Two groups of people are eligible for Medicare benefits: adults aged 65 and older, and people under age 65 with certain disabilities. The program was created in the 1960s to provide health insurance for senior citizens.
- People who are 65 or older.
- Certain younger people with disabilities.
- People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
Who is eligible for Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
Is Medicare eligibility different in each state?
Since Medicare is a federal program, eligibility is consistent across the states. Persons must be U.S. Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare.
Do you qualify for Medicare Part A or B?
However, there are now additional ways to qualify for Medicare. Younger people with qualifying disabilities can also be eligible, along with individuals with end-stage renal disease. If you meet certain qualifications, you can get Medicare Part A for free, but Medicare Part B comes with a monthly premium.
What are the two parts of Medicare?
Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance). You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and paid Medicare taxes for at least 10 years.
What population uses Medicare?
Currently, 44 million beneficiaries—some 15 percent of the U.S. population—are enrolled in the Medicare program. Enrollment is expected to rise to 79 million by 2030.
Who is Medicare eligible quizlet?
What is Medicare? Federal program that provides health insurance coverage to people ages 65 and older and younger people with permanent disabilities. The 4 part program covers all those who are eligible regardless of their health status, medical conditions, or incomes.
Which of the following persons would qualify for Medicare Part A?
In general, you are eligible for Medicare Part A if: You are age 65 or older and a U.S. citizen or permanent legal resident of at least five years in a row. You are already receiving retirement benefits. You are disabled and receiving disability benefits.
What are 3 ways to qualify for Medicare?
Who is Eligible for Medicare? You are eligible for Medicare if you are a citizen of the United States or have been a legal resident for at least 5 years and: You are age 65 or older and you or your spouse has worked for at least 10 years (or 40 quarters) in Medicare-covered employment.
At what age are people eligible for Medicare quizlet?
Generally, Medicare is available to people age 65 or older that are U.S citizens or have been continuous permanent legal residents for at least five consecutive years. Eligible individuals or their spouses must have paid Medicare taxes for a minimum of 10 years.
Who is Medicare through?
The Centers for Medicare & Medicaid Services (CMS) is the federal agency that runs Medicare. The program is funded in part by Social Security and Medicare taxes you pay on your income, in part through premiums that people with Medicare pay, and in part by the federal budget.
Who is not eligible for Medicare Part A?
Why might a person not be eligible for Medicare Part A? A person must be 65 or older to qualify for Medicare Part A. Unless they meet other requirements, such as a qualifying disability, they cannot get Medicare Part A benefits before this age. Some people may be 65 but ineligible for premium-free Medicare Part A.
What is the eligibility requirement for Medicare Part B quizlet?
Terms in this set (59) anyone reaching age 65 and qualifying for social security benefits is automatically enrolled into the Medicare part A system and offered Medicare Part B regardless of financial need.
Which of the following are two examples of activities of daily living used in qualifying for long term care benefits?
The law requires tax-qualified policies to pay or reimburse benefits if you are impaired in two out of the following six ADLs: bathing, dressing, transferring, eating, toileting, and continence.
Who is eligible for medical?
To qualify for free Medi-Cal coverage, you need to earn less than 138% of the poverty level, based on the number of people who live in your home. The income limits based on household size are: One person: $17,609. Two people: $23,792.
What is the age for Medicare?
65 or olderMedicare is health insurance for people 65 or older. You're first eligible to sign up for Medicare 3 months before you turn 65. You may be eligible to get Medicare earlier if you have a disability, End-Stage Renal Disease (ESRD), or ALS (also called Lou Gehrig's disease).
How can I qualify for Medicaid?
You may be eligible if you are:65 years of age or older.An individual under 65 years of age who has a disability, or is visually impaired according to Social Security guidelines.An individual 18 years of age or younger.An adult age 19-64.A pregnant woman.A parent or caretaker.A former foster care youth.
How to Enroll in Medicare and When You Should Start Your Research Process
Getting older means making more decisions, from planning for your kids’ futures to mapping out your retirement years. One of the most important dec...
Who Is Eligible to Receive Medicare Benefits?
Two groups of people are eligible for Medicare benefits: adults aged 65 and older, and people under age 65 with certain disabilities. The program w...
When Should You Enroll For Medicare?
Just because you qualify for something doesn’t mean you need to sign up, right? Not always. In the case of Medicare, it’s actually better to sign u...
Can You Delay Medicare Enrollment Even If You Are Eligible?
The short answer here is yes, you can choose when to sign up for Medicare. Even if you get automatically enrolled, you can opt out of Part B since...
What About Medigap Plans?
Original Medicare covers a good portion of your care, but it’s not exhaustive. There’s a wide range of services that Parts A and B don’t cover, inc...
How long do you have to be a US citizen to qualify for Medicare?
To receive Medicare benefits, you must first: Be a U.S. citizen or legal resident of at least five (5) continuous years, and. Be entitled to receive Social Security benefits.
How many parts are there in Medicare?
