What Is Medicare Credentialing?
- Becoming a Medicare Provider. If you want to serve patients with Medicare, it is not as simple as opening your doors to...
- Medicare Credentialing Requirements. Medicare will require you to meet all of the credentialing and licensing...
- Maintaining Medicare Credentials. Once you meet Medicare credentialing standards and have been approved...
Full Answer
How to become credentialed with Medicare?
± Eligibility for Participation in Medicare (Excluded and Opt -Out) - Quality of Care Issues, Grievances etc.(usually at recredentialing) In addition, credentialing must include a Completed Application and the use of Current Documents ( The information used in the review must be no more than 6 months old on the date of determination.)
How much can you make to qualify for Medicare?
This Webinar Covers Everything You Need To Know About Medicare Credentialing To Billing. Who has medicare? What populations? Difference between Social Security Disability Insurance (SSDI) & Supplemental Security Income (SSI) The different types of Medicare, how to know the difference with A,B,C and D. Exact steps to get credentialed with Medicare.
How to enroll in Medicare if you are turning 65?
Dec 01, 2021 · Medicare Participating Physician or Supplier Agreement (Form CMS-460) Submit Your Application When you’ve completed your paper application, print it and sign it. Your signature is required to be handwritten when you submit a paper application.
How to get Medicaid and Medicare certified?
Apr 01, 2020 · What Is Medicare Credentialing? Becoming a Medicare Provider. If you want to serve patients with Medicare, it is not as simple as opening your doors to... Medicare Credentialing Requirements. Medicare will require you to meet all of the credentialing and licensing... Maintaining Medicare ...

What does it mean to be credentialed with Medicare?
Credentialing is the process of approving a physician, agency or other medical provider as part of the Medicare supply chain.Apr 1, 2020
What is required to bill Medicare?
In summary, a provider, whether participating or nonparticipating in Medicare, is required to bill Medicare for all covered services provided. If the provider has reason to believe that a covered service may be excluded because it may be found not to be reasonable and necessary the patient should be provided an ABN.
What does it mean to be CMS certified?
Certification is when the State Survey Agency officially recommends its findings regarding whether health care entities meet the Social Security Act's provider or supplier definitions, and whether the entities comply with standards required by Federal regulations.
Is accreditation mandatory for Medicare?
Accreditation by an AO is voluntary and is not required for Medicare certification or participation in the Medicare Program. A provider's or supplier's ability to bill Medicare for covered services is not impacted if it chooses to discontinue accreditation from a CMS-approved AO or change AOs.Dec 1, 2021
What triggers payment of Medicare Part A benefits?
If you're under 65, you get premium-free Part A if: You have Social Security or Railroad Retirement Board disability benefits for 24 months. You have End-Stage Renal Disease (ESRD) or Amyotrophic Lateral Sclerosis (ALS) and meet certain requirements.
Who is responsible for Medicare billing?
Non-participating providers must submit claims to Medicare on behalf of their Medicare patients, but Medicare reimburses the patient, rather than the nonparticipating provider, for its portion of the covered charges. A small share (4%) of providers who provide Medicare-covered services are non-participating providers.Nov 30, 2016
How long does it take to become Medicare certified?
Most Medicare provider number applications are taking up to 12 calendar days to process from the date we get your application. Some applications may take longer if they need to be assessed by the Department of Health.Jan 25, 2022
What is the difference between credentialing and accreditation?
As nouns the difference between credentials and accreditation. is that credentials is (credential): documentary evidence of someone's right to credit or authority, especially such a document given to an ambassador by a country while accreditation is the giving of credentials.
How is Medicare regulated?
