- Medicare is a type of health insurance
- Medicare offers hospital and medical insurance
- Medicare offers Prescription Drug benefits
- Medicare has Gap insurance to cover deductibles and coinsurance
- Medicare provides total health insurance plans
What are the best insurance companies for Medicare?
Top 10 Medicare Supplement Insurance Companies in 2021
- Aetna Medicare Supplements
- Cigna Medicare Supplements
- Mutual of Omaha Medicare Supplements
- Manhattan Life Medicare Supplements
- Bankers Fidelity Medicare Supplements
- Blue Cross Blue Shield Medicare Supplements
- Western United Life Medicare Supplements
- Anthem Medicare Supplements
- United Healthcare Medicare Supplements
- Combined Medicare Supplements
What other insurance do I need with Medicare?
What it means to pay primary/secondary
- The insurance that pays first (primary payer) pays up to the limits of its coverage.
- The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover.
- The secondary payer (which may be Medicare) may not pay all the uncovered costs.
Is Medicare the only health insurance I Need?
The answer is: It depends. For many low-income Medicare beneficiaries, there’s no need for private supplemental coverage. Almost one in five Medicare beneficiaries are dual eligible for both Medicare and Medicaid. Failed to initialize the widget.
What does insurances pay primary to Medicare?
What it means to pay primary/secondary The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the remaining costs.

What type of insurance is Medicare?
Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles).
What are the 3 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Is Medicare a primary or group?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
Is Medicare a type of healthcare?
Medicare is the federal government program that provides health care coverage (health insurance) if you are 65+, under 65 and receiving Social Security Disability Insurance (SSDI) for a certain amount of time, or under 65 and with End-Stage Renal Disease (ESRD).
Which is better PPO or HMO?
HMO plans typically have lower monthly premiums. You can also expect to pay less out of pocket. PPOs tend to have higher monthly premiums in exchange for the flexibility to use providers both in and out of network without a referral. Out-of-pocket medical costs can also run higher with a PPO plan.
What is Plan B Medicare?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services. Part B also covers some preventive services. Look at your Medicare card to find out if you have Part B.
Is Medicare Advantage plan primary or secondary?
Is Medicare Advantage Primary or Secondary? When you enroll in a Medicare Advantage plan, the carrier pays for your medical care instead of Medicare. Therefore, Medicare is no longer responsible to pay your claims. Your Medicare Advantage plan is your primary, and only, coverage.
How do you determine which insurance is primary?
Primary insurance is a health insurance plan that covers a person as an employee, subscriber, or member. Primary insurance is billed first when you receive health care. For example, health insurance you receive through your employer is typically your primary insurance.
What is the difference between Medicare and Medicaid?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
What are the 4 types of health insurance?
Types of Health Insurance Plans: HMO, PPO, HSA, Fee for Service, POS.
Is Medicare the same as health insurance?
Medicare provides health coverage to individuals 65 and older or those with a severe disability regardless of income, whereas Medi-Cal (California's state-run and funded Medicaid program) provides health coverage to those families with very low income, as well as pregnant women and the blind, among others.
Does everyone get Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is Medicare insurance?
Medicare is a type of health insurance. Medicare offers hospital and medical insurance. Medicare offers Prescription Drug benefits. Medicare has Gap insurance to cover deductibles and coinsurance. Medicare provides total health insurance plans. Medicare offers a wide range of coverage and benefits for older Americans.
What is Medicare Advantage?
The Medicare Advantage was meant to add private sector initiatives to stimulate competition and variety. The below-listed Medicare parts describe features that applicants can choose. Hospital Insurance Medicare Part A is the basic coverage of Medicare. Part A coverage meets the requirements of the Affordable Care Act and the individual mandate.
How old do you have to be to qualify for Medicare?
Usually, older Americans qualify for Medicare by reaching the retirement age of 65. They can apply for Medicare benefits at the same time they apply for retirement benefits from social security. A clock begins to run at this time, and if they did not select benefits they will pay more later in late fees. The initial enrollment period is ...
Why is Medicare management important?
As the largest federal health program, Medicare management is a top priority for controlling costs, improving performance, and improving patient outcomes. Medicare moves to value-based purchasing in its relationships with medical care providers and hospitals.
Is Medicare a comprehensive health system?
