
Full Answer
What is the rate of Medicaid fraud?
Medicare fraud stats suggest that all parts of the insurance scheme are vulnerable to scams and abuse, with roughly 3–4% of insurance claims being fraudulent. 3. Medicaid has an improper payment rate of 14.90%. Inconsistencies in payments may not necessarily mean fraud or abuse, but do indicate a human error.
How does Medicare fraud affect the entire healthcare system?
Medicare fraud statistics show that billions of dollars are wasted every year due to scams and corruption. The damage to the entire healthcare system is irreparable, as that money could have been invested in a range of legal medical services. Enormous expenses of fraudulent practices result in Medicare costs escalation.
What percentage of healthcare spend is due to fraud?
Fraud and abuse comprise between 3% and 10% of total healthcare spendings. The National Healthcare Anti-Fraud Association estimates that health care scams incur billions of dollars of losses every year, as much as 10% of annual healthcare spendings.
What is the $62 million Medicare fraud case in Miami?
Two Miami residents were convicted and sentenced in February to serve 72 months in prison for their roles in a $62 million Medicare fraud scheme involving mental health treatment programs at the now defunct Health Care Solutions Network that often consisted of nothing more than Disney movies and bingo games.
How much is Medicare fraud per year?
approximately $60 billion annuallyMedicare fraud can be a big business for criminals. Medicare loses approximately $60 billion annually due to fraud, errors, and abuse, though the exact figure is impossible to measure. Medicare is complicated.
Did you catch that in fiscal year 2016 what was the total number of defendants convicted for healthcare fraud related crimes?
658 defendantsIn FY 2016, the Department of Justice (DOJ) opened 975 new criminal health care fraud investigations. Federal prosecutors filed criminal charges in 480 cases involving 802 defendants. A total of 658 defendants were convicted of health care fraud-related crimes during the year.
What percentage of the US spending on healthcare costs is consumed by fraud waste and abuse?
three percentFraud, waste and abuse in our health care system account for three percent of our total health care spending, costing Americans more than $60 billion every year. For every $1 spent on oversight and enforcement to fight fraud, waste and abuse in Medicare, Americans can see up to $17 in return.
What percentage of healthcare funds are lost due to fraud?
3 percentThe National Health Care Anti-fraud Association (NHCAA) conservatively estimates that 3 percent of all health care spending, or $60 billion, is lost to health care fraud.
Why is healthcare fraud so prevalent?
There are many innocent Americans who are being cheated when visiting different medical facilities or when they are getting medications. Their lack of education in understanding different medical information facilitates the occurrence of medical fraud.
Does the government play a role in the increase of fraud and abuse in healthcare?
Recently, the U.S. Department of Justice announced “the largest ever health care fraud enforcement action,” charging 412 people with crimes totaling around $1.3 billion in false billings. Many of the charges were related to the prescription and distribution of opioids, according to the Washington Post.
How much does healthcare fraud cost the US?
Health care fraud costs insurers anywhere between $70 billion and $234 billion each year, harming both patients and taxpayers.
What percentage of US healthcare spending is devoted to unnecessary services?
In other words, just get rid of the waste. A new study, published Monday in JAMA, finds that roughly 20 percent to 25 percent of American health care spending is wasteful.
