
Since 2019, Medicare Advantage plans have been allowed to cover a broader range of extra benefits, including things like home health aides, medical transportation, and the installation of in-home safety devices. Relatively few plans have started offering these benefits as of 2021, but more appear poised to do so for 2022.
Full Answer
What are the benefits of Medicare Advantage plans?
- Eye exams and/or eyeglasses: Provided by 98% of plans
- Fitness benefit: 97%
- Telehealth: 95%
- Hearing exams and/or hearing aids: 95%
- Dental benefit: 94%
- Prescription drug coverage: 89%
- Over-the-counter benefits (for items such as adhesive or elastic bandages): 81%
- Meal benefit (such as a cooking class, nutrition education or meal delivery): 67%
How many Medicare Advantage plans are there?
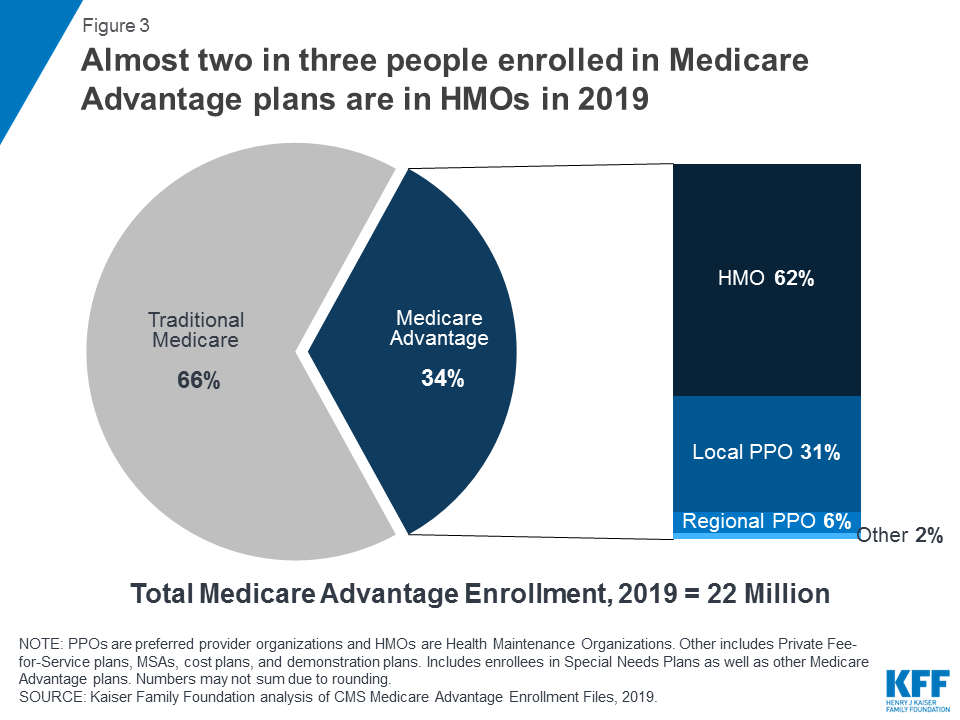
Your care is “coordinated” in four types of Medicare Advantage plans: HMO, POS, PPO, and SNP. This means that the plan can coordinate your coverage with a primary care doctor who manages the care you receive from specialists and hospitals. You may need to select specific doctors and hospitals.
What is the best Medicare plan for You?
Ranking the best medicare supplement plans of 2021
- Humana. Humana is one of the largest providers of healthcare and healthcare insurance in the country. ...
- Mutual of Omaha Medicare Supplement. Mutual of Omaha offers eight Medicare supplement plans that cover most out of pocket expenses most people will incur.
- United Medicare Advisors. ...
- Aetna Medicare Supplement. ...
- Cigna. ...
Which Medicare Advantage plans are available in my area?
Wyoming
- SHIP Contact the State Health Information Program if you are trying to make a health care plan decision and need unbiased advice. ...
- U.S. ...
- Wyoming Health Insurance Consumer Help The organizations listed on this page can help you make the most of your Medicare options. ...
What is not covered by Medicare Advantage plans?
Most Medicare Advantage Plans offer coverage for things Original Medicare doesn't cover, like fitness programs (like gym memberships or discounts) and some vision, hearing, and dental services. Plans can also choose to cover even more benefits.
What is included in a Medicare Advantage plan?
Medicare Advantage Plans must offer emergency coverage outside of the plan's service area (but not outside the U.S.). Many Medicare Advantage Plans also offer extra benefits such as dental care, eyeglasses, or wellness programs. Most Medicare Advantage Plans include Medicare prescription drug coverage (Part D).
Does Medicare Advantage pay 80%?
Under Medicare Part B, patients usually pay 20% of their medical bills and Medicare pays the remaining 80%. Medicare Advantage, however, can charge patients coinsurance rates above 20%.
Do Medicare Advantage plans pay 100 %?
Medicare Advantage plans must limit how much their members pay out-of-pocket for covered Medicare expenses. Medicare set the maximum but some plans voluntarily establish lower limits. After reaching the limit, Medicare Advantage plans pay 100% of eligible expenses.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Do Medicare Advantage Plans cover hospital stays?
Medicare Advantage plans typically cover hospital and medical benefits, as well as prescription drugs not generally covered by Original Medicare (Part A and Part B).
How do you qualify for $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
What is the most popular Medicare Advantage plan?
AARP/UnitedHealthcare is the most popular Medicare Advantage provider with many enrollees valuing its combination of good ratings, affordable premiums and add-on benefits. For many people, AARP/UnitedHealthcare Medicare Advantage plans fall into the sweet spot for having good benefits at an affordable price.
What are the top 3 Medicare Advantage plans?
Best Medicare Advantage Providers RatingsProviderForbes Health RatingsCMS ratingHumana5.03.6Blue Cross Blue Shield5.03.8Cigna4.53.8United Healthcare4.03.81 more row•Feb 25, 2022
What percent of seniors choose Medicare Advantage?
[+] More than 28.5 million patients are now enrolled in Medicare Advantage plans, according to new federal data. That's up nearly 9% compared with the same time last year. More than 40% of the more than 63 million people enrolled in Medicare are now in an MA plan.
What is the maximum out-of-pocket with Medicare?
Out-of-pocket limit. In 2021, the Medicare Advantage out-of-pocket limit is set at $7,550. This means plans can set limits below this amount but cannot ask you to pay more than that out of pocket.
Does Medicare Advantage have out-of-pocket maximum?
The US government sets the standard Medicare Advantage maximum out-of-pocket limit every year. In 2019, this amount is $6,700, which is a common MOOP limit. However, you should note that some insurance companies use lower MOOP limits, while some plans may have higher limits.
What happens if you have a Medicare Advantage Plan?
If you have a Medicare Advantage Plan, you have the right to an organization determination to see if a service, drug, or supply is covered. Contact your plan to get one and follow the instructions to file a timely appeal. You also may get plan directed care.
How much is Medicare Advantage 2021?
In addition to your Part B premium, you usually pay a monthly premium for the Medicare Advantage Plan. In 2021, the standard Part B premium amount is $148.50 (or higher depending on your income). If you need a service that the plan says isn't medically necessary, you may have to pay all the costs of the service.
What is Medicare Advantage?
Most Medicare Advantage Plans offer coverage for things that aren't covered by Original Medicare, like vision, hearing, dental, and wellness programs (like gym memberships). Plans can also cover more extra benefits than they have in the past, including services like transportation to doctor visits, over-the-counter drugs, adult day-care services, ...
What is Medicare health care?
Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine. under Medicare. If you're not sure whether a service is covered, check with your provider before you get the service.
Is Medicare Advantage covered for emergency care?
In all types of Medicare Advantage Plans, you're always covered for emergency and. Care that you get outside of your Medicare health plan's service area for a sudden illness or injury that needs medical care right away but isn’t life threatening.
Does Medicare cover hospice?
Medicare Advantage Plans must cover all of the services that Original Medicare covers. However, if you’re in a Medicare Advantage Plan, Original Medicare will still cover the cost for hospice care, some new Medicare benefits, and some costs for clinical research studies. In all types of Medicare Advantage Plans, you're always covered for emergency and Urgently needed care.
What is Medicare Advantage?
For those unfamiliar with the Medicare Part C (Medicare Advantage) program, Medicare Advantage plans are health plans offered by Medicare-approved private insurance companies as an alternate way to get your Original Medicare benefits. Medicare Advantage plans must offer at least the same level of coverage as the federal program, but can also provide additional benefits that go beyond Part A and Part B, such as wellness programs. These extra benefits may vary from plan to plan.
Is Medicare Advantage supplemental?
Recently, CMS released a new policy update affecting benefits for Medicare Advantage plans in the 2019 plan year. This new policy expands the definition of Medicare Advantage supplemental benefits to those that aren’t covered by Original Medicare, and:
Who sells Medicare Advantage plans?
Medicare Advantage plans are sold by private insurance companies all over the U.S. As a consumer, you can do some research into a company’s history, reputation and ratings before committing to 2019 coverage.
How many stars does Medicare Advantage have?
Each year, the Centers for Medicare & Medicaid Services (CMS) issues star ratings for all Medicare Advantage plans using a system of one to five stars. 1 These plans are evaluated and rated each year, so plan Star Ratings can change each year.
Does Medicare Advantage have a deductible?
Some Medicare Advantage plans may have a higher monthly premium but a lower deductible (or no deductible at all), while other plans may feature $0 premiums but a higher deductible. $0 premium plans may not be available in all locations.
Why do you keep your Medicare card?
Keep your red, white, and blue Medicare card in a safe place because you’ll need it if you ever switch back to Original Medicare. Below are the most common types of Medicare Advantage Plans. An HMO Plan that may allow you to get some services out-of-network for a higher cost.
What is MSA plan?
Medicare Medical Savings Account (Msa) Plan. MSA Plans combine a high deductible Medicare Advantage Plan and a bank account. The plan deposits money from Medicare into the account. You can use the money in this account to pay for your health care costs, but only Medicare-covered expenses count toward your deductible.
What is a special needs plan?
Special Needs Plans (SNPs) Other less common types of Medicare Advantage Plans that may be available include. Hmo Point Of Service (Hmopos) Plans. An HMO Plan that may allow you to get some services out-of-network for a higher cost. and a. Medicare Medical Savings Account (Msa) Plan.
Does Medicare Advantage include drug coverage?
Most Medicare Advantage Plans include drug coverage (Part D). In many cases , you’ll need to use health care providers who participate in the plan’s network and service area for the lowest costs.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
What to know about Medicare Advantage?
Things to know about Medicare Advantage Plans. You're still in the Medicare Program. You still have Medicare rights and protections. You still get complete Part A and Part B coverage through the plan. Some plans offer extra benefits that Original Medicare doesn ’t cover – like vision, hearing, or dental. Your out-of-pocket costs may be lower in ...
Can you check with a health insurance plan before you get a service?
You can check with the plan before you get a service to find out if it's covered and what your costs may be. Following plan rules, like getting a Referral to see a specialist in the plan's Network can keep your costs lower. Check with the plan.
Can you pay more for a Medicare Advantage plan than Original Medicare?
Medicare Advantage Plans can't charge more than Original Medicare for certain services like chemotherapy, dialysis, and skilled nursing facility care. Medicare Advantage Plans have a yearly limit on your out-of-pocket costs for medical services. Once you reach this limit, you’ll pay nothing for covered services.
What does Medicare Advantage cover?
Advantage plans also cover urgent and emergency care services, and in many cases, the private plans cover vision, hearing, health and wellness programs, and dental coverage. Since 2019, Medicare Advantage plans have been allowed to cover a broader range of extra benefits, including things like home health aides, medical transportation, ...
How many people will be enrolled in Medicare Advantage in 2021?
As of 2021, there were more than 26 million Americans enrolled in Medicare Advantage plans — about 42% of all Medicare beneficiaries. Enrollment in Medicare Advantage has been steadily growing since 2004, when only about 13% of Medicare beneficiaries were enrolled in Advantage plans.
What happens if a Medicare Advantage plan fails to meet the MLR requirements?
If a Medicare Advantage plan fails to meet the MLR requirement for three consecutive years, CMS will not allow that plan to continue to enroll new members. And if a plan fails to meet the MLR requirements for five consecutive years, the Medicare Advantage contract will be terminated altogether.
How much of Medicare revenue is used for patient care?
That means 85% of their revenue must be used for patient care and quality improvements, and their administrative costs, including profits and salaries, can’t exceed 15% of their revenue (revenue for Medicare Advantage plans comes from the federal government and from enrollee premiums).
When did Medicare start?
Managed care programs administered by private health insurers have been available to Medicare beneficiaries since the 1970s, but these programs have grown significantly since the Balanced Budget Act – signed into law by President Bill Clinton in 1997 – created the Medicare+Choice program.
How much of Medicare premiums must be spent on medical?
Medicare Advantage plans must spend at least 85% of premiums on medical costs. The ACA added new medical loss ratio requirements for commercial insurers offering plans in the individual, small group, and large group markets.
What is the average Medicare premium for 2021?
But across all Medicare Advantage plans, the average premium is about $21/month for 2021. This average includes zero-premium plans and Medicare Advantage plans that don’t include Part D coverage — if we only look at plans that do have premiums and that do include Part D coverage, the average premium is higher.
