How much does Medicare pay for in home health care?
Jun 20, 2019 · If you qualify for home health care under Medicare, you generally don’t have to pay any coinsurance or copayment. If you need durable medical equipment, you’ll typically pay 20% of the Medicare-approved amount as coinsurance. Read more about Medicare and durable medical equipment. When does Medicare not cover in-home health care?
How long does Medicare pay for home health care?
Feb 11, 2022 · Medicare will pay for home health care costs if you meet all criteria for participation. Original Medicare allows you to go to any home health care agency that is a Medicare contracted provider. The agency should also tell you if Medicare doesn’t cover any items or services and how much you'll have to pay. This should be explained by both telling you …
What does Medicare cover for home health?
Medicare will cover 100% of the costs for medically necessary home health care provided for less than eight hours a day and a total of 28 hours per week. The average cost of home health care as of 2019 was $21 per hour. Many seniors opt for home health care if they require some support but do not want to move into an assisted living community.
Is home health care covered by Medicare?
Medicare usually pays 80% of the Medicare-approved amount for certain pieces of medical equipment, like a wheelchair or walker. If your home health agency doesn’t supply durable medical equipment directly, the home health agency staff will usually arrange for a home equipment supplier to bring the items you need to your home. Note:
What Is Home Health Care?
Home health care can involve a wide range of services you may need when you’re ill or recovering from an illness or surgery. In some cases it can i...
In-Home Care: Medical and Non-Medical
Depending on what is available in your community, home care can include: 1. Health care – skilled nursing care; physical, speech, occupational and...
Does Medicare Cover Home Health Care?
Medicare Part A and/or Part B may help pay for your home health care if these conditions apply to you: 1. You’re under the care of a doctor who acc...
Home Health Care and Medicare Supplement Insurance
You might have to pay a coinsurance amount in some cases; for example, under Medicare Part B, you usually pay 20% of durable medical equipment cost...
Not All Home Health Care Agencies Are Created Equal
Home health agencies vary in the services they offer, and not every agency is certified by Medicare. You may want to match your needs with the serv...
What is home health aide?
Home health aides, when the only care you need is custodial. That means you need help bathing, dressing, and/or using the bathroom. Homemaker services, like cleaning, laundry, and shopping. If these services aren’t in your care plan, and they’re the only care you need, they’re generally not covered.
Does Medicare Advantage have a deductible?
Medicare Advantage plans may have annual deductibles, and may charge coinsurance or copayments for these services. Medicare Advantage plans have out-of-pocket maximum amounts, which protect you from unlimited health-care spending.
Do you have to pay coinsurance for osteoporosis?
Medical supplies. Injectable osteoporosis drugs. If you qualify for home health care under Medicare, you generally don’t have to pay any coinsurance or copayment. If you need durable medical equipment, you’ll typically pay 20% of the Medicare-approved amount as coinsurance.
Does Medicare cover in-home care?
When might Medicare cover in-home health care? In general, Medicare doesn’t cover long- term home health care. Here’s how Medicare coverage of in-home health care typically works. In most cases, even when Medicare covers in-home health care, it’s for part-time care, and for a limited time.
Do you have to be Medicare approved to be homebound?
The in-home health agency must be Medicare-approved. Your doctor must certify that you’re unable to leave your home without some difficulty – for example, you might need transportation and/or help from a cane, a walker, a wheelchair, and/or someone to help you. In other words, you’re homebound.
Will Medicare Pay for Home Health Care Costs?
Medicare will pay for home health care costs if you meet all criteria for participation. Original Medicare allows you to go to any home health care agency that is a Medicare contracted provider. The agency should also tell you if Medicare doesn’t cover any items or services and how much you'll have to pay.
What Home Health Care Services Will Medicare Cover?
Medicare will cover a wide range of healthcare services under the home health care benefit, but you may not need all of them depending on the condition that qualified you to begin with. However, you have to have some need for professional services to be eligible for home health care services.
What Home Health Care Services Will Medicare NOT Cover?
There are services Medicare will not pay for, which may come as a surprise to some families. If your loved one needs some of the care that Medicare will not cover, you will need to consider family caregiving or private-pay caregivers. Medicare will not cover the following under the home health care benefit:
How Do You Qualify for Home Health Care Coverage?
For Medicare to qualify you for home health coverage, you must meet specific criteria. If you’re in doubt about qualifying, contact your physician first to tell you whether they are willing to write an order for services.