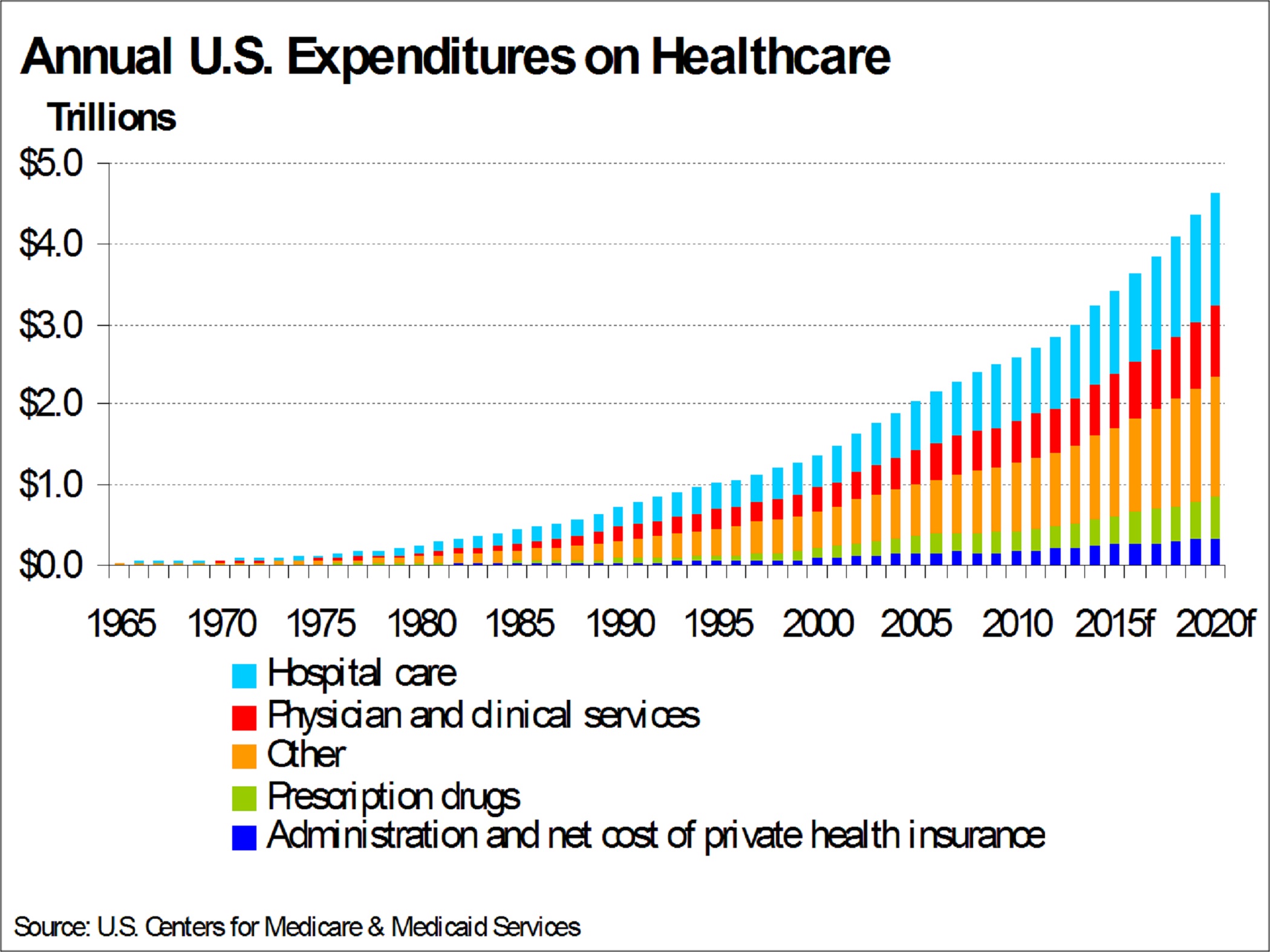
How much of US healthcare spending is wasteful?
Estimates of total waste ranged from $600 billion to almost $2 trillion annually, or 17% to 53% of the $3.6 trillion we now spend annually on healthcare.
How does Medicare fraud affect the economy?
The Effects on Your Organization Fraud perpetrated against the Medicare and Medicaid systems directly drains the taxpayers of this country. Medicare is funded through a payroll tax on both the employer and employee. As more funds are needed, taxes are raised. Thus, everyone employed is affected.
What is the largest area of fraud identified by the insurance industry?
Application Fraud It is generally the most common form of insurance fraud, being responsible for up to two-thirds of all denied life insurance claims alone, according to the Los Angeles Times.
How extensive is healthcare fraud?
The National Health Care Anti-Fraud Association (NHCAA) estimates that the financial losses due to health care fraud are in the tens of billions of dollars each year.
How much money was stolen from Medicare in 2010?
The federal government admits that a staggering $60 billion is stolen from tax payers through Medicare scams every year. Some experts believe the number is more than twice that.
Who is the senator for Medicare fraud?
