What is a 20% discount for Medicare Part B drugs?
Medicare coverage for many tests, items, and services depends on where you live. This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live. Your Medicare coverage choices. Learn about the 2 main ways to get your Medicare coverage — Original Medicare or a Medicare Advantage Plan ...
Is there a 20% copay for Medicare Advantage?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage; Creditable Prescription Drug Coverage In general, you'll have to pay this penalty for as long as you have a Medicare drug plan. The cost of the late enrollment penalty depends on how long you went without Part D or creditable prescription …
What is a Medicare drug list?
· Under new rules, Medigap Plans C and F will no longer be available for most people who are enrolling in Medicare for the first time on or after January 1, 2020. The exception is for people who were 65 or older on January 1 and thus eligible for …
What do I need to know about Medicare prescription drug coverage?
· Special Needs Plans give you tailored coverage. SNPs have three different categories for health coverage. Medicare SNPs limit membership to one of the three plan types. The three types of Special Needs Plans include Chronic Condition SNP, Institutional SNP, and Dual-Eligible SNP. Most SNPs are Health Maintenance Organizations (HMOs).
Which Medicare type covers prescriptions?
While Medicare Part D covers your prescription drugs in most cases, there are circumstances where your drugs are covered under either Part A or Part B. Part A covers the drugs you need during a Medicare-covered stay in a hospital or skilled nursing facility (SNF).
What are the 4 standardized levels of Medicare prescription drug coverage?
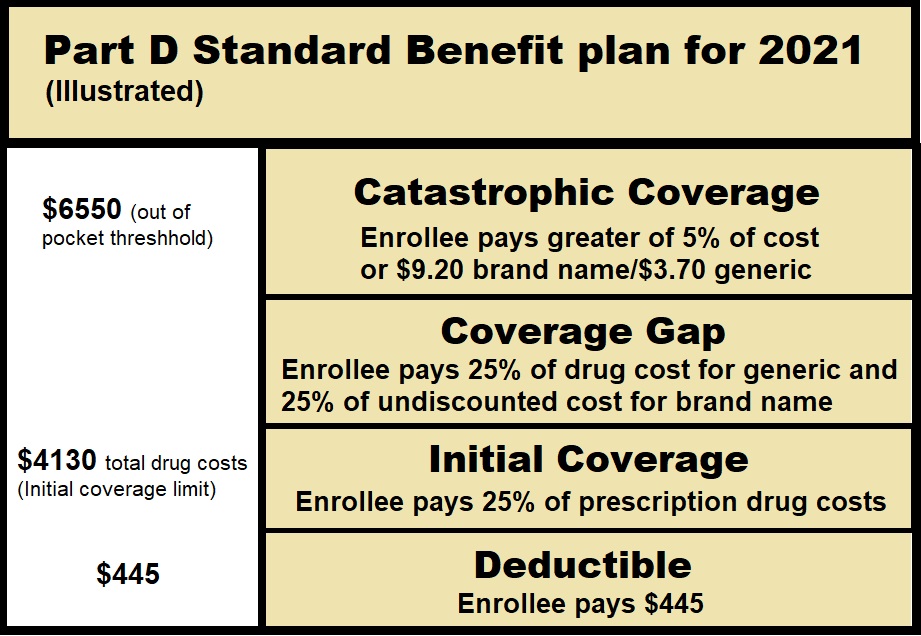
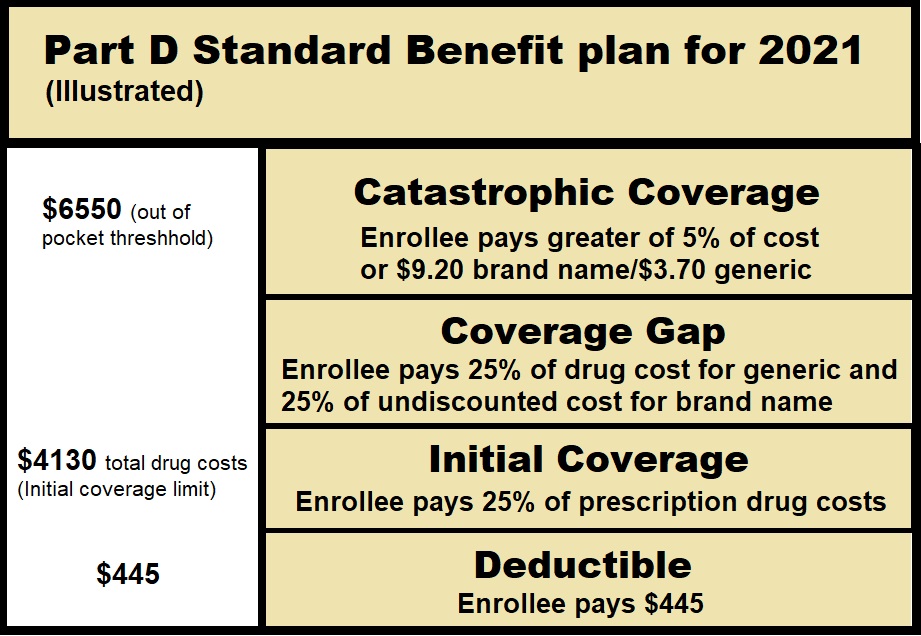
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.