How Do You Get Medicare to Pay for These Costs?
As the recipient of home health services with a Medicare provider, you would not typically need to get Medicare to pay for costs. Medicare pays your Medicare-certified home health agency for the covered services you get during a 30-day period of care.
Medicare Payment for Home Health Care Costs
Although it’s a beneficial healthcare program, Medicare can be complicated to understand. Benefits through medicare are numerous but require an understanding of the criteria for participation. This is especially true of Medicare Advantage plans. Home healthcare costs are covered under Medicare if you follow the rules for participation.
Medicare Covers Medically Necessary Home Health Services
Medicare does not usually cover the cost of non-medical home care aides if that is the only type of assistance that a senior needs.
Medicare Advantage May Offer More Comprehensive Coverage
Private insurance companies run Medicare Advantage. Those companies are regulated by Medicare and must provide the same basic level of coverage as Original Medicare. However, they also offer additional coverage known as “supplemental health care benefits.”
How long does Medicare pay for home health?
Medicare pays your Medicare-certified home health agency one payment for the covered services you get during a 30-day period of . care. You can have more than one 30-day period of care. Payment for each 30-day period is based on your condition and care needs.
What is a home health nurse?
If you get services from an LPN, your care . will be supervised by an RN. Home health nurses provide direct care and teach you and your caregivers about your care. They also manage, observe, and evaluate your care.
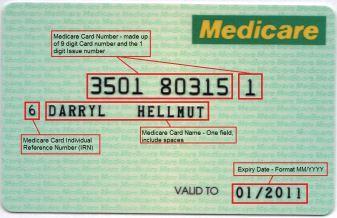
How to contact Medicare after printing?
Changes may occur after printing. Visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) to get the most current information. TTY users can call 1-877-486-2048. “Medicare & Home Health Care” isn’t a legal document. Official Medicare Program legal guidance is contained in the relevant statutes, regulations, and rulings. 3.
What is an appeal in Medicare?
Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
How to contact the Long-Term Care Ombudsman?
information on the home health agencies in your area. Visit ltcombudsman.org, visit eldercare.gov, or call the eldercare locator at 1-800-677-1116. To find out more about home health agencies, you can: .
What happens when home health services end?
When all of your covered home health services are ending, you may have the right to a fast appeal if you think these services are ending too soon. During a fast appeal, an independent reviewer called a Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) looks at your case and decides if you need your home health services to continue.
Why is home health important?
Where possible, home health care helps you get better, regain your independence, and become as self-sufficient as possible. Home health care may also help you maintain your current condition or level of function, or to slow decline.
What is home health care?
Home health care is an alternative to traditional in-hospital care that’s growing in popularity. Care at home offers convenience, ease of access and peace of mind for many families in the US. However, like all other health care options, cost is often a consideration. Not all families can afford to pay in full for home health care services out ...
How much does it cost to hire a home health aide?
In fact, hiring a home health aide to care for an elderly loved one for 40-44 hours a week can cost as little $5000 monthly . Compare that cost to a nursing home, which can cost almost $7000 a month, by comparison. Keep in mind that home health aides aren’t qualified nurses and can’t administer skilled health care services.
How is Medicare funded?
Medicare is a government health plan funded through tax money. Most people contribute to Medicare during their working years. In the same way you contribute to social security tax, part of your income tax goes towards Medicare cover.
Can a home health aide administer wound care?
Keep in mind that home health aides aren’t qualified nurses and can’t administer skilled health care services. A health aide won’t be able to deliver complex wound care. Your health aide also won’t be able to deliver medications through an IV or to tube feed a patient, as these all require the skills of a nurse.
Can you claim home health care for indefinitely?
The home health care treatment must be part of a plan prescribed by a doctor or qualified medical professional. Necessary services can’t be claimed for indefinitely. This means that you can only claim for a set duration of time as prescribed by a qualified health care professional.
Does Medicare pay for home health care?
Medicare won’t pay for home health care services if they aren’t administered through a registered home health care agency. Furthermore, Medicare won’t pay if you only require minor household services like cleaning, cooking and shopping.
Do you have to pay monthly premiums for Medicare?
Upon retirement, American tax payers normally qualify for Part A Medicare cover automatically without the need to pay monthly premiums. Part A covers hospital care or the cost of being in a medical facility.
What Is In-Home Care?