There are four parts to the program (A, B, C and D); Part C is a private portion known as Medicare Advantage, and Part D is drug coverage. Please note that throughout this article, we use Medicare as shorthand to refer to Parts A and B specifically.
How old do you have to be to get a Medigap policy?
In other words, you must be 65 and enrolled in Medicare to sign up for a Medigap policy. Once you’re 65 and enrolled in Part B, you have six months to enroll in Medigap without being subject to medical underwriting. During this initial eligibility window, you can: Buy any Medigap policy regardless of health history.
How long do you have to sign up for Medicare before you turn 65?
And coverage will start…. Don’t have a disability and won’t be receiving Social Security or Railroad Retirement Board benefits for at least four months before you turn 65. Must sign up for Medicare benefits during your 7-month IEP.
When do you sign up for Medicare if you turn 65?
You turn 65 in June, but you choose not to sign up for Medicare during your IEP (which would run from March to September). In October, you decide that you would like Medicare coverage after all. Unfortunately, the next general enrollment period doesn’t start until January. You sign up for Parts A and B in January.
How long does it take to enroll in Medicare?
If you don’t get automatic enrollment (discussed below), then you must sign up for Medicare yourself, and you have seven full months to enroll.
When does Medicare open enrollment start?
You can also switch to Medicare Advantage (from original) or join a Part D drug plan during the Medicare annual open enrollment period, which runs from October 15 through December 7 each year. Eligibility for Medicare Advantage depends on enrollment in original Medicare.
How many people are dual eligible for medicaid?