What is a Tier 1 prescription?
There are typically three or four tiers: Tier 1: Least expensive drug options, often generic drugs. Tier 2: Higher price generic and lower-price brand-name drugs. Tier 3: Mainly higher price brand-name drugs. Tier 4: Highest cost prescription drugs.
What is the difference between Part C and Part D Medicare?
Medicare Part C is an alternative to original Medicare. It must offer the same basic benefits as original Medicare, but some plans also offer additional benefits, such as vision and dental care. Medicare Part D, on the other hand, is a plan that people can enroll in to receive prescription drug coverage.
What is plan G Medicare?
Plan G is a supplemental Medigap health insurance plan that is available to individuals who are disabled or over the age of 65 and currently enrolled in both Part A and Part B of Medicare. Plan G is one of the most comprehensive Medicare supplement plans that are available to purchase.
How do you know what tier your prescriptions are?
The easiest way to find out what tier your drugs are in is by using your plan's drug list. When you look up a drug, the second column of the drug list will show you what tier it's in. You can find out more about how to read a drug list in our Help Center. Find your plan's drug list.
Is Metformin a Tier 1 drug?
What drug tier is metformin typically on? Medicare prescription drug plans typically list metformin on Tier 1 of their formulary.
What do drug tiers mean?
Drug tiers are a way for insurance providers to determine medicine costs. The higher the tier, the higher the cost of the medicine for the member in general. If you look at your insurance card, you'll see the copay values for all the tiers under your insurance plan.
Is omeprazole a Tier 1 drug?
What drug tier is omeprazole typically on? Medicare prescription drug plans typically list omeprazole on Tier 1 of their formulary. Generally, the higher the tier, the more you have to pay for the medication. Most plans have 5 tiers.
Does Medicare Part D cover prescriptions?
Medicare Part D, the prescription drug benefit, is the part of Medicare that covers most outpatient prescription drugs. Part D is offered through private companies either as a stand-alone plan, for those enrolled in Original Medicare, or as a set of benefits included with your Medicare Advantage Plan.
Does Medicare Part B pay for prescriptions?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers a limited number of outpatient prescription drugs under certain conditions.
Does Medicare C cover prescriptions?
Unlike Original Medicare, Medicare Part C generally offers coverage for prescription drugs you take at home. The exact prescription drugs that are covered are listed in the plan's formulary. Formularies may vary from plan to plan.
What is Medicare drug coverage?
You'll make these payments throughout the year in a Medicare drug plan: A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list. ).
When will Medicare start paying for insulin?
Look for specific Medicare drug plan costs, and then call the plans you're interested in to get more details. Starting January 1, 2021, if you take insulin, you may be able to get Medicare drug coverage that offers savings on your insulin.
Why are my out-of-pocket drug costs less at a preferred pharmacy?
Your out-of-pocket drug costs may be less at a preferred pharmacy because it has agreed with your plan to charge less. A Medicare program to help people with limited income and resources pay Medicare prescription drug program costs, like premiums, deductibles, and coinsurance. paying your drug coverage costs.
What is formulary in insurance?
Your prescriptions and whether they’re on your plan’s list of covered drugs (. formulary. A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
How much will Medicare cost in 2021?
Most people don't pay a monthly premium for Part A (sometimes called " premium-free Part A "). If you buy Part A, you'll pay up to $471 each month in 2021. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $471. If you paid Medicare taxes for 30-39 quarters, the standard Part A premium is $259.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
What medical equipment is ordered by your doctor for use in the home?
Certain medical equipment, like a walker, wheelchair, or hospital bed, that's ordered by your doctor for use in the home.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
How much is the Part B premium for 91?
Part B premium. The standard Part B premium amount is $148.50 (or higher depending on your income). Part B deductible and coinsurance.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How long does a SNF benefit last?
The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins. You must pay the inpatient hospital deductible for each benefit period. There's no limit to the number of benefit periods.
Who sells Medicare Advantage plans?
Medicare Advantage plans are sold by private insurers who offer the same coverage as Original Medicare. These plans often offer extra benefits such as vision and dental.
What is Medicare Supplement Insurance?