In-home care (also known as “home health care”) is a service covered by Medicare that allows skilled workers and therapists to enter your home and provide the services necessary to help you get better.
What Parts Of In-Home Care Are Covered?
In-home care can cover a wide range of services, but they’re not all covered by Medicare. According to the Medicare site, the in-home care services covered by parts A and B include:
How To Get Approved For In-Home Care
There are a handful of steps and qualifications you need to meet to have your in-home care covered by Medicare. It starts with the type of help your doctor says you or your loved one needs and includes other aspects of care.
Cashing In On In-Home Care
Once you qualify for in-home care, it’s time to find the right agency who will provide you or your loved one services. The company you receive your services from is up to you, but they must be approved by Medicare in order for their services to be covered.
How To Pay for In-Home Care Not Covered By Medicare
There may be times when not every part of your in-home care is covered. We already know 20 percent of the durable medical equipment needed to treat you is your responsibility, but there are other services like custodial care or extra round-the-clock care that won’t be covered by Medicare. This is where supplemental insurance (Medigap) comes in.
How long does home health care take before Medicare benefits apply?
The home health care must follow a qualifying hospital stay of at least three days before your Medicare benefits apply. If you haven’t had a hospital stay, Medicare Part B might still cover home health care visits.
How long does Medicare cover home health aides?
Medicare generally covers fewer than seven days a week of home health aide visits, and fewer than eight hours of care per visit.
How many hours of home health aides can Medicare cover?
For example, the plan may choose to cover up to 50 hours per year of home health aide services, or 20 transportation trips per year.
What is Medicare Advantage?
Medicare Advantage plans are offered by private insurance companies. They must provide the same coverage as Original Medicare at a minimum. Some many plans offer additional benefits to their members, including expanded coverage for home health care.
What does it mean to be homebound?
You must be certified by your doctor as homebound, which means you are unable to leave home without assistance or special transportation. Medicare may consider you homebound if leaving the house requires “considerable and taxing effort.”. Your doctor must monitor the services you receive at home.
Does Medicare Part B cover home care?
If you haven’t had a hospital stay, Medicare Part B might still cover home health care visits. Your doctor would need to recommend these visits as part of a formal, written treatment plan. Part B generally covers 80% of allowable charges for durable medical equipment and devices you need for your treatment at home. Your Part B deductible applies.
Does Medicare cover home health?
If you need Medicare home health care after a hospitalization or due to a condition that keeps you homebound, Medicare might cover a home health aide. Here’s the information you need to know about Medicare coverage of home health services. A Medicare Advantage plan might cover some home health services.
How to qualify for home health care?
Ideally, home health can enhance your care and prevent re-admission to a hospital. There are several steps and conditions to qualify for home health care: 1 You must be under the care of a doctor who has created a plan for you that involves home health care. Your doctor must review the plan at regular intervals to make sure it is still helping you. 2 Your doctor must certify that you need skilled nursing care and therapy services. To need this care, your doctor must decide that your condition will improve or maintain through home health services. 3 Your doctor must certify that you are homebound. This means it is very difficult or medically challenging for you to leave your home.
What is home health aide?
Home health aides are health professionals who help people in their home when they have disabilities, chronic illnesses, or need extra help. Aides may help with activities of daily living, such as bathing, dressing, going to the bathroom, or other around-the-home activities. For those who need assistance at home, home health aides can be invaluable.
What is the difference between home health and skilled nursing?
The difference is that, for reimbursement, you must be getting skilled nursing services as well.
What is Medicare Part A?
Medicare Part A is the portion that provides hospital coverage. Medicare Part A is free to most individuals when they or their spouse worked for at least 40 quarters paying Medicare taxes.
What education do you need to be a home health aide?
According to the U.S. Bureau of Labor Statistics, the typical educational level for a home health aide is a high school diploma or equivalent. Some people may use the term “home health aide” to describe all occupations that provide care at home, but a home health aide is technically different from a home health nurse or therapist.
Who must review home health care plans?
You must be under the care of a doctor who has created a plan for you that involves home health care. Your doctor must review the plan at regular intervals to make sure it is still helping you. Your doctor must certify that you need skilled nursing care and therapy services.
Is long term care insurance part of Medicare?
Some people choose to purchase separate long-term care insurance, which isn’t a part of Medicare . These policies may help to cover more home health care services and for longer time periods than Medicare. However, the policies vary and do represent an extra cost to seniors.
