:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/3722016/TyrGObW.0.jpg)
Medicare doesn’t pay for medically unreasonable and unnecessary services and supplies to diagnose and treat a patient’s condition. Some examples include: Hospital furnished services that, based on the patient’s condition, could have been furnished in a lower-cost setting, such as the patient’s home or a nursing home
Full Answer
What services are not covered by Medicare?
The U.S. Centers for Medicare and Medicaid Services (CMS) recently issued a draft ... Cummings wrote that the risks of ARIA posed by Aduhelm “do not exceed those of cancer therapies that are routinely covered by CMS.” He called limiting treatment ...
What medications are not covered by Medicare?
Some examples of medications that may not be covered by Medicare include: Weight loss or weight gain medications Medications used to treat cold or cough symptoms Fertility medications Vitamins and minerals (with the exception of prenatal vitamins or fluoride preparation products) Medications used ...
Does my supplemental insurance cover what Medicare does not?
Medicare supplement plans don't work like most health insurance plans. They don't actually cover any health benefits. Instead, these plans cover the costs you're responsible for with Original Medicare. These costs can include: Your Medicare deductibles. Your coinsurance. Hospital costs after you run out of Medicare-covered days.
What type of care is not covered by Medicare?
Medicare does not cover items and services that are not reasonable and necessary for the diagnosis or treatment of an illness or injury or to improve the functioning of a malformed body member. Section 1862(a)(1) of the Social Security Act is the basis for denying payment for types of care,…

What is not typically covered by Medicare?
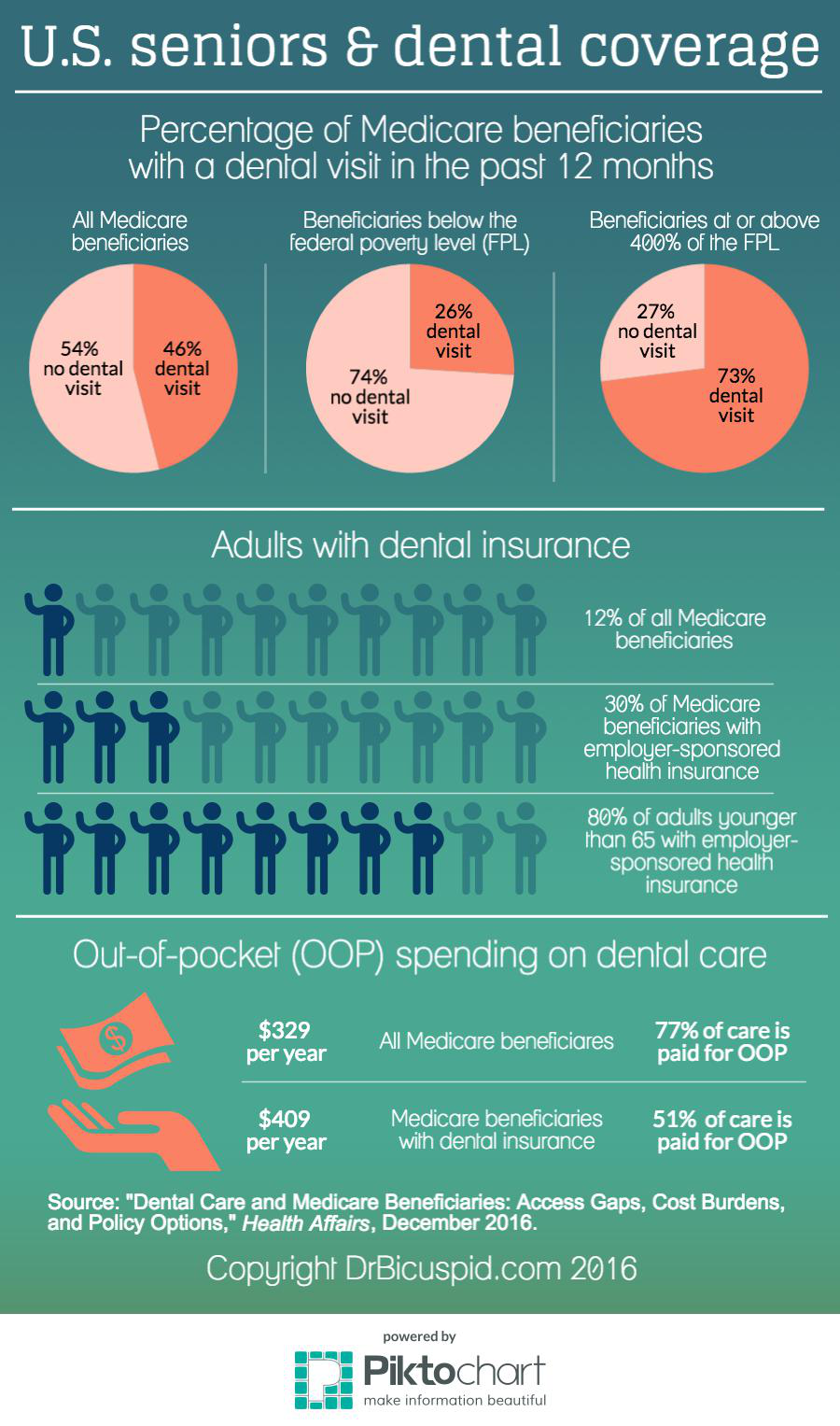
Medicare doesn't provide coverage for routine dental visits, teeth cleanings, fillings, dentures or most tooth extractions. Some Medicare Advantage plans cover basic cleanings and X-rays, but they generally have an annual coverage cap of about $1,500.
What is something Medicare Part A will not pay for?
Part A does not cover the following: A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care.
Is everything free with Medicare?
Medicare is a federal insurance program for people aged 65 years and over and those with certain health conditions. The program aims to help older adults fund healthcare costs, but it is not completely free. Each part of Medicare has different costs, which can include coinsurances, deductibles, and monthly premiums.
