeal. You must send your request for redetermination to the company that handles claims for Medicare (their address is listed in the "Appeals Information" section of the MSN).
How do I request a Medicare redetermination?
Send a written request to the company that handles claims for Medicare (their address is listed in the "Appeals Information" section of the MSN.) Your request must include: Your name and Medicare Number. The specific item (s) and/or service (s) for which you're requesting a redetermination and the specific date (s) of service.
What should be included in a redetermination request?
An explanation of why the appellant disagrees with the contractor's determination The appellant should include with their redetermination request any and all documentation that supports their argument against the previous decision. A minimum monetary threshold on the claim is not required to request a redetermination.
What is a Medicare request for payment?
• A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, or drug you already got. • A request to change the amount you must pay for a health care service, supply, item, or drug.
Can I submit additional information or evidence after the filing redetermination?
You can submit additional information or evidence after the filing redetermination request, but, it may take longer than 60 days for the Medicare Administrator Contractor (MAC) that processes claims for Medicare to make a decision.
What is the Medicare redetermination process?
Any party to the initial claim determination that is dissatisfied with the decision may request a redetermination. A redetermination is a review of the claim by Medicare Administrative Contractor (MAC) personnel not involved in the initial claim determination.
How do I write a Medicare reconsideration letter?
Include this information in your written request:Your name, address, and the Medicare Number on your Medicare card [JPG]The items or services for which you're requesting a reconsideration, the dates of service, and the reason(s) why you're appealing.More items...
What should I say in a Medicare appeal?
What are the steps for filing an appeal for original Medicare?your name and address.your Medicare number (as shown on your Medicare card)the items you want Medicare to pay for and the date you received the service or item.the name of your representative if someone is helping you manage your claim.More items...•
What are the steps taken when appealing a Medicare claim?
Left navigationFile a complaint (grievance)File a claim.Check the status of a claim.File an appeal. Appeals if you have a Medicare health plan. Get help filing an appeal.Your right to a fast appeal.Authorization to Disclose Personal Health Information.
How do you write a redetermination letter?
How to Write an Appeal Letter in 6 Simple StepsReview the appeal process if possible.Determine the mailing address of the recipient.Explain what occurred.Describe why it's unfair/unjust.Outline your desired outcome.If you haven't heard back in one week, follow-up.
What is the difference between reconsideration and redetermination?
Any party to the redetermination that is dissatisfied with the decision may request a reconsideration. A reconsideration is an independent review of the administrative record, including the initial determination and redetermination, by a Qualified Independent Contractor (QIC).
How do I win a Medicare appeal?
Appeals with the best chances of winning are those where something was miscoded by a doctor or hospital, or where there is clear evidence that a doctor advised something and the patient followed that advice and then Medicare didn't agree with the doctor's recommendation.
What are the chances of winning a Medicare appeal?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.
What percentage of Medicare appeals are successful?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
How long does it take Medicare to review an appeal?
about 60 daysHow Long Does a Medicare Appeal Take? You can expect a decision on your Medicare appeal within about 60 days. Officially known as a “Medicare Redetermination Notice,” the decision may come in a letter or an MSN. Medicare Advantage plans typically decide within 14 days.
How do I correct a rejected Medicare claim?
When a claim is denied because the information submitted was incorrect, often the claim can be reopened using a Clerical Error Reopening (CER). CERs can be used to fix errors resulting from human or mechanical errors on the part of the party or the contractor.
Can providers appeal denied Medicare claims?
If you disagree with a Medicare coverage or payment decision, you can appeal the decision. Your MSN contains information about your appeal rights. If you decide to appeal, ask your doctor, other health care provider, or supplier for any information that may help your case.
What is a redetermination request?
The specific item (s) and/or service (s) for which you're requesting a redetermination and the specific date (s) of service. An explanation of why you don't agree with the initial determination. If you've appointed a representative, include the name of your representative.
How long does it take for Medicare to be reconsidered?
You'll generally get a decision from the MAC (either in a letter or an MSN) called a "Medicare Redetermination Notice" within 60 days after they get your request. If you disagree with this decision, you have 180 days after you get the notice to request a reconsideration by a Qualified Independent Contractor (QIC).
