• When you are in hospice care, Medicare does not cover care in a hospital either as an inpatient or outpatient, or ambulance services unless your hospice team makes the arrangements, or if you need this care for reasons that are not related to the terminal illness. Hospital Care
Does Medicare cover you in the hospital?
The hospital accepts Medicare. In certain cases, the Utilization Review Committee of the hospital approves your stay while you’re in the hospital. Your doctor or other health care provider may recommend you get services more often than Medicare covers. Or, they may recommend services that Medicare doesn’t cover.
What are the types of admission codes for a hospital?
Admission Type Code Code Code value 1 Emergency: The patient requires immediat ... 2 Urgent: The patient requires immediate a ... 3 Elective: The patient’s condition permit ... 4 Newborn: The patient is a newborn delive ... 2 more rows ...
Can a patient ask for a service that Medicare does not cover?
A patient may ask for a service that Medicare does not consider medically reasonable and necessary under the circumstances. For instance, the patient wants the service more frequently than Medicare allows or for a diagnosis that Medicare does not cover. You can often verify coverage information by researching the service on the payer’s website.
When is an inpatient admission to a hospital appropriate?
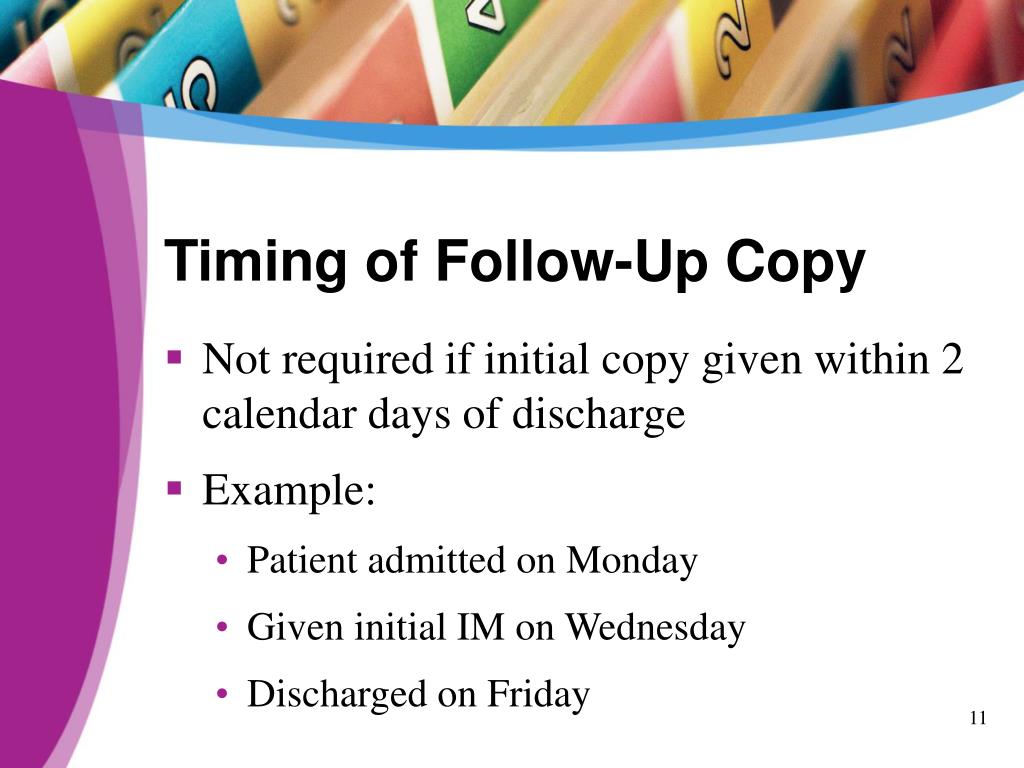
The decision for inpatient hospital admission is a complex medical decision based on your doctor’s judgment and your need for medically necessary hospital care. An inpatient admission is generally appropriate when you’re expected to need 2 or more midnights of medically necessary hospital care.

Which type of care is not covered by Medicare?
does not cover: Routine dental exams, most dental care or dentures. Routine eye exams, eyeglasses or contacts. Hearing aids or related exams or services.
Which item is not covered by Medicare Part A?
Part A does not cover the following: A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care.
What surgical procedures are not covered by Medicare?
Does Medicare Cover Surgery? Medicare covers surgeries that are deemed medically necessary. This means that procedures like cosmetic surgeries typically aren't covered. Medicare Part A covers inpatient procedures, while Part B covers outpatient procedures.
Does Medicare a cover hospitalization?
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
Which of the following services would not be covered under Medicare Part B?
