Uninsured Care Expansion Grant The Health Care Authority (HCA) has received $35 million in federal resources for the provision of health care services for uninsured and underinsured individuals under 200 percent of the federal poverty level, regardless of immigration status.
Full Answer
What is the ACA Medicaid expansion?
Uninsured Care Expansion Grant. The Health Care Authority (HCA) has received $35 million in federal resources for the provision of health care services for uninsured and underinsured individuals under 200 percent of the federal poverty level, regardless of immigration status. HCA will distribute funding in the form of Uninsured Care Expansion Grants.
What would happen if the Affordable Care Act didn’t expand Medicaid?
Feb 07, 2022 · Its focus is on expanding its roster of physicians as well as outpatient network. HCA Healthcare maximized profits at the expense of patient care and obtained more than $1 billion in fraudulent...
Is HCA Healthcare’s systemic over-admissions of Medicare patients need reform?
The ACA Medicaid Expansion in Washington Full implementation of the Affordable Care Act (ACA) will add some 330,000 people to the Medicaid rolls in Washington state and a much smaller number for the Children's Health Insurance Program (CHIP). The state’s cost per new enrollee will be low, however, when compared with current enrollees.
How many hospitals did HCA Healthcare have in 1981?
Dec 03, 2014 · December 3, 2014. The Health Care Authority (HCA) has completed changes that should help many hospitals obtain significant additional Medicare disproportionate share hospital funding. WSHA became aware that HCA’s process for counting and reporting Medicaid days for the period from January 1, 2011 through December 2013 did not include days for patients …

Did the ACA expand Medicare?
The Affordable Care Act's (ACA) Medicaid expansion expanded Medicaid coverage to nearly all adults with incomes up to 138% of the Federal Poverty Level ($17,774 for an individual in 2021) and provided states with an enhanced federal matching rate (FMAP) for their expansion populations.Feb 24, 2022
What is the Medicare expansion?
Medicare expansion refers to broadening the benefits of the program, as the parts in which beneficiaries enroll through the government provide limited coverage. Throughout the years, extensions of the program have been uncommon, with one of the most notable instances being coverage of disabled individuals under 65.Nov 9, 2021
What was the purpose of the expansion under the Affordable Care Act?
A provision in the Affordable Care Act (ACA) called for the expansion of Medicaid eligibility in order to cover more low-income Americans. Under the expansion, Medicaid eligibility would be extended to adults up to age 64 with incomes up to 138% of the federal poverty level (133% plus a 5% income disregard).
Did Pa expand Medicare?
Pennsylvania expanded Medicaid as of January 1, 2015, a year after it first became available under the ACA. Eligible enrollees were able to apply starting December 1, 2014.
Who is Medicare through?
The Centers for Medicare & Medicaid Services (CMS) is the federal agency that runs Medicare. The program is funded in part by Social Security and Medicare taxes you pay on your income, in part through premiums that people with Medicare pay, and in part by the federal budget.
Who qualifies for Mainecare expansion?
Who is eligible for Expansion? People age 21 to 64, who are not eligible for Medicare, with income less than the limit shown for their family size in this chart are eligible. There are no asset limits.Jan 20, 2022
Did the ACA Medicaid expansion save lives?
We estimate the effect of the Affordable Care Act Medicaid expansion on county-level mortality in the first four years following expansion. We find a reduction in all-cause mortality in ages 20 to 64 equaling 11.36 deaths per 100,000 individuals, a 3.6 percent decrease.
How did the Affordable Care Act change healthcare?
The ACA significantly changed the healthcare system in the U.S. by reducing the amount individuals and families paid in uncompensated care. The act requires every American to have health insurance and provides assistance to those who cannot afford a plan.
Is Medicare Part of the Affordable Care Act?
The 2010 Affordable Care Act (ACA) included many provisions affecting the Medicare program and the 57 million seniors and people with disabilities who rely on Medicare for their health insurance coverage.Dec 13, 2016
What are the 2021 Medicare changes?
The Medicare Part B premium is $148.50 per month in 2021, an increase of $3.90 since 2020. The Part B deductible also increased by $5 to $203 in 2021. Medicare Advantage premiums are expected to drop by 11% this year, while beneficiaries now have access to more plan choices than in previous years.Sep 24, 2021
Did Oklahoma expand Medicaid?
Oklahoma has successfully expanded Medicaid, as more than 210,000 Oklahomans have enrolled in expansion and there have been substantial declines in the uninsured rate across all demographics.Nov 15, 2021
Did Wisconsin expand Medicaid?