Which service is not covered by Part B Medicare?
But there are still some services that Part B does not pay for. If you're enrolled in the original Medicare program, these gaps in coverage include: Routine services for vision, hearing and dental care — for example, checkups, eyeglasses, hearing aids, dental extractions and dentures.
Does Medicare pay 100 of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
Does Medicare cover all costs?
For each lifetime reserve day, Medicare pays all covered costs except for a daily coinsurance. : All costs. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
Is Medicare taken out of your Social Security check?
Yes. In fact, if you are signed up for both Social Security and Medicare Part B — the portion of Medicare that provides standard health insurance — the Social Security Administration will automatically deduct the premium from your monthly benefit.
Does Medicare cover surgery?
Does Medicare Cover Surgery? Medicare covers surgeries that are deemed medically necessary. This means that procedures like cosmetic surgeries typically aren't covered. Medicare Part A covers inpatient procedures, while Part B covers outpatient procedures.
Does Medicare provide groceries?
While Medicare benefits provide coverage for a lot of healthcare needs, the program does not cover grocery delivery services. You may consider asking a family member or friend to help, or look into local community programs that may offer assistance.
Does Medicare pay for cataract surgery?
Medicare covers cataract surgery that involves intraocular lens implants, which are small clear disks that help your eyes focus. Although Medicare covers basic lens implants, it does not cover more advanced implants. If your provider recommends more advanced lens implants, you may have to pay some or all of the cost.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
Does Medicare cover eye exams?
Eye exams (routine) Medicare doesn't cover eye exams (sometimes called “eye refractions”) for eyeglasses or contact lenses. You pay 100% for eye exams for eyeglasses or contact lenses.
What happens if Medicare doesn't pay?
What if Medicare will not pay for something? If Medicare refuses to pay for something, they send you a “denial” letter. The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.”.
What is it called when you think Medicare should not pay?