How long does it take for Medicare to make a decision?
You can submit additional information or evidence after the filing redetermination request, but, it may take longer than 60 days for the Medicare Administrator Contractor (MAC) that processes claims for Medicare to make a decision. If you submit additional information or evidence after filing, the MAC will get an extra 14 calendar days ...
How long does it take to appeal a Medicare payment?
The MSN contains information about your appeal rights. You'll get a MSN in the mail every 3 months, and you must file your appeal within 120 days of the date you get the MSN.
What information do you put on your MSN?
Include your name, phone number, and Medicare Number on the MSN. Include any other information you have about your appeal with the MSN. Ask your doctor, other health care provider, or supplier for any information that may help your case.
How to request a redetermination of Medicare?
In order to process a Redetermination request, we also need the following pieces of information: 1 The beneficiary's name 2 The Medicare Beneficiary Identifier (MBI) 3 The DOS and the name of the service or item 4 The name of the person filing the Redetermination request 5 Send Redeterminations to the below address:#N#J15 — Part B Correspondence#N#CGS Administrators, LLC#N#PO Box 20018#N#Nashville, TN 37202 6 Medicare Redetermination Request Form
How long does it take to get a Medicare redetermination?
A redetermination is the first level of the Medicare Appeals Process. All requests should be submitted within 120 days of the initial claim determination. Appellants should attach any supporting documentation to their redetermination request.
How long does it take CMS to redetermine a contractor?
Contractors will generally issue a decision (either a letter or a revised remittance advice) within 60 days of receipt of the redetermination request. Please be advised, CMS has instructed all contractors to no longer correct minor errors and omissions on claims through the appeals process.
Why are run tickets denied as part A?
NOTE: Run tickets should be included to support each trip. Charges denied as Part A because the patient was seen in the office prior to admission in the hospital. NOTE: Documentation should be included to support the office service. Claim denied as not medically necessary and a GA modifier has been added to the claim.
Requesting a Redetermination
An initial determination decision is communicated on the beneficiary's Medicare Summary Notice (MSN), and on the provider's, physician's and supplier's Remittance Advice (RA). The appellant (the individual filing the appeal) has 120 days from the date of receipt of the initial claim determination to file a redetermination request.
Dismissal of a Redetermination Request