But there are still some services that Part B does not pay for. If you're enrolled in the original Medicare program, these gaps in coverage include: Routine services for vision, hearing and dental care — for example, checkups, eyeglasses, hearing aids, dental extractions and dentures.
Which of the following services is not included under hospitalization expense coverage?
Which of the following services is NOT covered under a hospitalization expense policy? Surgeon's fees. (While an insured is hospitalized, the hospitalization expense coverage includes benefits for the cost of all of these services EXCEPT a surgeon's fees.)
How do I know if Medicare will cover a procedure?
Ask the doctor or healthcare provider if they can tell you how much the surgery or procedure will cost and how much you'll have to pay. Learn how Medicare covers inpatient versus outpatient hospital services. Visit Medicare.gov or call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
Does Medicare cover ICU costs?
(Medicare will pay for a private room only if it is "medically necessary.") all meals. regular nursing services. operating room, intensive care unit, or coronary care unit charges.
Do all hospitals accept Medicare?
Not all hospitals accept Medicare, but luckily, the vast majority of hospitals do. Generally, the hospitals that do not accept Medicare are Veterans Affairs and active military hospitals (they operate with VA and military benefits instead), though there are a few other exceptions nationwide.
Does Medicare cover Covid hospitalization?
If an inpatient hospitalization is required for treatment of COVID-19, this treatment will be covered for Medicare beneficiaries, including beneficiaries in traditional Medicare and those in Medicare Advantage plans.
Can you claim Medicare on private hospital?
Medicare generally covers 75% of the fees for treatment as a private patient in a public or private hospital.
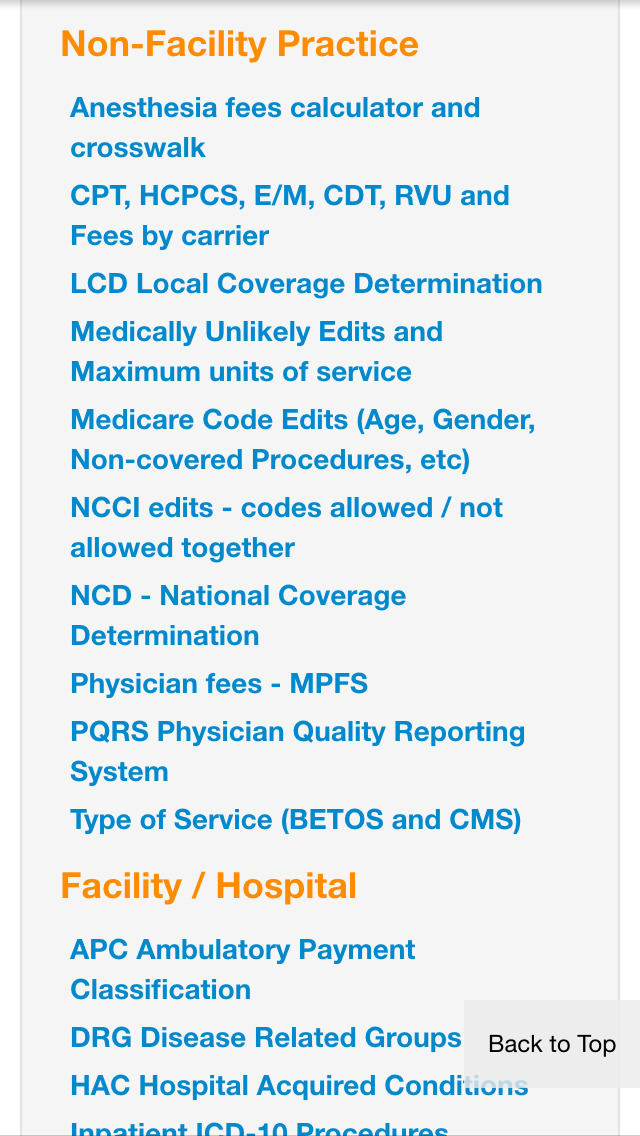
What are non covered services?
Medicare Non-covered Services. There are two main categories of services which a physician may not be paid by Medicare: Services not deemed medically reasonable and necessary. Non-covered services. In some instances, Medicare rules allow a physician to bill the patient for services in these categories. Understanding these rules and how ...
What is an ABN for Medicare?
If a Medicare patient wishes to receive services that may not be considered medically reasonable and necessary, or you feel Medicare may deny the service for another reason, you should obtain the patient’s signature on an Advance Beneficiary Notice (ABN).
When Medicare or another payer designates a service as “bundled,” does it make separate payment for the pieces of the
When Medicare or another payer designates a service as “bundled,” it does not make separate payment for the pieces of the bundled service and does not permit you to bill the patient for it since the payer considers payment to already be included in payment for another service that it does cover. Coordination of Benefits.
Is it reasonable to ask for a service from Medicare?