If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial .”. If you appeal a denial, Medicare may decide to pay some or all of the charge after all. They may “change or reverse the denial.”. You can appeal if:
What happens if you don't get a favorable decision?
If you do not receive a favorable decision, you may appeal to an Administrative Law Judge, then to the Medicare Appeals Council then to Federal Court.
What happens if you appeal Medicare?
If you appeal, Medicare will write back to you and tell you their decision. If they still deny your claim, the letter will include instructions for how to file the next step of the appeal.
How often do you get a Medicare statement?
If you have Part B Original Medicare, you should get a statement every three months. The statement is called a Medicare Summary Notice (MSN). It shows the services that were billed to Medicare. It also shows you if Medicare will pay for these services.
How to contact Medicare Advocacy Project?
If you need help with an appeal, call the Medicare Advocacy Project at 1-800-323-3205 to apply for assistance.
Can Medicare reverse a denial?
They may “change or reverse the denial.”. You can appeal if: Medicare refuses to pay for a health care service, supply or prescription that you think you should be able to get. Medicare refuses to pay the bill for health care services or supplies or a prescription drug you already got.
What services does Medicare cover?
Dentures. Cosmetic surgery. Acupuncture. Hearing aids and exams for fitting them. Routine foot care. Find out if Medicare covers a test, item, or service you need. If you need services Medicare doesn't cover, you'll have to pay for them yourself unless you have other insurance or a Medicare health plan that covers them.
Does Medicare cover everything?
Medicare doesn't cover everything. Some of the items and services Medicare doesn't cover include: Long-Term Care. Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
Does Medicare pay for long term care?
Medicare and most health insurance plans don’t pay for long-term care. (also called. custodial care. Non-skilled personal care, like help with activities of daily living like bathing, dressing, eating, getting in or out of a bed or chair, moving around, and using the bathroom.
Does Medicare cover everything?
But like most forms of health insurance, the program won't cover everything. The services Medicare won't help pay for often come as a surprise and can leave people with hefty medical bills.
Can you get Medicare out of area?
Out-of-Area Care. With traditional Medicare, you can get coverage for treatment if you're hospitalized or need to see a doctor while you're away from home inside the U.S. People covered by Medicare Advantage policies, however, generally need to see doctors within their plan's network for full coverage. If your plan is a preferred provider ...
Does Medicare Advantage cover dental?
Many Medicare Advantage plans, which are Medicare policies administered by private insurers, may offer benefits to help cover the cost of routine dental and vision care. But Lipschutz cautions that these extra benefits, while nice to have, tend to be quite limited.
Does Medicare cover travel to Canada?
When it comes to travel overseas, Medicare rarely covers the cost of medical services, except under special circumstances in Canada or for care delivered on a cruise ship within six hours of a U.S. port.
Does Medicare pay for cataract surgery?
Medicare will help pay for some services, however, as long as they are considered medically necessary. For example, cataract surgery and one pair of glasses following the procedure are covered, although you must pay 20 percent of the cost, including a Part B deductible.
Does Medicare cover chiropractic care?
Alternative treatments such as acupuncture or chiropractics are not typically covered by Medicare. Chiropractic care is covered only in cases in which a licensed chiropractor manually manipulates the spine to correct a condition that causes one or more of the bones of the spine to become dislocated.
Does Medicare Advantage cover emergency services?
And sometimes Medicare Advantage plans offer worldwide coverage for emergencies, but not all plans offer the same extra services or define emergency in the same way.
What are the parts of Medicare?
Medicare health insurance is made up of four major parts: Original Medicare (Parts A and B), Medicare Part C (Medicare Advantage), and Medicare Part D (prescription drug coverage. Each of these parts of Medicare are responsible for providing insurance coverage for differing healthcare needs.
When do you get Medicare?
One first becomes eligible for Medicare as they approach the age of 65, usually beginning in the three months prior to their 65th birthday. As stated, certain individuals may also become eligible for Medicare upon the diagnosis of certain qualifying diseases or disabilities.
