Pre-existing conditions are the main reason you could be denied a Medicare Supplement
Medigap
Medigap refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges. Medigap's name is derived from the notion that it exists to …
What to do if Medicare denies your medical claim?
Feb 12, 2022 · You have a guaranteed issue right: If you have a guaranteed issue right, such as if you move out of the service area for your Medicare Advantage plan, insurance companies cant refuse your application for a Medigap policy or charge you more for one. And they must cover your preexisting health conditions.
Are people denied Medicare and why?
Apr 13, 2021 · Consequently, denied Medicare claims could be one of those unwelcome surprises that can sometimes be returned or attributed to a learning experience on your part. First, let us know some of the reasons why your claims were denied: The doctor or the hospital you visited is not in Medicare's network; The care you sought was not deemed "necessary."
What can you do if your Medicaid application is denied?
Oct 26, 2021 · In most cases your renewal is considered guaranteed and cannot be dropped, however there are certain circumstances when the insurance company can decide not to renew your Medigap policy: You stopped making premium payments. You lied on your policy application. Your insurance company went bankrupt.
Can secondary insurance pay claims that are denied by Medicare?
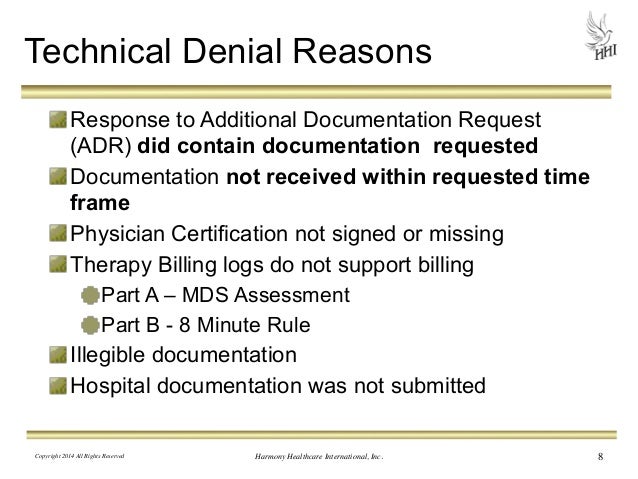
Jun 25, 2014 · The following are ten reasons for denials and rejections: 1. The claim was submitted to the wrong contractor or payer, an error which is frequently associated with new Medicare advantage programs. For instance, a claim was sent to Traditional Medicare when it should have been sent to Railroad Medicare. 2. The patient ID is not valid. 3.

Why did I get denied for Medicare?
Medicare's reasons for denial can include: Medicare does not deem the service medically necessary. A person has a Medicare Advantage plan, and they used a healthcare provider outside of the plan network. The Medicare Part D prescription drug plan's formulary does not include the medication.Aug 20, 2020
What would make you ineligible for Medicare?
Did not work in employment covered by Social Security/Medicare. Do not have 40 quarters in Social Security/Medicare-covered employment. Do not qualify through the work history of a current, former, or deceased spouse.
Can Medicare coverage be denied?
When Can a Medicare Plan Deny Coverage? Coverage can be denied under a Medicare Advantage plan when: Plan rules are not followed, like failing to seek prior approval for a particular treatment if required. Treatments provided were not deemed to be medically necessary.Aug 12, 2020
What is Medicare Part B only?
Medicare Part B helps cover medical services like doctors' services, outpatient care, and other medical services that Part A doesn't cover. Part B is optional. Part B helps pay for covered medical services and items when they are medically necessary.Sep 16, 2014
Who is eligible for Medicare Part B reimbursement?
How do I know if I am eligible for Part B reimbursement? You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B. 2.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
Can Medicare Advantage plans deny for pre-existing conditions?
As with Original Medicare, Medicare Advantage plans can't charge you more for preexisting conditions. Because they are offered by private insurance companies, basic costs for Medicare Advantage plans will vary by plan. In addition, you can't be denied coverage based on preexisting conditions.
What states are guaranteed issue for Medicare Supplement?
Only four states (CT, MA, ME, NY) require either continuous or annual guaranteed issue protections for Medigap for all beneficiaries in traditional Medicare ages 65 and older, regardless of medical history (Figure 1).Jul 11, 2018
Why is Medicare denied?
The following are ten reasons for denials and rejections:#N#1. The claim was submitted to the wrong contractor or payer, an error which is frequently associated with new Medicare advantage programs. For instance, a claim was sent to Traditional Medicare when it should have been sent to Railroad Medicare.#N#2. The patient ID is not valid.#N#3. There is another insurance primary.#N#4. The patient name or date of birth does not match the Medicare beneficiary or Medicare record.#N#5. The primary payer’s coordination of benefits is not in balance.#N#6. There is only Part A coverage and no Part B coverage.#N#7. The referring physician’s NPI is invalid.#N#8. The zip code of where the service was rendered is invalid.#N#9. The Procedure Code for the date of service is invalid.#N#10. Simple user error, such as a mistake in the info submitted other than date of birth or name.
What is revenue cycle denial management?
Some use the term to describe a method of addressing claims that have been denied for a medical procedure or treatment. Others have used the term to describe how some information is tracked for a particular payer, place of service, or set of procedures. Still, there are some that try and use the term to describe what they do every day in a physician’s office.
What happens if Medicare denies coverage?
If you feel that Medicare made an error in denying coverage, you have the right to appeal the decision. Examples of when you might wish to appeal include a denied claim for a service, prescription drug, test, or procedure that you believe was medically necessary.
What are some examples of Medicare denied services?
This notice is given when Medicare has denied services under Part B. Examples of possible denied services and items include some types of therapy, medical supplies, and laboratory tests that are not deemed medically necessary.
What is a denial letter for Medicare?
Medicare denial letters notify you of services that won’t be covered for a variety of reasons. There are several different types of letters, depending on the reason for denial. Denial letters should include information about how to appeal the decision. You will receive a Medicare denial letter when Medicare denies coverage for a service or item ...
When do you get a notice of non-coverage from Medicare?
You’ll receive a Notice of Medicare Non-Coverage if Medicare stops covering care that you get from an outpatient rehabilitation facility, home health agency, or skilled nursing facility. Sometimes, Medicare may notify a medical provider who then contacts you. You must be notified at least 2 calendar days before services end.
What is an integrated denial notice?
Notice of Denial of Medical Coverage (Integrated Denial Notice) This notice is for Medicare Advantage and Medicaid beneficiaries, which is why it’s called an Integrated Denial Notice. It may deny coverage in whole or in part or notify you that Medicare is discontinuing or reducing a previously authorized treatment course. Tip.
What is a denial letter?
A denial letter will usually include information on how to appeal a decision. Appealing the decision as quickly as possible and with as many supporting details as possible can help overturn the decision.
Does Medicare cover skilled nursing?
This letter will notify you about an upcoming service or item at a skilled nursing facility that Medicare will not cover. In this case, Medicare has deemed the service not medically reasonable and necessary. The service might also be deemed custodial (not medical related), which is not covered.