A MAC may dismiss a request for a redetermination for various reasons, some of which may be:
Redetermination Decision Notification
Generally, the MAC will send its decision (either in a letter, an RA, and/or an MSN) to all parties within 60 days of receipt of the request for redetermination. The decision will contain detailed information on further appeals rights, where applicable.
Fact Sheet: Redetermination Appeals Data
These reports summarize and highlight some of the key data on redeterminations from January 1, 2013 through December 31, 2020. To view the Appeals Fact Sheets, click on the link in the " Downloads " section below.
Redetermination Request Options
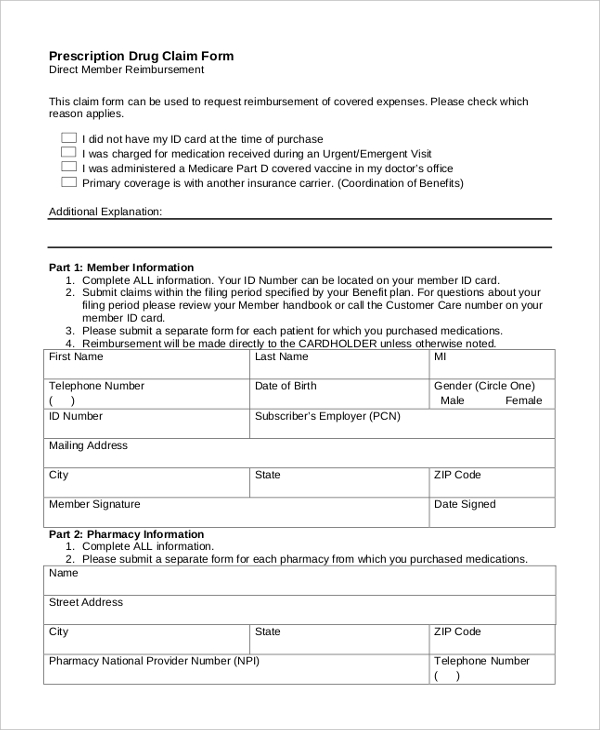
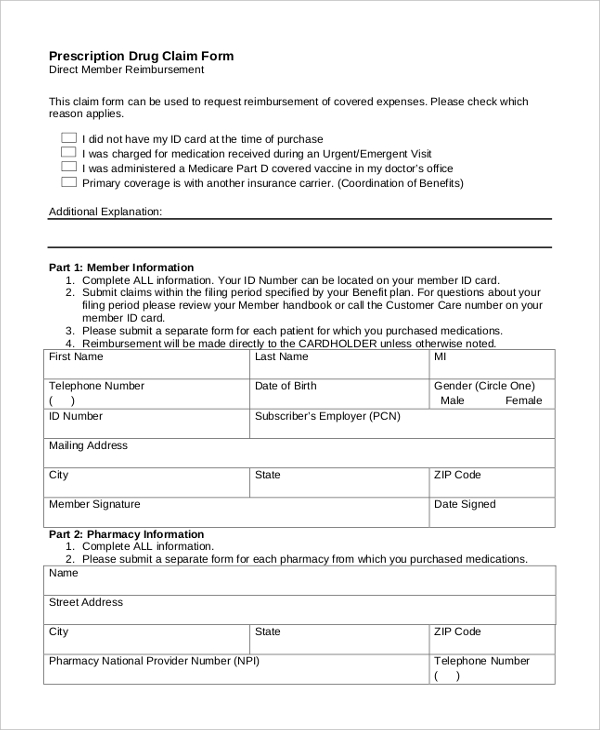
Access the Redetermination/Reopening Form - One request form per beneficiary and issue
Requests Filed on Resubmitted Claims
For appeals of a specific line item or service, the date of the first MSN or RA that states the coverage and payment decision is the date of the initial determination.
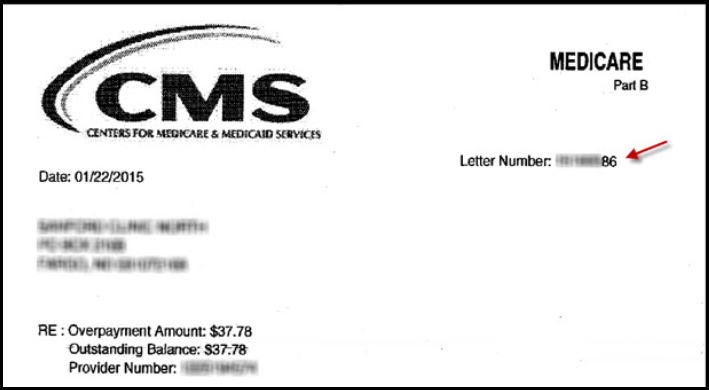
Overpayment Redetermination Request
View the Limitation on Recoupment webpage for information regarding Section 1893 (f) (2) (a) of the Social Security Act, which provides limitations on the recoupment of Medicare overpayments during the appeals process
Good Cause for Extension
Requests made after the 120-day time limit must include an explanation regarding the late file.
Appeal Demand Letter
When Medicare (Noridian) or other outside contractor (Comprehensive Error Rate Testing (CERT), Recover Auditor (RA), Unified Program Integrity Contractor (UPIC) or the Supplemental Medical Review Contractor (SMRC)) determines that an overpayment has occurred, a Demand Letter is issued.
How long does Medicare take to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 calendar days. Payment request—60 calendar days. Learn more about appeals in a Medicare health plan.
How to ask for a prescription drug coverage determination?
To ask for a coverage determination or exception, you can do one of these: Send a completed "Model Coverage Determination Request" form. Write your plan a letter.
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
What to do if you didn't get your prescription yet?
If you didn't get the prescription yet, you or your prescriber can ask for an expedited (fast) request. Your request will be expedited if your plan determines, or your prescriber tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function.
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
How long does it take for a Medicare plan to make a decision?
The plan must give you its decision within 72 hours if it determines, or your doctor tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function. Learn more about appeals in a Medicare health plan.
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.