Medicare is a Comprehensive Health System. From state of the art research to hospice care for people with little or no family, the Medicare system shows a remarkable ability to perform its vital humanitarian work. One can measure the quality of society by the treatment of the old and most vulnerable members.
What age does Medicare cover?
Medicare provides healthcare coverage to people over age 65 and those with disabilities or certain health conditions . This complex program has many parts, and it involves the federal government and private insurers working together to offer a wide variety of services and products.
What is Medicare Part C?
Medicare Part C (Medicare Advantage) is a private insurance product that gives you all the coverage of Medicare parts A and B, plus extra services. Most of these plans offer prescription coverage in addition to inpatient and outpatient services. Benefits like dental and vision coverage can be added too.
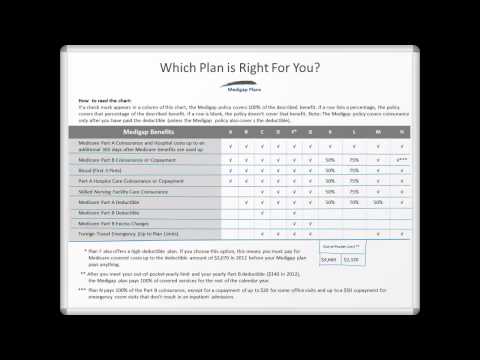
What is a Medigap plan?
Coverage. Plan A. Medicare Part A coinsurance and the costs of 365 days’ worth of care after Medicare benefits are exhausted, Part B coinsurance or copayments, the first 3 pints of a blood transfusion, and hospice care coinsurance or copayments. Plan B.
How much will Medicare cost in 2021?
Under Medicare Part B, you can expect to pay the following costs in 2021: a premium of at least $148.50 per month (this amount increases if your individual income is above $88,000 per year or $176,000 per year for married couples) a $203 deductible for the year.
How much is coinsurance for a 61 day stay?
a $1,484 deductible for each benefit period. daily coinsurance costs based on the the length of your inpatient stay: $0 for days 1 to 60, $371 per day for days 61 to 90, and $742 per day for days 91 and beyond.
Does Medicare cover outpatient prescriptions?
some outpatient prescription medications. To be sure Medicare Part B covers your appointment, service, or medical equipment, ask if your doctor or service provider accepts Medicare. You can also use the Medicare coverage tool to determine whether your appointment or service is covered.
Is Medicare Advantage a private insurance?
Premiums and copayments apply, but they’re usually income-based and may be subsidized. Medicare Advantage (Part C) plans are private insurance plans. These plans combine multiple elements of Medicare, like parts A and B , with other services, such as prescription, dental, and vision coverage.
Medicare Eligibility, Applications, and Appeals
Find information about Medicare, how to apply, report fraud and complaints.
Voluntary Termination of Medicare Part B
You can voluntarily terminate your Medicare Part B (medical insurance). It is a serious decision. You must submit Form CMS-1763 ( PDF, Download Adobe Reader) to the Social Security Administration (SSA). Visit or call the SSA ( 1-800-772-1213) to get this form.
Medicare Prescription Drug Coverage (Part D)
Part D of Medicare is an insurance coverage plan for prescription medication. Learn about the costs for Medicare drug coverage.
Replace Your Medicare Card
You can replace your Medicare card in one of the following ways if it was lost, stolen, or destroyed:
Medicare Coverage Outside the United States
Medicare coverage outside the United States is limited. Learn about coverage if you live or are traveling outside the United States.
Do you have a question?
Ask a real person any government-related question for free. They'll get you the answer or let you know where to find it.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
Can you cancel a Medigap policy?
This means the insurance company can't cancel your Medigap policy as long as you pay the premium. Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is a health care provider?
Tell your doctor and other. health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. about any changes in your insurance or coverage when you get care.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What happens if you don't sign up for Medicare?
If you don’t sign up within seven months of turning 65 (three months before your 65 th birthday, your birthday month, and three months after), you will pay a 10% penalty for every year you delay. Enroll in a Medicare Advantage plan, which is a privately-run health plan approved by the government to provide Medicare benefits.
Does Part D cover prescriptions?
It will help cover the cost of your prescription medications. Similar to Part B, there is a financial penalty if you do not sign up for a Part D plan when you are first eligible, unless you have other prescription drug coverage.