How can I find Medicare coverage that works specifically for me?
While Original Medicare Parts A and B can and does offer necessary health insurance coverage to millions of seniors and disabled Americans, Original Medicare doesn’t pay for every aspect of healthcare that you may encounter as you live through your golden years.
What is Medicare Part C?
Medicare Part C (also known as Medicare Advantage) is health insurance coverage that is sold separately by private companies. Usually, Medicare Advantage can cover things that Original Medicare cannot, like dental, vision, and hearing needs.
Does Medicare have a premium charge?
For most Medicare beneficiaries who have paid Medicare taxes for 40 quarters or more, Part A is available with no premium charge. However, if you or your spouse paid Medicare taxes for less than 30 quarters, you must pay a standard Part A premium. If you or your spouse paid Medicare taxes for 30-39 quarters, you must pay a discounted premium.
Does Medicare Advantage cover dental implants?
That being said, most Medicare Advantage plans provide coverage for additional healthcare needs beyond what is covered by Original Medicare. Mostly, this includes things like eyeglasses and contacts, dentures and dental implants, and hearing aids. In some cases, Medicare Advantage may also cover transportation to and from appointments.
Does Medicare cover a large portion of the cost of healthcare?
Original Medicare covers a large portion of the healthcare costs you will encounter after the age of 65, but Original Medicare may also leave specific gaps in your health insurance coverage.
What happens if you don't know what Medicare will cover?
If you don’t know what Medicare will and will not cover, an unexpected bill or expense could send your blood pressure through the roof.
How long does Medicare cover nursing?
Medicare only covers up to 100 days in a skilled nursing facility per benefit period. In order to be covered, the stay must follow a qualifying inpatient stay in the hospital, and you must need a higher level of care than just help with activities of daily living. If you only need custodial care—assistance with eating, bathing, and toileting—Medicare won’t cover your stay.
Does Medicare cover out of pocket prescriptions?
Medigap doesn’t cover your out-of-pocket costs for prescription drugs unless they’re covered under Part A or Part B.
Does Medicare Advantage include Part D?
It’s worth noting that most Medicare Advantage plans also include Part D prescription drug coverage. You get all your benefits in one plan for one monthly premium, which makes Medicare Advantage a convenient alternative for many people.
Will Medicare pay for 2020?
Medicare Won’t Pay for These Six Things. February 7, 2020 By Danielle Kunkle Roberts. Most seniors love their Medicare coverage. Even though Medicare is a bit different from most employer health plans, 9 in 10 seniors are happy with their health care options. That’s the good news.
Does Medicare cover everything?
The bad news is that Medicare doesn’t cover everything, and in fact, some benefits you’re accustomed to with private group health plans aren’t included in Part A and Part B. If you’re not prepared, you might be unpleasantly surprised when you retire and transition to Medicare. With that, here are six things Medicare won’t pay for.
Can foreign providers accept Medicare Advantage plans?
Most Medicare Advantage plans also include some provisions for care outside the U.S., but again, foreign providers aren’t required to accept your plan or bill it on your behalf.
When Medicare or another payer designates a service as “bundled,” does it make separate payment for the pieces of the?
When Medicare or another payer designates a service as “bundled,” it does not make separate payment for the pieces of the bundled service and does not permit you to bill the patient for it since the payer considers payment to already be included in payment for another service that it does cover. Coordination of Benefits.
What are the two resources that Medicare considers medically reasonable?
There are two resources to help you determine if Medicare considers services to be medically reasonable and necessary: national coverage determinations (NCDs) and local coverage determinations (LCDs). These documents provide information regarding CPT and Healthcare Common Procedure Coding System (HCPCS) codes, ICD-10 codes, billing information, as well as service delivery requirements.
What is the modifier for ABN?
If an ABN is obtained, attach modifier -GA (waiver of liability statement issued as required by payer policy, individual case) to the line item (s) within the claim to indicate the patient has been notified.