Many people who choose Original Medicare instead of Medicare Advantage purchase Medicare Supplement insurance, also known as Medigap. There are 10 active Medigap plan types, which are identified by letter – like Plan D, Plan K, or Plan M. Medigap helps cover premiums, copayments and additional out-of-pocket costs that Original Medicare doesn’t cover.
Is Medicare coverage available to everyone?
Keep in mind, however, that unlike the uniform medical coverage offered to everyone enrolled in any type of Medicare plan, these expanded benefits are not available to everyone. Before you sign up for one of these expanded plans, be sure you know the limits involved, warns David Lipschutz, senior policy attorney at the Center for Medicare Advocacy.
Will Medicare Advantage plan include additional benefits?
This year, however, a large number of Medicare Advantage plans are expected to include additional benefits. In addition, the government is allowing even more non-medical benefits for plan year 2020, especially for people with chronic illnesses.
When will Medicare changes take effect?
Individual plan costs and benefits can change often. These Medicare changes that will take effect in January may impact your decision. Here’s what you need to know to help find the Medicare coverage that’s best for you.
Does Medicare cover prescription drugs?
Most important, look for changes in your Medicare prescription drug plan. Don’t assume that your plan’s formulary, the list of prescription drugs covered by your Part D or Medicare Advantage plan, is permanent. These lists change every year.
What is Medicare Special Needs Plan?
Medicare Advantage Special Needs Plans offer tailored plan options to Medicare beneficiaries with certain health issues. Those with Medicare and Medicaid are eligible for another type of Medicare Special Needs Plan. Just as all people have individual medical needs, not all health conditions are generic. You may find your medical needs can be quite complicated but this doesn’t mean your coverage should be too. A branch of Medicare Advantage plans known as Medicare Special Needs Plans (SNPs) may be able to further help with extra coverage options.
What are the different types of SNPs?
Medicare SNPs limit membership to one of the three plan types. The three types of Special Needs Plans include Chronic Condition SNP, Institutional SNP, and Dual-Eligible SNP. Most SNPs are Health Maintenance Organizations (HMOs).
What are SNP restrictions?
Restrictions may include receiving health care and services from providers within the SNP’s network. Exceptions for care include if a beneficiary suffers a sudden illness requiring the E.R. or urgent care services or if a beneficiary has End-Stage Renal Disease (ESRD) requiring dialysis out of the service area.
What is a dual SNP?
Dual-Eligible SNP (D-SNP) Beneficiaries who have both Medicare and Medicaid coverage are dual-eligible. D-SNPs provide coverage to these individuals. All levels of Medicaid beneficiaries are eligible for this coverage.
Can special needs plans free up expenses?
We can help find the right Medicare plan for your needs. For eligible beneficiaries, Special Needs Plans may free up some monthly expenses.
Does Medicare cover SNPs?
To be clear, SNPs must provide all the coverage Original Medicare includes, as well as Part D pre scription drug coverage. Medicare Special Needs Plans offer extra coverage options to help the management of your specific circumstance or disease.
What happens if you don't agree with Medicare disenrollment?
If you happen to get a notice of dis-enrollment, and you don’t agree with the terms – you have the right to file an appeal. Should your plan disagree with your appeal, an independent organization will look over the forms. These organizations work for Medicare, not for your SNP plan. So, no need to worry about a biased decision.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
Does Medicare pay for nursing home care?
Depending on what kind of coverage you have , Medicare may pay for your health care and prescription drugs while you're in a nursing home.
Can you switch Medicare plans in a nursing home?
If you move in or out of a nursing home or other institution, you can switch Medicare drug plans at that time. In this situation, “other institutions” do not include assisted living, adult living facilities, residential homes, or any kind of nursing home that’s not certified by Medicare or Medicaid.
Does Medicare automatically enroll people in nursing homes?
If you have Medicare & live in a nursing home or other institution, you should know: Unless you choose a Medicare Advantage Plan with prescription drug coverage or a Medicare Prescription Drug Plan on your own, Medicare automatically enrolls people with both Medicare and full Medicaid coverage living in institutions into Medicare Prescription Drug ...
Does Medicare cover long term care?
This coverage is offered by insurance companies and other private companies approved by Medicare. and live in a nursing home or other institution, you’ll get your covered prescriptions from a long-term care pharmacy that works with your plan.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. (like an HMO or PPO) or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Is SNF covered by Medicare?
If you're in a skilled nursing facility (SNF) getting Medicare-covered. skilled nursing care. Care like intravenous injections that can only be given by a registered nurse or doctor. , your prescriptions generally will be covered by Part A.
How many reserve days can you use for Medicare?
You may use up to 60 lifetime reserve days at a per-day charge set by Medicare for days 91–150 in a benefit period. You pay 100 percent of the cost for day 150 and beyond in a benefit period. Your inpatient rehab coverage and costs may be different with a Medicare Advantage plan, and some costs may be covered if you have a Medicare supplement plan. ...