Sen. Charles Grassley, R-Iowa, who has been holding hearings for decades on Medicare fraud, said he's worried the president's health care bill fails to address the problem at the heart of the matter: pay and chase. Medicare pays the criminals and then chases after them.
Why is Medicare so easy to get?
It's that easy because Medicare is based on trust. When the program was introduced in the 1960s it was assumed that no one would try to defraud a system designed to take care of the health needs of the elderly. The government was required to reimburse vendors in less than 30 days.
How long does it take for Medicare to reimburse a vendor?
The government was required to reimburse vendors in less than 30 days. To this day, in 99.9 percent of the cases, Medicare "auto-adjudicates" claims within 30 days. In other words, the computer decides if the right codes are in the right boxes. If they are, jackpot, the checks are sent.
How much was phony claims made by Teller?
Teller estimates that $50,000 in phony claims was made under her Medicare card. Judge Marshall Ader, who sat on the Florida state bench for decades, said he even had trouble getting Medicare to pay attention.
Who is the attorney for Medicare scam?
U.S. Attorney Jeffrey Sloman spearheads prosecutions in South Florida.
Who can be involved in individual scams?
Former car mechanics and drug dealers, bus boys and clerks can be involved in individual scams, taking tens of millions of dollars every year from the government program designed to provide health care to the nation's elderly.
How much was recovered from healthcare fraud in 2014?
In 2014, the federal government recovered nearly $5.7 billion in healthcare fraud cases, up $1.9 billion from the prior fiscal year. Of that amount, $2.3 billion was tied to healthcare fraud against the federal government, according to a recent review by the Nashville, Tennessee firm of Bass, Berry & Sims PLC.
Who is the doctor who was charged with insurance fraud?
15 announcement. Dr. Munir Uwaydah, 49, owner of Frontline Medical, his personal lawyer and his former office manager are among 15 defendants named in the case that also alleges surgical procedures were performed by a physician's assistant who never attended medical school. Full story.
Why did Community Health Systems pay $75 million?
Community Health Systems and three of its hospitals in New Mexico in February agreed to pay a $75 million settlement to the federal government over a whistleblower suit that claimed it illegally donated money between 2000 and 2011 to New Mexico counties in return for higher Medicaid payments to cover the costs of indigent care. The 2009 suit claimed CHS and three of its New Mexico facilities received higher payments from the New Mexico Sole Community Provider Fund, a matching funds program between the state and Medicaid. The money in the fund was meant to help cover costs for unpaid medical bills.The activity was uncovered by whistleblower Robert Baker, a former revenue manager at Community Health Systems Professional Services Corp. Full story.
What is the owner of a home healthcare company in Illinois facing?
The owner of an Illinois home healthcare company is facing conspiracy and fraud charges after being indicted in an alleged kickback scheme that defrauded Medicare for at least $450,000.
How much did the Justice Department recover from the False Claims Act?
The Justice Department raked in more than $3.5 billion in 2015 in settlements and judgements from civil cases under the False Claims Act, including $1.9 billion in healthcare fraud settlements, according to Principal Deputy Assistant Attorney General Benjamin C. Mizer, head of the Justice Department's Civil Division. Since January 2009, the DOJ has recovered $26.4 billion, with the bulk coming out of healthcare cases. Full story.
What happened to the medical director of Brooklyn Center?
Medical director at Brooklyn center sentenced for $13M fraud - August 17. A doctor at a Brooklyn, New York, clinic was sentenced Friday to two years in prison for his role in a $13 million healthcare fraud scheme, according to the U.S. Department of Justice.
How long is the owner of a pharmacy in prison?
The Miami owner of eight pharmacies will spend nine years in prison, the Department of Justice announced this week, for his part in a healthcare fraud that saw him spending the money he scammed on luxury cars for himself and his family. Full story.
In addition to costing taxpayers billions of dollars, Medicare fraud also lowers the quality of healthcare
Medicare processed more than $909 billion in Medicare benefits in 2020. That's millions of claims, and sifting through that data to find examples of fraud can be a challenge.
What is Medicare fraud?
Medicare fraud is when someone knowingly does something to deceive Medicare in order to receive a payment when they shouldn't be paid, or to get a higher payment than they are supposed to.