Medically Reasonable and Necessary. A patient may ask for a service that Medicare does not consider medically reasonable and necessary under the circumstances. For instance, the patient wants the service more frequently than Medicare allows or for a diagnosis that Medicare does not cover.
Do commercial insurance companies have similar coverage guidelines?
Commercial insurance companies and some Medicaid payers will have similar types of information about their coverage guidelines on their websites. Stay up-to-date on these policies for your local payers to ensure claims are processed as medically reasonable and necessary.
Can you bill for a non-covered medical visit?
For instance, in the case of a medically-necessary visit on the same occasion as a preventiv e medicine visit, you may bill for the non-covered (carved-out) preventive visit, but must subtract your charge for the covered service from your charge for the non-covered service.
Does Medicare require an ABN?
Medicare requires an ABN be signed by the patient prior to beginning the procedure before you can bill the patient for a service Medicare denies as investigational or not medically necessary. Otherwise, Medicare assumes the patient did not know and prohibits the patient from being liable for the service.
What age do you have to be to get Medicare?
If you are close to the age of 65 and soon to be eligible for Medicare insurance, you may be doing some homework on Medicare coverage. In most cases, it is equally as important to know what Original Medicare covers ...
What does Medicare mean for retirement?
For many people at retirement age, having Medicare benefits means the difference between getting quality health care and not being able to visit a doctor.
Does Medicare cover long term care?
Long-term, or custodial care that takes place either in a skilled nursing facility or in your own home, is not included in Medicare insurance coverage. Part A insurance does cover short-term stays in skilled nursing care facilities and home health care on a part-time, or intermittent, basis. But even this short-term care does not include custodial ...
Is dental insurance covered by Medicare?
1. Routine dental care and dentures are not included in Medicare insurance coverage. Examples of this sort of care include: • Check-ups. • Cleaning. • Fillings. • Extractions. • Dentures, dental plates, other orthodontic or dental devices.
Does Medicare pay for custodial care?
But even this short-term care does not include custodial care services. Custodial care includes things like meal preparation and feeding, bathing, dressing, or personal hygiene care. In cases of home health care, Medicare does not pay for the following services: • 24-hour care. • Meals delivered to the home.
Does Medicare cover hospice?
Hospice. Once your hospice care benefits begin, Medicare does not cover the following: • Treatment to cure our terminal illness or any related conditions. • Any prescription drugs meant to cure the illness, other than drugs administered for pain relief or symptom control.
Does Medicare cover self-administered prescriptions?
Unless you have a separate Part D policy, Original Medica re does not cover self-administered prescription drug costs. Your prescription drugs needed during hospital inpatient stays are covered by Part A. Drugs covered under Part B are those that your health care provider administers in a medical office or facility.
When is an inpatient admission appropriate?
An inpatient admission is generally appropriate when you’re expected to need 2 or more midnights of medically necessary hospital care. But, your doctor must order such admission and the hospital must formally admit you in order for you to become an inpatient.
How does hospital status affect Medicare?
Inpatient or outpatient hospital status affects your costs. Your hospital status—whether you're an inpatient or an outpatient—affects how much you pay for hospital services (like X-rays, drugs, and lab tests ). Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility ...
What is an ED in hospital?
You're in the Emergency Department (ED) (also known as the Emergency Room or "ER") and then you're formally admitted to the hospital with a doctor's order. Outpatient until you’re formally admitted as an inpatient based on your doctor’s order. Inpatient after your admission.
How long does an inpatient stay in the hospital?
Inpatient after your admission. Your inpatient hospital stay and all related outpatient services provided during the 3 days before your admission date. Your doctor services. You come to the ED with chest pain, and the hospital keeps you for 2 nights.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. , coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles.
Is an outpatient an inpatient?
You're an outpatient if you're getting emergency department services, observation services, outpatient surgery, lab tests, or X-rays, or any other hospital services, and the doctor hasn't written an order to admit you to a hospital as an inpatient. In these cases, you're an outpatient even if you spend the night in the hospital.
Does Medicare cover skilled nursing?
Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility (SNF) following your hospital stay. You're an inpatient starting when you're formally admitted to the hospital with a doctor's order. The day before you're discharged is your last inpatient day. You're an outpatient if you're getting ...
Does Medicare cover exceptions?
This booklet outlines the 4 categories of items and services Medicare doesn’t cover and exceptions (items and services Medicare may cover). This material isn’t an all-inclusive list of items and services Medicare may or may not cover.
Does Medicare cover personal comfort items?
Medicare doesn’t cover personal comfort items because these items don’t meaningfully contribute to treating a patient’s illness or injury or the functioning of a malformed body member. Some examples of personal comfort items include:
Does Medicare cover non-physician services?
Medicare normally excludes coverage for non-physician services to Part A or Part B hospital inpatients unless those services are provided either directly by the hospital/SNF or under an arrangement that the hospital/SNF makes with an outside source.
Does Medicare cover dental care?
Medicare doesn’t cover items and services for the care, treatment, filling, removal, or replacement of teeth or the structures directly supporting the teeth, such as preparing the mouth for dentures, or removing diseased teeth in an infected jaw. The structures directly supporting the teeth are the periodontium, including:
Can you transfer financial liability to a patient?
To transfer potential financial liability to the patient, you must give written notice to a Fee-for-Service Medicare patient before furnishing items or services Medicare usually covers but you don’ t expect them to pay in a specific instance for certain reasons, such as no medical necessity .
What does Medicare not cover?
Medicare does not cover: 1 examinations for life insurance, superannuation or memberships for which someone else is responsible (for example, a compensation insurer, employer or government authority); 2 ambulance services; 3 most dental examinations and treatment; 4 most physiotherapy, occupational therapy, speech therapy, eye therapy, chiropractic services, podiatry or psychology services; 5 acupuncture (unless part of a doctor's consultation); 6 glasses and contact lenses; 7 hearing aids and other appliances; and 8 home nursing.
What are the services that are offered by a doctor?
most physiotherapy, occupational therapy, speech therapy, eye therapy, chiropractic services, podiatry or psychology services; acupuncture (unless part of a doctor's consultation); glasses and contact lenses; hearing aids and other appliances; and. home nursing.
What are the benefits of Medicare?
Medicare provides benefits for: consultation fees for doctors, including specialists; tests and examinations by doctors needed to treat illnesses, such as x-rays and pathology tests; eye tests performed by optometrists; most surgical and other therapeutic procedures performed by doctors; some surgical procedures performed by approved dentists;
Does Medicare cover dental insurance?
Medicare does not cover: examinations for life insurance, superannuation or memberships for which someone else is responsible (for example, a compensation insurer, employer or government authority); ambulance services; most dental examinations and treatment; most physiotherapy, occupational therapy, speech therapy, eye therapy, ...
Can you be a public patient under Medicare?
Under Medicare you can be treated as a public patient in a public hospital, at no charge, by a doctor appointed by the hospital. You can choose to be treated as a public patient, even if you are privately insured.
Does Medicare cover GP?
Medicare will also cover some or all the costs of seeing a GP or specialist outside of hospital, and some pharmaceuticals. Medicare does not cover private patient hospital costs, ambulance services, and other out of hospital services such as dental, physiotherapy, glasses and contact lenses, hearings aids. Many of these items can be covered on ...
What is noncompliance in Medicare?
Noncompliance will be considered in determining whether the provider is honoring its agreement, under which it may not charge for services for which payment may be made under the Medicare program.
What is M+CO in Medicare?
The provider must ascertain whether the patient is a member of a Medicare + Choice organization (M+CO). If the patient is a member of an M+CO, the provider must contact the M+CO specified by the patient or identified on the patient’s membership card, so the provider may determine whether to submit the claim to the M+CO.
What is encounter in medical?
The term “encounter” means a direct personal contact in the hospital between a patient and a physician, or other person who is authorized by State law and, if applicable, by hospital staff bylaws to order or furnish services for diagnosis or treatment of the patient. Direct personal contact does not include telephone contacts between a patient and physician. Nor is the compensation arrangement between the physician and the hospital relevant to whether an encounter has occurred. Patients will be treated as hospital outpatients for purposes of billing for certain diagnostic services that are ordered during or as a result of an encounter that occurred while such patients are in an outpatient status at the hospital. If a Medicare outpatient is referred to another provider or supplier for further diagnostic testing or other diagnostic services as a result of an encounter that occurs in this hospital, the hospital is responsible for arranging with the other entity for the furnishing of services. Hospitals are not required to verify that all ordered services are furnished but only to assure that, when it is necessary to refer a patient to an outside entity, the referral is made to a provider or supplier with which the referring hospital an arrangement. This requirement is necessary to assure that billing for services that are furnished is processed through the servicing hospital.
Can a provider collect a deductible?
The provider may collect deductible or coinsurance amounts only where it appears that the patient will owe deductible or coinsurance amounts and where it is routine and customary policy to request similar prepayment from non-Medicare patients with similar benefits that leave patients responsible for a part of the cost of their hospital services. In admitting or registering patients, the provider must ascertain whether beneficiaries have medical insurance coverage. Where beneficiaries have medical insurance coverage, the provider asks the beneficiary if he/she has a Medicare Summary Notice (MSN) showing his/her deductible status. If a beneficiary shows that the Part B deductible is met, the provider will not request or require prepayment of the deductible.