But because Wisconsin has not expanded Medicaid, the state is only receiving its regular federal match rate of 59.36%, and the state is paying the rest (the federal matching rate has been temporarily increased by federal legislation, in order to address the COVID-19 pandemic; Wisconsin's federal Medicaid funding has ...Dec 29, 2021
How much did Columbia HCA pay?
Over two settlement rounds, Columbia/HCA wound up paying the government $1.7 billion in criminal fines, civil damages, and penalties, in what the Justice Department called “the largest health-care fraud case in U.S. history.
Who is the Republican senator who is leading the push for health care reform?
On Thursday, Trump told reporters that Scott, and fellow Republican Senators John Barrasso of Wyoming and Bill Cassidy of Louisiana, will lead the party’s push on health-care reform.
What is the Affordable Care Act?
Medicaid—a federal/state partnership with shared authority and financing—is a health insurance program for low-income individuals, children, their parents, the elderly and people with disabilities. Medicaid pays for health care for more than 74.5 million people nationally.
Do all states have to meet the federal minimum requirements for Medicaid?
However, eligibility for Medicaid benefits varies widely among the states - all states must meet federal minimum requirements, but they have options for expanding Medicaid beyond the minimum federal guidelines, the details are outlined here.
Why didn't I qualify for medicaid?
Weren’t eligible for Medicaid when you first applied because you live in a state that hasn’t expanded Medicaid. Weren’t eligible for a Marketplace plan with tax credits when you first applied because your income was too low.
What is the poverty level for Medicaid?
When the health care law was passed, it required states to provide Medicaid coverage for all adults 18 to 65 with incomes up to 133% (effectively 138%) of the federal poverty level, regardless of their age, family status, or health. The law also provides premium tax credits for people with incomes between 100% and 400% of ...
What percentage of income is eligible for Marketplace Plan?
If your expected yearly income increases so it’s between 100% and 400% of the federal poverty level (FPL), you become eligible for a Marketplace plan with advance payments of the premium tax credit (APTC). If your income increases to above 400% FPL, you may still qualify for savings.
Can I apply for medicaid if my state hasn't expanded?
Even if your state hasn't expanded Medicaid and it looks like your income is below the level to qualify for financial help with a Marketplace plan, you should fill out a Marketplace application.
Is Medicaid expansion voluntary?
The U.S. Supreme Court later ruled that the Medicaid expansion is voluntary with states. As a result, some states haven’t expanded their Medicaid programs. Adults in those states with incomes below 100% of the federal poverty level, and who don’t qualify for Medicaid based on disability, age, or other factors, fall into a gap.
Can I qualify for medicaid if I have expanded my Medicaid?
Others haven’t. Whether you qualify for Medicaid coverage depends partly on whether your state has expanded its program. In all states: You can qualify for Medicaid based on income, household size, disability, family status, and other factors. Eligibility rules differ between states. In states that have expanded Medicaid coverage: You can qualify ...
Do you have to pay for low cost medical care?
See how to get low-cost care in your community. If you don’t have any coverage, you don’t have to pay the fee. For plan years through 2018, most people must have health coverage or pay a fee. But you won’t have to pay this fee if you live in a state that hasn’t expanded Medicaid and you would have qualified if it had.
What is the ACA expansion?
A provision in the Affordable Care Act ( ACA) called for expansion of Medicaid eligibility in order to cover more low-income Americans. Under the expansion, Medicaid eligibility would be extended to adults up to age 64 with incomes up to 138 percent of the federal poverty level (133 percent plus a 5 percent income disregard).
Which states have Medicaid expansion?
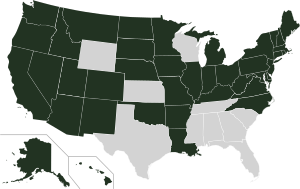
Five states — Texas, North Carolina, Florida, Georgia, and Tennessee — account for the lion’s share of the coverage gap population, and they are among the 14 states where expansion is still a contentious issue and the legislature and/or governor are still strongly opposed to accepting federal funding to expand Medicaid.
How many people are on medicaid in 2019?
As of 2019, official Medicaid data put the total newly-eligible enrollment at about 10 million . Total enrollment in Medicaid/CHIP has increased by 26 percent since 2013, although enrollment growth is much higher than that average (34.4 percent) if we only consider states that have expanded Medicaid.
How many states have expanded Medicaid?
Thirty-six states and DC have either already expanded Medicaid under the ACA or are in the process of doing so. Fourteen states continue to refuse to adopt Medicaid expansion, despite the fact that the federal government will always pay 90% of the cost.
Is Medicaid funded by the federal government?