Who is the Dual-Eligible Population and Why is Change Needed? There are 12.2 million people nationwide who are simultaneously enrolled in Medicare and Medicaid, a population often referred to as “dual-eligible” beneficiaries.
Why do people get Medicare and Medicaid?
People generally become eligible for both Medicare and Medicaid because they are low-income and are over the age of 65 or are disabled. This means that the dual-eligible population spans young and old, as well as individuals with physical, mental, and developmental disabilities.
What is dual eligible?
Dual-eligible individuals experience much higher rates of chronic disease than the average population, necessitating solutions that take their health challenges into account and work to integrate and streamline their care. Dual-eligible beneficiaries tend to use more health care and need more support than the Medicare-only population.
Why are dual eligible people not homogeneous?
When surveyed, dual-eligible individuals were three times as likely to report that their health was poor, compared to individuals who are enrolled in Medicare only. Because the dual-eligible population is not homogenous, their unique circumstances and needs must be taken into account when developing policy solutions.
Is dual eligibility poor?
OUTCOMES. Despite high spending, the outcomes experienced by dual-eligible individuals are often poor. Dual-eligible individuals are more likely than their Medicare-only counterparts to experience at least one inpatient hospital stay and visit to the emergency room per year.
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
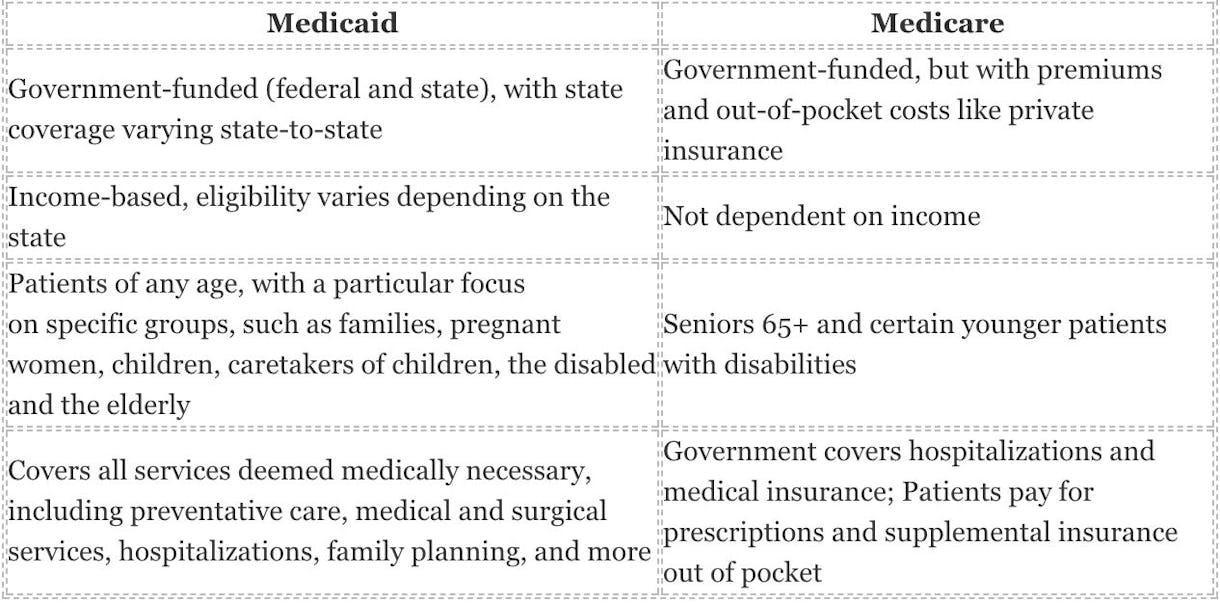
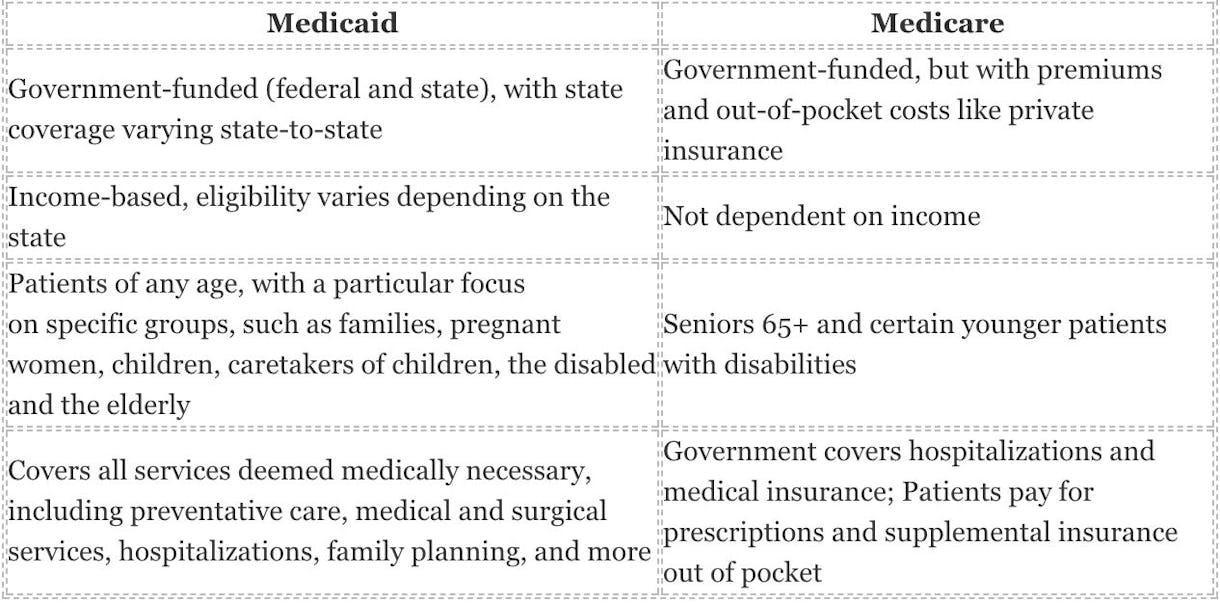
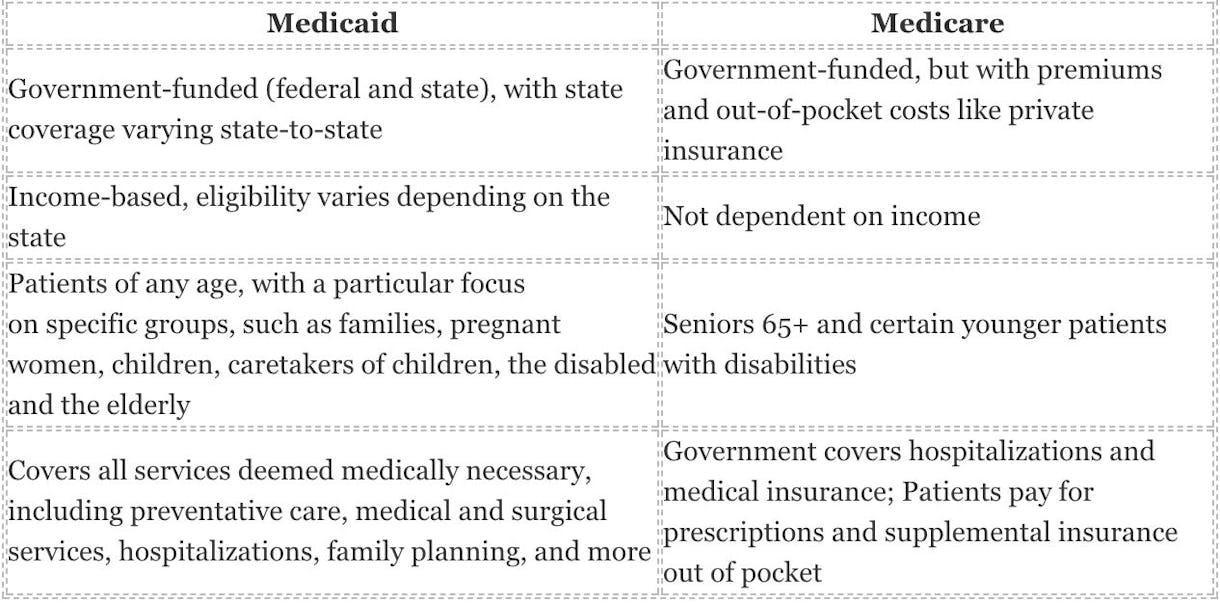
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.