What are non covered services?
Medicare Non-covered Services. There are two main categories of services which a physician may not be paid by Medicare: Services not deemed medically reasonable and necessary. Non-covered services. In some instances, Medicare rules allow a physician to bill the patient for services in these categories. Understanding these rules and how ...
Do you need to get a signature on an advance beneficiary notice?
This should be done before you provide the service. If a Medicare patient wishes to receive services that may not be considered medically reasonable and necessary, or you feel Medicare may deny the service for another reason , you should obtain the patient’s signature on an Advance Beneficiary Notice (ABN).
Is it reasonable to ask for a service from Medicare?
Medically Reasonable and Necessary. A patient may ask for a service that Medicare does not consider medically reasonable and necessary under the circumstances. For instance, the patient wants the service more frequently than Medicare allows or for a diagnosis that Medicare does not cover.
Is cosmetic surgery covered by Medicare?
Cosmetic procedures are never covered unless there is a medically-necessary reason for a procedure. In this instance, you should document and code it as such. Services rendered to immediate relatives and members of the household are not eligible for payment.
Does Medicare cover exceptions?
This booklet outlines the 4 categories of items and services Medicare doesn’t cover and exceptions (items and services Medicare may cover). This material isn’t an all-inclusive list of items and services Medicare may or may not cover.
Does Medicare cover personal comfort items?
Medicare doesn’t cover personal comfort items because these items don’t meaningfully contribute to treating a patient’s illness or injury or the functioning of a malformed body member. Some examples of personal comfort items include:
Does Medicare cover non-physician services?
Medicare normally excludes coverage for non-physician services to Part A or Part B hospital inpatients unless those services are provided either directly by the hospital/SNF or under an arrangement that the hospital/SNF makes with an outside source.
Does Medicare cover dental care?
Medicare doesn’t cover items and services for the care, treatment, filling, removal, or replacement of teeth or the structures directly supporting the teeth, such as preparing the mouth for dentures, or removing diseased teeth in an infected jaw. The structures directly supporting the teeth are the periodontium, including:
Can you transfer financial liability to a patient?
To transfer potential financial liability to the patient, you must give written notice to a Fee-for-Service Medicare patient before furnishing items or services Medicare usually covers but you don’ t expect them to pay in a specific instance for certain reasons, such as no medical necessity .
What about Medicare Advantage plans?
The price for Medicare Advantage (Part C) plans greatly varies. Depending on your location, you may have dozens of options, all with different premium amounts. Because Part C plans don’t have a standard plan amount, there are no set income brackets for higher prices.
What is Medicare Part B?
Medicare Part B. This is medical insurance and covers visits to doctors and specialists, as well as ambulance rides, vaccines, medical supplies, and other necessities.
What about Medicaid?
If you qualify for Medicaid, your costs will be covered. You won’t be responsible for premiums or other plan costs.
What is the Medicare Part D premium for 2021?
Part D plans have their own separate premiums. The national base beneficiary premium amount for Medicare Part D in 2021 is $33.06, but costs vary. Your Part D Premium will depend on the plan you choose.
How much is Medicare Part B 2021?
For Part B coverage, you’ll pay a premium each year. Most people will pay the standard premium amount. In 2021, the standard premium is $148.50. However, if you make more than the preset income limits, you’ll pay more for your premium.
How does Social Security determine IRMAA?
The Social Security Administration (SSA) determines your IRMAA based on the gross income on your tax return. Medicare uses your tax return from 2 years ago. For example, when you apply for Medicare coverage for 2021, the IRS will provide Medicare with your income from your 2019 tax return. You may pay more depending on your income.
How many types of Medicare savings programs are there?
Medicare savings programs. There are four types of Medicare savings programs, which are discussed in more detail in the following sections. As of November 9, 2020, Medicare has not announced the new income and resource thresholds to qualify for the following Medicare savings programs.