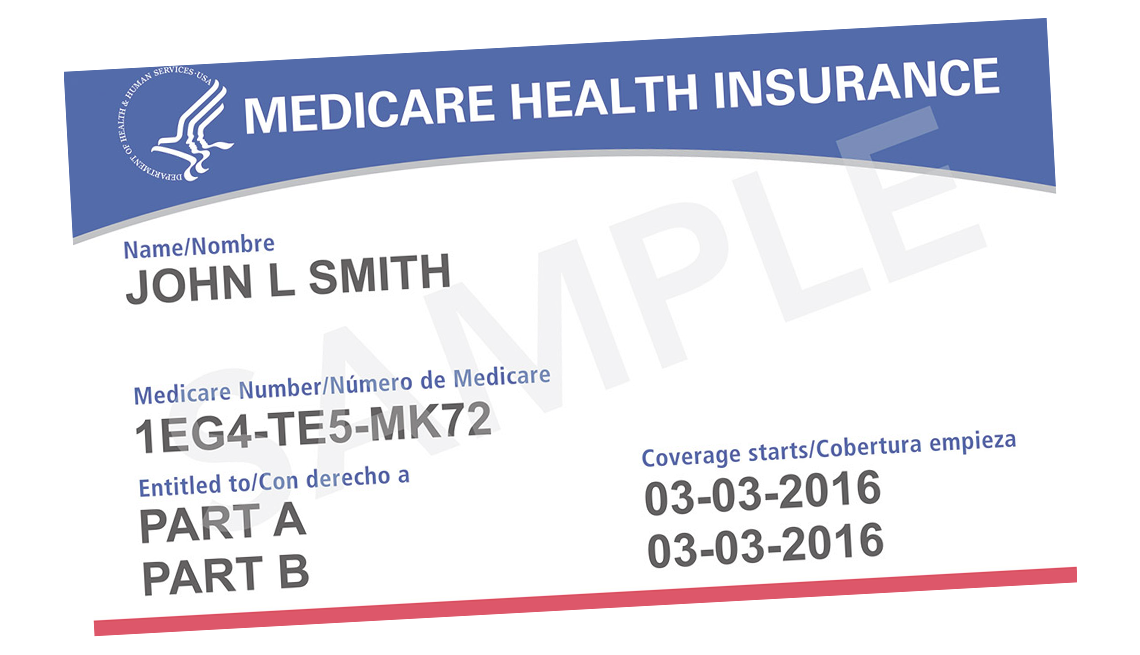
Medicare is a federal health insurance program regulated by the Centers for Medicare and Medicaid Services (CMS). As a member currently enrolled in a CalPERS Medicare health benefits plan, you don't need to provide CalPERS with your new card or MBI number.Feb 23, 2022
What is Medicare compliance?
The Medicare Compliance Program is specifically designed to prevent, detect, and correct noncompliance as well as fraud, waste, and abuse.
What is the difference between CMS and TJC?
While TJC is an independent and not for profit group, it has fixed its standards based on CMS guidelines, and, in some cases, exceeds established federal requirements. As a result, CMS has identified TJC as an entity able to accredit hospitals and other health care organizations.Nov 12, 2020
Why does the state and Medicare require accreditation?
Why Medicare Accreditation is Important Staging of the process provides information for management to make decisions regarding operations, whether they are business or patient-care related, in order to improve effectiveness and efficiency of Home Health Care Business performance.
What is Medicare credentialing?
Medicare approves a variety of individual practitioners, agencies and facilities to provide high-quality care to Medicare recipients. Medicare credentialing standards vary depending on the type of services you are providing.
What are the requirements for a medical license?
Medicare will require you to meet all of the credentialing and licensing requirements of your field. As such, be prepared to provide the following documentation as part of the application process: 1 Tax records 2 Proof of malpractice insurance 3 Practitioner licenses 4 Diplomas 5 Board certifications 6 Federal and state CDS certificates 7 Current CV using a month and year format 8 Proof of identification
How long does it take for Medicare to bill?
Once you submit all of your paperwork, expect it to take two to three months for your application to be reviewed and either accepted or denied. Once you are an approved Medicare provider, you will be able to bill retroactively for all services provided during the waiting period.
How often do you need to resubmit Medicare enrollment application?
Once you meet Medicare credentialing standards and have been approved as a provider, you need to keep up your credentials. Every three years, you will need to resubmit the Medicare enrollment application CMS-855I.
How long does it take to get a psychologist's license?
Once you submit all of your paperwork, expect it to take two to three months for your application to be reviewed and either accepted or denied.
Who is Anne Kinsey?
Accessed July 17, 2020. Writer Bio. Anne Kinsey is an entrepreneur and business pioneer, who has ranked in the top 1% of the direct sales industry, growing a large team and earning the title of Senior Team Manager during her time with Jamberry.
Can you file an electronic claim with Medicare?
Once you are credentialed through Medicare, you must ensure that you bill accurately for every Medicare patient you serve. Electronic claims are simple to file from your computer and are delivered directly to the Medicare Administrative Contractor. If claims do not meet HIPAA standards, they might be rejected and need to be resubmitted.
What to do if you don't have an NPI?
If you do not have an NPI, start with NPPES and obtain an NPI. Most providers in residency will already have an NPI so if you’re not sure, do a search on the NPI Registry to see if you’re listed. If you are, you simply need to reset your login info using your personal info.
What is CMS 855O?