The federal government is financing most of the cost of expanding Medicaid, and a small portion is being paid by participating states. The costs for enrollees who are newly eligible under the expanded guidelines was covered 100 percent by the federal government until 2016.
When did HCA Healthcare merge with Columbia?
HCA Healthcare re-emerged as a public company in 1992. In February 1994 , HCA Healthcare merged with Louisville, Kentucky-based Columbia Hospital Corporation, which earlier had acquired 73 hospitals of Galen Health Care from Humana, to form Columbia/HCA.
What happened to HCA?
In 1993, lawsuits were filed against HCA by former employees who alleged that the company had engaged in questionable Medicare billing practices. In 1997, with a federal investigation by the FBI, the IRS and the Department of Health and Human Services in its early stages, the Columbia/HCA board of directors forced Rick Scott to resign as chairman and CEO amid growing evidence that the company "had kept two sets of books, one to show the government and one with actual expenses listed." Thomas Frist, a co-founder of HCA and brother of U.S. Senator Bill Frist, returned to the company as CEO in 1997 and called on longtime friend and colleague Jack O. Bovender, Jr. to help him turn the company around.
Why did Bill Frist sell his HCA stock?
In July 2005, U.S. Senator Bill Frist sold all of his HCA shares, which were held in a blind trust, two weeks before disappointing earnings sent the stock on a 9-point plunge. At the time, Frist was considering a run for president and said that he had sold his shares to avoid the appearance of a conflict of interest. When the company disclosed that other executives had also sold their shares during that same time, shareholders alleged that the company had made false claims about its profits to drive up the price, which then fell when the company reported disappointing financial results. Eleven of HCA's senior officers were sued for accounting fraud and insider trading. HCA settled the lawsuit in August 2007, agreeing to pay $20 million to the shareholders but admitting no wrongdoing, and no charges were brought.
What was the HCA industry in the 1970s?
The 1970s were characterized by rapid growth in the industry and for HCA Healthcare. In the early 1980s, the focus shifted to consolidation with HCA Healthcare acqui ring General Care Corporation, General Health Services, Hospital Affiliates International and Health Care Corporation. By the end of 1981, the company operated 349 hospitals with more than 49,000 beds. Operating revenues had grown to $2.4 billion.
What does HCA Healthcare do?
HCA Healthcare supports local communities through the HCA Healthcare Foundation and HCA Healthcare corporate sponsorships, as well as through the grassroots efforts of employees and affiliates. The company provides support for childhood and youth development programs, scholarships, community-based health clinics and the operating budgets of not-for-profit organizations. HCA Healthcare provided $45 million in charitable contributions across the United States in 2019.
How many babies does HCA deliver?
HCA Healthcare delivers nearly one of every 17 babies born in the United States, more than 219,000 in 2019. Maternal mortality at HCA Healthcare hospitals was less than half the national rate in 2019. March of Dimes is a national partner of HCA Healthcare.
How many stroke patients does HCA treat?
HCA Healthcare treats approximately 50,000 stroke patients annually at 31 recognized comprehensive stroke centers. The average time between a patient's arrival and receiving needed medication as of November 2019 was 42 minutes—30% faster than the national standard.
What is HCA in medical terms?
HCA is “cherry-picking patients, ” said Ed Jimenez, CEO of the University of Florida Health Shands, which runs a Level I trauma center, the highest designation. “What you find is an elderly person who fell and broke their hip who could be perfectly well treated at their local hospital now becomes a trauma patient.”.
How many trauma centers does HCA have?
HCA has opened trauma centers in more than half its 179 hospitals and says it runs 1 of every 20 such facilities in the country. And it’s not slowing down. What Trauma Center Levels Mean.
How much does VCU charge for trauma activation?
VCU Health charges up to $13,455 for trauma activation, according to its charge list.
Is VCU covered by Medicaid?
VCU and other urban hospitals, on the other hand, treat a higher share of patients with gun and knife injuries — penetra ting trauma — who are more often uninsured or covered by Medicaid. About 75% of VCU’s trauma cases are classified as blunt trauma, hospital officials said.
Is Med Trans part of Aetna?
But Med-Trans is out of network for Virginia members of Aetna and UnitedHealthcare, two of the state’s biggest carriers, said spokespeople for those companies. Med-Trans is part of Anthem Blue Cross Blue Shield’s network, an Anthem spokesperson said.
Is HCA reimbursed by insurers?
HCA and its contractor had filed paperwork for the operation to be reimbursed by insurers when Richmond City Council members learned about it. Members “were not up to speed on this matter,” council member Kristen Larson told a May 2020 meeting of the Richmond Ambulance Authority, according to the minutes.