How much does Medicare fraud cost the government?
In 2020, CMS estimated that improper payments to Medicare cost billions of dollars each year. While improper payments don't necessarily mean fraud, they are payments that did not meet statutory, regulatory, administrative, or other legally applicable requirements.
How does Medicare fraud impact beneficiaries?
Medicare fraud can impact beneficiaries both physically and financially.
How to help prevent Medicare fraud
One of the best ways to help prevent Medicare fraud is to know what it is and recognize when it happens.
What are the components of Medicare?
Although Medicare’s two components—Hospital Insurance (HI) and Supplementary Medical Insurance (SMI)— are very different from each other in many key respects, it is important to consider the overall cost of Medicare and its financing.
When will the Trust Fund be depleted?
However, the Trustees project slight surpluses in 2015 through 2023, with a return to deficits thereafter until the trust fund becomes depleted in 2030. In 2014, $8.1 billion in trust fund assets were redeemed to cover the shortfall of income relative to expenditures. The Treasury .
How much money does Medicare lose?
Medicare loses billions of dollars each year due to fraud, errors, and abuse. Estimates place these losses at approximately $60 billion annually, though the exact figure is impossible to measure. Medicare fraud hurts us all.
How to protect Medicare benefits?
Be the first line of defense in protecting your Medicare benefits. Treat your Medicare card like a credit card. Your Medicare number can be valuable to thieves who want to steal your medical identity or bill Medicare without even seeing you.
How to find Medicare Patrol?
To locate your state Senior Medicare Patrol (SMP) use the SMP State Locator or call 1-877-808-2468. For a printable resource, see the Medicare Fraud by the Numbers Fact Sheet. Fraud Convictions. Operation Brace Yourself.
What is SMP in Medicare?
SMPs and their trained volunteers help educate and empower Medicare beneficiaries in the fight against health care fraud . Your SMP can help you with your questions, concerns, or complaints about potential fraud and abuse issues. It also can provide information and educational presentations.
How much does health care fraud cost?
The National Heath Care Anti-Fraud Association estimates conservatively that health care fraud costs the nation about $68 billion annually — about 3 percent of the nation's $2.26 trillion in health care spending. Other estimates range as high as 10 percent of annual health care expenditure, or $230 billion.
Is health care fraud a felony in Michigan?
Health care fraud is a felony under Michigan's Health Care False Claims Act, punishable by up to four years in prison, a $50,000 fine and loss of health insurance. It's also a federal criminal offense under the Health Insurance Portability and Accountability Act.
What is Medicare Part D improper payment estimate?
The Medicare Part D improper payment estimate measures the payment error related to inaccurately submitted prescription drug event (PDE) data, where the majority of errors for the program exists . CMS measures the inconsistencies between the information reported on PDEs and the supporting documentation submitted by Part D sponsors including prescription record hardcopies (or medication orders, as appropriate), and detailed claims information. The FY 20202020 Part D improper payment data is representative of PDE data generated from the Calendar Year 2018 payment year.
What is a smaller proportion of improper payments?
A smaller proportion of improper payments are payments that should not have been made or should have been made in different amounts and are considered a monetary loss to the government (e.g., medical necessity, incorrect coding, beneficiary ineligible for program or service, and other errors).
Is the APTC program reporting improper payments?
While a FY 2016 risk assessment concluded that the Advance Payments of the Premium Tax Credit (APTC) program is susceptible to significant improper payments, the program is not yet reporting improper payment estimates for FY 2020. CMS is committed to implementing an improper payment measurement program as required by PIIA. As with similar CMS programs, developing an effective and efficient improper payment measurement program requires multiple, time-intensive steps including contractor procurement; developing measurement policies, procedures, and tools; and extensive pilot testing to ensure an accurate improper payment estimate. CMS will continue to monitor and assess the program for changes and adapt accordingly. In FYs 2017 through 2020, CMS conducted development and piloting activities for the APTC improper payment measurement program and will continue these activities in FY 2021. HHS will continue to update its annual AFRs with the measurement program development status until the reporting of the improper payment estimate.