CMS-855O for Ordering and Certifying Physicians and Non-Physician Practitioners. This is used for providers who do not want to participate with Medicare but do refer Medicare patients as a nonpar provider.
How to enroll in PECOS?
There are primarily four ways that you will be enrolling in PECOS which are as follows: 1 Enrolling as an employee/contractor of an established Medicare Provider/Supplier 2 Enrolling as a provider and owner of a new Medicare supplier 3 Enrolling as an owner/managing investor of a new Medicare supplier 4 Enrolling as an individual of a sole proprietorship
What is medical credentialing?
Medical credentialing offers quality assertion to the medical industry that advantage all involved parties. Clinics as well as hospitals may be self-assured that the staff they employ to offer care as per the guided standards. Payers operate on the incentive-based model that leads to cut down their costs and so select to make sure only those professionals who manifest enough competence to practice medicine.
What is a CVO?
The credentialing organization, which is the authority for medical credentialing, known as a Credentials Verification Organization ( CVO ). The duties of the organization involve communicating with universities where providers completed their medicine education, did their internship, to verify, confirm, and review their credentials such as licenses or certifications. Though medical credentialing looks a very simple process, it can be a confusing and complex practice, since different healthcare providers need multiple types of certification as well as education. Credentialing is essential for new graduates and new hires .However, it accomplished at regular time interval even after appointing new graduates in order to follow the standards of an accrediting and regulatory organization such as The Centers for Medicare and Medicaid Services (CMS), The Joint Commission (TJC), and the National Committee for Quality Assurance (NCQA).
Can a healthcare practitioner work in between credentialing?
A healthcare practitioner is unable to work in between credentialing. He/she have to wait until the approval and completion of the credentialing procedure before they initiate their practice. This guarantees each patient at whole times that they get care from providers who possess thorough knowledge, experience, and training to diagnose and treat their healthcare issues. If a practitioner allows working meanwhile the credentialing process, a facility is setting itself at legal risk at the same time in jeopardy of failing its own credentials as an institution.
What is credentialing in healthcare?
Credentialing in the healthcare industry sometimes goes by other terms, including the following: Insurance Credentialing: Also known informally as “getting on insurance panels,” this term refers to a health insurance company verifying a physician’s credentials.
What is provider credentialing?
Provider credentialing in healthcare is the process by which medical organizations verify the credentials of healthcare providers to ensure they have the required licenses, certifications, and skills to properly care for patients. The process is also called physician credentialing, medical credentialing, or doctor credentialing.
How long does it take to get a physician credentialed?
Under the most efficient circumstances, a physician can be credentialed to work at a hospital or credentialed and approved to be in-network for a health insurance company in 30 days. More often, the process takes 60 to 90 days. And on occasion — especially with insurance companies — it can take six months or more.
What is a medical sales rep?
Medical sales rep credentialing: Also known as vendor credentialing, this refers to healthcare organizations checking on and monitoring the background and training of sales reps and other vendors who may want or need access to the facilities. Credentialing is also used in non-medical contexts, including the following:
What is a CVO in healthcare?
In some cases, the healthcare facility or insurance company works with a third-party company — called a credentials verification organization (CVO) — that works with the provider to gather and verify information. Organizations often hire CVOs to allow for more efficient credentialing. 2. Check the Information.
What is a CAQH?
The Council for Affordable Quality Healthcare (CAQH) is a not-for-profit organization formed by some of the nation’s top health insurance companies . One of its online products — formerly called the Universal Provider Datasource and now known as ProView — gathers a common set of information from healthcare providers, including their professional background. Hundreds of insurance plans then use that common information as they credential providers — and relieve providers of the burden of submitting the same information to every insurance company they may want to enroll with.
Do hospitals have to be credentialed?
Healthcare organizations that don’t follow the CMS regulations are not eligible for Medicare or Medicaid reimbursement. Similarly, the Joint Commission accredits only those who follow its regulations. Most U.S. hospitals pursue the Joint Commission accreditation, which is required for Medicare and Medicaid reimbursement eligibility. States also have their own regulations.
Why is credentialing important for physicians?
It allows patients to trust that they’re in good hands and physicians to have trust in their peers. Credentialing also plays a part in physician health plan enrollment so that payment for services can be received. For residents, having a knowledge base about the process and how it can be used can go a long way.
Do physicians have to go through the credentialing process?
Anytime a physician changes employers or seeks new privileges, they are required to go through the credentialing process. For residents and fellows wrapping up their training, credentialing is one of the first steps to working as a practicing physician.