How many days do you pay Medicare per day?
You pay a per-day charge set by Medicare for days 21–100 in a benefit period.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How long do you pay nothing for Medicare?
You usually pay nothing for days 1–60 in one benefit period, after the Part A deductible is met.
How long does it take to get Medicare to cover rehab?
The 3-day rule for Medicare requires that you are admitted to the hospital as an inpatient for at least 3 days for rehab in a skilled nursing facility to be covered. You must be officially admitted to the hospital by a doctor’s order to even be considered an inpatient, so watch out for this rule. In cases where the 3-day rule is not met, Medicare ...
How long does Medicare cover inpatient rehab?
Medicare covers inpatient rehab in a skilled nursing facility – also known as an SNF – for up to 100 days. Rehab in an SNF may be needed after an injury or procedure, like a hip or knee replacement.
What is Medicare Part A?
Published by: Medicare Made Clear. Medicare Part A covers medically necessary inpatient rehab (rehabilitation) care , which can help when you’re recovering from serious injuries, surgery or an illness. Inpatient rehab care may be provided in of the following facilities: A skilled nursing facility.
How much is Medicare premium for 2020?
Most 2020 Medicare members must pay a monthly premium of $144.60. If you don't enroll in Medicare Part B as soon as you are eligible, you could be assessed a late enrollment penalty when you do enroll. The penalty could be as high as a 10% increase in your premium for each 12-month period that you were eligible but not enrolled.
Who offers Medicare Advantage plans?
Medicare Advantage plans are offered by private insurance companies contracted by the federal government, so they vary in cost, coverage, deductibles and copays.
How much is the penalty for Part D 2020?
The penalty for 2020 is the “national base premium,” which is $32.74 per month , times the number of months that you weren’t covered. This penalty is assessed when you enroll, and you’ll pay the higher amount for as long as you keep your Part D coverage. Your Part D premium could be higher depending on your income.
What is Medicare Part D?
Medicare Part D – prescription drug coverage. Medicare Part D covers prescriptions drugs. Plan premiums, the drugs that are covered, deductibles, coinsurance and copays will vary by plan, so you should check and compare plans each year based on your needs, the prescription drugs you take, etc.
Is Medicare Advantage the same as Medicare Part A?
Medicare Advantage plans are required by law to provide—at minimum—the same coverage, benefits and rights provided by Original Medicare Part A and Part B, with the exception of hospice care.
How much is the deductible for Medicare Part B 2020?
There is a $198 annual deductible for Medicare Part B in 2020. After the deductible, you’ll pay a 20% copay for most doctor services while hospitalized, as well as for DME and outpatient therapy. There is a 20% copay of the Medicare-approved amount for doctor visits to diagnose a mental health condition after the deductible.
How much is the penalty for Medicare Part B?
Your Part B premium could be higher depending on your income. Other Part B costs: There is a $198 annual deductible for Medicare Part B in 2020.
When is the Medicare election period?
The AEP runs from October 15 through December 7 of each year. It is the one enrollment period that occurs each year.
When does Medicare open enrollment end?
Medicare Advantage plan enrollees have an annual opportunity to disenroll from their plan and return to Original Medicare between January 1 and March 31 of every year. The effective date of a disenrollment request made during the Medicare Advantage Open Enrollment Period will be the first ...
When is Medicare disenrollment effective?
The effective date of a disenrollment request made during the Medicare Advantage Open Enrollment Period will be the first of the month following the Medicare Advantage Plan’s receipt of the disenrollment request . A request made in January will be effective February 1, and a request made in February will be effective March 1.
What is AEP enrollment?
It is the one enrollment period that occurs each year. The AEP is also referred to as the “Fall Open Enrollment” season in Medicare beneficiary publications and other tools. Outside of this period, you may be more limited in the types of changes you can make.
Who completes an enrollment request?
You or a legal representative completes an enrollment request and includes all the information required to process the enrollment or meets alternative conditions for enrollment specified by Medicare.
Can you live outside of the service area of Medicare Advantage?
Permanently reside in the service area of the Medicare Advantage plan (exceptions may apply for persons living outside the service area at time of the enrollment request). Not have been medically determined to have End-Stage Renal Disease (ESRD) prior to completing the enrollment request.
Can you change your Medicare Advantage plan?
In addition, you may be able to change your Medicare Advantage coverage by qualifying for a Special Election Period (SEP). This lets you enroll in, switch, or disenroll from plans without waiting for the Annual Election Period or the Medicare Advantage Open Enrollment Period that occurs each year. Some situations that may qualify you for a Special Election Period include, but aren’t limited to, if you: