What do you pay in a Medicare Advantage plan?
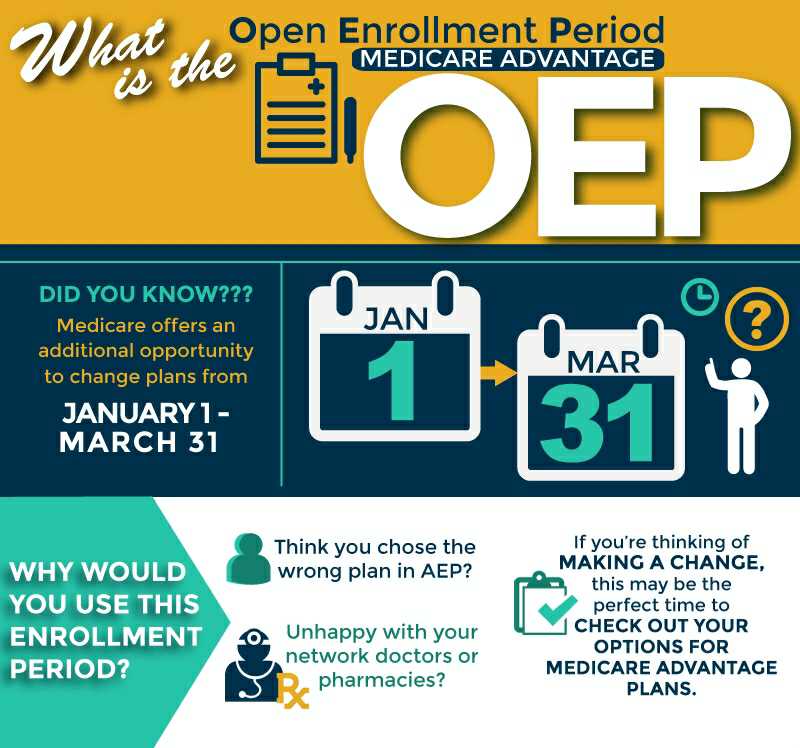
- Complete a new Medicare enrollment (unless you are in your initial or special enrollment period)
- Switch from Original Medicare to Medicare Advantage
- Enroll in a stand-alone Part D prescription drug plan (unless you are moving to Original Medicare from Medicare Advantage)
How much does Medicare Advantage plan cost?
- $1,484 ($1,556 in 2022) deductible for each benefit period
- Days 1-60: $0 coinsurance for each benefit period
- Days 61-90: $371 ($389 in 2022) coinsurance per day of each benefit period
- Days 91 and beyond: $742 ($778 for 2022) coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime)
How to compare Medicare Advantage plans?
What You Should Know
- In 2022, there are more than 3,800 Medicare Advantage Plans for Americans to choose from — more than any previous year.
- Choosing the right plan requires a careful comparison of costs and how often you expect to need the benefits.
- All Medicare Advantage Plans are required to have an annual limit on out-of-pocket costs. ...
Do I qualify for Medicare Advantage?
You need to be enrolled in both Medicare Part A and Part B to qualify for a Medicare Advantage plan. You must also live within the plan’s service area. With any kind of Medicare Advantage plan, in most cases you must continue paying your Medicare Part B premium. However, the Medicaid program might pay your premium.
What is another name for a Medicare Advantage program?
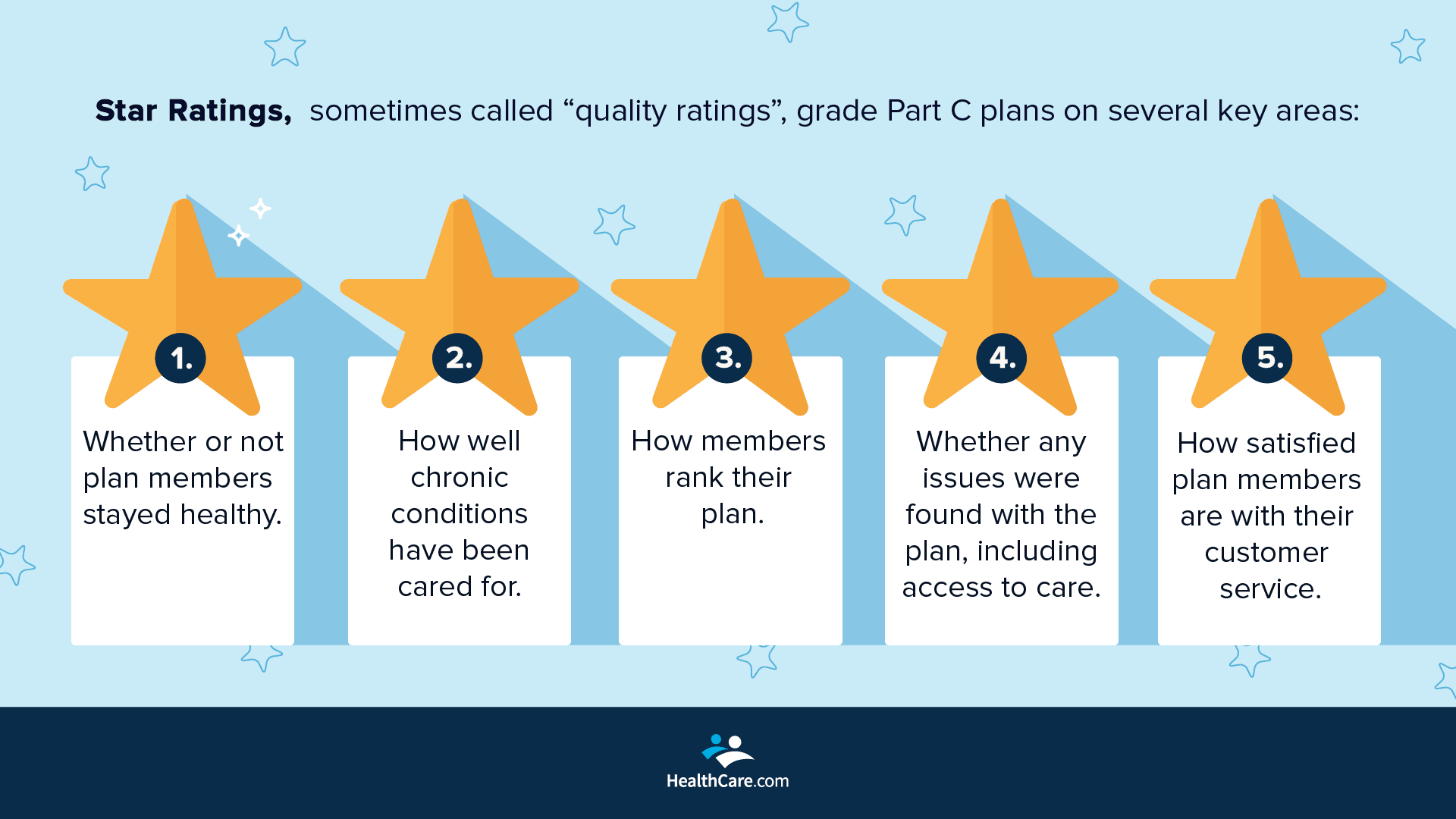
Medicare Advantage Plans, sometimes called “Part C” or “MA Plans,” are offered by private companies approved by Medicare.
Is Medicare Advantage Plan also called Part C?
A Medicare Advantage is another way to get your Medicare Part A and Part B coverage. Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are offered by Medicare-approved private companies that must follow rules set by Medicare.
What are 4 types of Medicare Advantage plans?
HMO Point-of-Service (HMOPOS) Most Medicare beneficiaries who get an Advantage plan enroll in one of two types: HMO (health maintenance organization) plans. PPO (preferred provider organization) plans.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
What is Type C Medicare?
Medicare Advantage, or Medicare Part C, is a type of Medicare plan that uses private health insurance to cover all the services you'd receive under Medicare Parts A and B. Anyone who is eligible for original Medicare Parts A and B is eligible for the Medicare Advantage programs in their area.
Does Medicare Part C replace A and B?
Part C (Medicare Advantage) Under Medicare Part C, you are covered for all Medicare parts A and B services. Most Medicare Advantage plans also cover you for prescription drugs, dental, vision, hearing services, and more.
Is Medicare PPO the same as Medicare Advantage?
There are differences between Medicare Advantage plans. The specific structure of the plan you choose dictates how much you pay for care and where you can seek treatment. HMO plans limit you to a specific network of providers, while PPO plans offer lower rates to beneficiaries who seek care from a preferred provider.
What is the most popular Medicare Advantage plan?
AARP/UnitedHealthcare is the most popular Medicare Advantage provider with many enrollees valuing its combination of good ratings, affordable premiums and add-on benefits. For many people, AARP/UnitedHealthcare Medicare Advantage plans fall into the sweet spot for having good benefits at an affordable price.
What is Medicare plan G?
Plan G is a supplemental Medigap health insurance plan that is available to individuals who are disabled or over the age of 65 and currently enrolled in both Part A and Part B of Medicare. Plan G is one of the most comprehensive Medicare supplement plans that are available to purchase.
Can you switch back to Medicare from Medicare Advantage?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
Who is the largest Medicare Advantage provider?
UnitedHealthcareUnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.
What are the top 3 Medicare Advantage plans?
Best Medicare Advantage Providers RatingsProviderForbes Health RatingsCMS ratingHumana5.03.6Blue Cross Blue Shield5.03.8Cigna4.53.8United Healthcare4.03.81 more row•Feb 25, 2022
What is Medicare Advantage?
A Medicare Advantage is another way to get your Medicare Part A and Part B coverage. Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are offered by Medicare-approved private companies that must follow rules set by Medicare. If you join a Medicare Advantage Plan, you'll still have Medicare but you'll get most of your Part A and Part B coverage from your Medicare Advantage Plan, not Original Medicare.
What is a copayment?
A copayment is usually a set amount, rather than a percentage. For example, you might pay or for a doctor's visit or prescription drug.
Does Medicare cover dental?
Covered services in Medicare Advantage Plans. Most Medicare Advantage Plans offer coverage for things Original Medicare doesn’t cover, like some vision, hearing, dental, and fitness programs (like gym memberships or discounts). Plans can also choose to cover even more benefits. For example, some plans may offer coverage for services like ...
Does Medicare Advantage include prescription drug coverage?
Most Medicare Advantage Plans include prescription drug coverage (Part D). You can join a separate Medicare Prescription Drug Plan with certain types of plans that:
What is Medicare Advantage?
Medicare Advantage (sometimes called Medicare Part C or MA) is a type of health insurance plan in the United States that provides Medicare benefits through a private-sector health insurer. In a Medicare Advantage plan, a Medicare beneficiary pays a monthly premium to a private insurance company ...
What is the difference between Medicare Advantage and Original Medicare?
From a beneficiary's point of view, there are several key differences between Medicare Advantage and Original Medicare. Most Medicare Advantage plans are managed care plans (e.g., PPOs or HMOs) with limited provider networks, whereas virtually every physician and hospital in the U.S. accepts Original Medicare.
What happens if Medicare bid is lower than benchmark?
If the bid is lower than the benchmark, the plan and Medicare share the difference between the bid and the benchmark ; the plan's share of this amount is known as a "rebate," which must be used by the plan's sponsor to provide additional benefits or reduced costs to enrollees.
How does capitation work for Medicare Advantage?
For each person who chooses to enroll in a Part C Medicare Advantage or other Part C plan, Medicare pays the health plan sponsor a set amount every month ("capitation"). The capitated fee associated with a Medicare Advantage and other Part C plan is specific to each county in the United States and is primarily driven by a government-administered benchmark/framework/competitive-bidding process that uses that county's average per-beneficiary FFS costs from a previous year as a starting point to determine the benchmark. The fee is then adjusted up or down based on the beneficiary's personal health condition; the intent of this adjustment is that the payments be spending neutral (lower for relatively healthy plan members and higher for those who are not so healthy).
How many people will be on Medicare Advantage in 2020?
Enrollment in the public Part C health plan program, including plans called Medicare Advantage since the 2005 marketing period, grew from zero in 1997 (not counting the pre-Part C demonstration projects) to over 24 million projected in 2020. That 20,000,000-plus represents about 35%-40% of the people on Medicare.
How much does Medicare pay in 2020?
In 2020, about 40% of Medicare beneficiaries were covered under Medicare Advantage plans. Nearly all Medicare beneficiaries (99%) will have access to at least one Medicare Advantage ...
How much has Medicare Advantage decreased since 2017?
Since 2017, the average monthly Medicare Advantage premium has decreased by an estimated 27.9 percent. This is the lowest that the average monthly premium for a Medicare Advantage plan has been since 2007 right after the second year of the benchmark/framework/competitive-bidding process.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
What to know about Medicare Advantage?
Things to know about Medicare Advantage Plans. You're still in the Medicare Program. You still have Medicare rights and protections. You still get complete Part A and Part B coverage through the plan. Some plans offer extra benefits that Original Medicare doesn ’t cover – like vision, hearing, or dental. Your out-of-pocket costs may be lower in ...
How long can you join a health insurance plan?
You can only join a plan at certain times during the year. In most cases, you're enrolled in a plan for a year.
Does Medicare cover dental and vision?
You still get complete Part A and Part B coverage through the plan. P lans may offer some extra benefits that Original Medicare doesn’t cover – like vision, hearing, and dental services.
Can you check with a health insurance plan before you get a service?
You can check with the plan before you get a service to find out if it's covered and what your costs may be. Following plan rules, like getting a Referral to see a specialist in the plan's Network can keep your costs lower. Check with the plan.
Can you pay more for a Medicare Advantage plan than Original Medicare?
Medicare Advantage Plans can't charge more than Original Medicare for certain services like chemotherapy, dialysis, and skilled nursing facility care. Medicare Advantage Plans have a yearly limit on your out-of-pocket costs for medical services. Once you reach this limit, you’ll pay nothing for covered services.
What is a TAB plan?
#TAB#Medical Savings Account (MSA) plans—These plans combine a high-deductible health plan with a bank account. Medicare deposits money into the account (usually less than the deductible). You can use the money to pay for your health care services during the year. MSA plans don’t offer Medicare drug coverage. If you want drug coverage, you have to join a Medicare Prescription Drug Plan. For more information about MSAs, visit Medicare.gov/publications to view the booklet “Your Guide to Medicare Medical Savings Account Plans.”
Can you sell a Medigap policy if you already have a Medicare Advantage Plan?
If you already have a Medicare Advantage Plan, it’s illegal for anyone to sell you a Medigap policy unless you’re disenrolling from your Medicare Advantage Plan to go back to Original Medicare.
Medicare Advantage
You can go to any doctor or hospital that takes Medicare, anywhere in the U.S.
Medicare Advantage
Out-of-pocket costs vary – plans may have different out-of-pocket costs for certain services.
Medicare Advantage
Original Medicare covers most medically necessary services and supplies in hospitals, doctors’ offices, and other health care facilities. Original Medicare doesn’t cover some benefits like eye exams, most dental care, and routine exams.