Medicare is the secondary payer for beneficiaries with supplemental coverage from a group health insurance plan for individuals ages 65 and older if the employer has more than 20 employees and for people under the age of 65 with a disability if the employer has 100 employees or more.
Full Answer
How many Medicare beneficiaries have supplemental insurance?
If your employer’s insurance covers more than 20 employees, Medicare will pay secondary and call your work-related coverage a Group Health Plan (GHP). Delaying Medicare Coverage If you have good insurance as a result of your, or your partner’s, employment when you become eligible to enroll in Medicare benefits, you may consider delaying your enrollment.
How many Medicare beneficiaries also have employer-sponsored retirement health coverage?
Aug 14, 2021 · Once you retire and choose to keep Medicare and employer coverage, Medicare Part B will become primary. Thus, your employer coverage will be secondary. Once retired, many beneficiaries find it more suitable to drop employer coverage …
Is it illegal for employers to contribute to Medicare premiums?
How Medicare coordinates with other coverage. If you have questions about who pays first, or if your coverage changes, call the Benefits Coordination & Recovery Center at 1-855-798-2627 (TTY: 1-855-797-2627). Tell your doctor and other. health care provider about any changes in your insurance or coverage when you get care. I have Medicare and:
Do I need my employer to fill out a Medicare form?
If that former employer DOES offer coverage, your benefits will likely change when you turn 65. This is because when you are age 65 and have retiree coverage, Medicare becomes your primary insurance, and your group coverage now pays secondary. Prices and benefits from your employer coverage may be different once you turn 65.
When a Medicare beneficiary has employer supplemental coverage Medicare refers to these plans as?
How do Medicare supplements help beneficiaries?
What percent of Medicare beneficiaries have some form of supplemental insurance?
How do I update my Medicare cob?
How is Medicare supplement divided?
What is the difference between a Medicare Supplement and a Medicare Advantage Plan?
Do I have to have supplemental insurance with Medicare?
How many Medicare enrollees purchase some form of supplemental insurance?
What is the average cost of supplemental insurance for Medicare?
What is the difference between COB and EOB in medical billing?
What is the purpose of a Medicare carve out or supplements?
How do you fix coordination of benefits?
- Avoid duplicate payments by making sure the two plans don't pay more than the total amount of the claim.
- Establish which plan is primary and which plan is secondary—the plan that pays first and the plan that pays any remaining balance after your share of the costs is deducted.
Medicare and Employer Coverage – Large Companies 20+ Employees
Medicare is secondary if your employer has more than 20 employees and you are ACTIVELY working (not a retiree or on COBRA). This is called Medicare...
Medicare as Secondary Insurance Costs Money
Now Part B is not premium-free. You will pay a monthly premium for Part B based on your income. Some people eligible for Medicare and employer grou...
Medicare and Employer Coverage – Small Companies Under 20 Employees
Medicare is primary if your employer has less than 20 employees. You will need both Part A & B for sure because Medicare will pay first, and then y...
Can Your Employer Pay Your Medigap Premium?
We often get questions here at Boomer Benefits about whether an employer can pay for your Medigap plan. This idea might appeal to both you and your...
Can My Employer Kick Me Off My Group Health Insurance When I Turn 65?
It’s illegal for an employer to force any actively working employee to choose Medicare instead of their group health plan. You have the option to l...
Can You Enroll in A Medigap Plan Even If You Have Employer Coverage at A Large Employer, Just to Be Sure?
This would be a waste of money. A Medigap cannot pay for anything unless Medicare is your primary insurance. The insurance company’s application wi...
What determines if you are a primary or secondary employer for Medicare?
The size of your employer will determine how your Medicare benefits will coordinate with your employer coverage. If you’re aging into Medicare while working for an employer with over 20 employees, your group plan is primary and Medicare secondary.
How many employees are eligible for creditable insurance?
For your outpatient and medication insurance, a plan from an employer with over 20 employees is creditable coverage. This safeguards you from having to pay late enrollment penalties for Part B and Part D, respectively.
What happens if you leave Medicare without a creditable coverage letter?
Without creditable coverage during the time you’ve been Medicare-eligible, you’ll incur late enrollment penalties. When you leave your group health coverage, the insurance carrier will mail you a creditable coverage letter. You’ll need to show this letter to Medicare to protect yourself from late penalties.
What is a Health Reimbursement Account?
Beneficiaries who participate can get tax-free reimbursements, including their Part B premium. A Health Reimbursement Account is a well-known Section 105 plan. An HRA reimburses eligible employees for their premiums, as well as other medical costs.
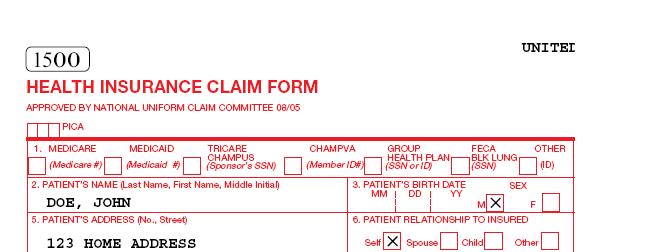
What is CMS L564?
You will need your employer to fill out the CMS-L564 form. This form is a request for employment information form. Once the employer completes section B of the form, you can send in the document with your application to enroll in Medicare.
What happens if you don't have Part B insurance?
If you don’t, your employer’s group plan can refuse to pay your claims. Your insurance might cover claims even if you don’t have Part B, but we always recommend enrolling in Part B. Your carrier can change that at any time, with no warning, leaving you responsible for outpatient costs.
Can you drop your Medicare coverage at 65?
An employer can never force you to drop your group coverage and enroll in Medicare once you turn 65. You can always choose to have Medicare and decline your group plan, but your employer can never force that decision.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.
When does Medicare change?
If that former employer DOES offer coverage, your benefits will likely change when you turn 65. This is because when you are age 65 and have retiree coverage, Medicare becomes your primary insurance, and your group coverage now pays secondary. Prices and benefits from your employer coverage may be different once you turn 65.
Why is Medicare different from Cobra?
A Word About COBRA. Medicare coordinates differently with COBRA than it does with active coverage. This is important because so many people get this wrong and then owe penalties. When you are still actively working at a large employer, their Group Insurance pays primary and Medicare pays secondary.
What is a 105 reimbursement plan?
A Section 105 Reimbursement Plan allows the employer to deduct expenses for employees who purchase individual health insurance plans. Eligible employees can participate and the employer can reimburse premiums for Medicare Parts A and B as well as Medigap plans.
How much is Medicare Part A deductible in 2021?
The Medicare Part A hospital deductible is $1,484 in 2021. So if you have both your employer insurance and Part A, and you incur a bill for a hospital stay, you will only be out $1,484 for your inpatient hospital services. Medicare pays the rest of any Part A services.
What does "active employer" mean?
Active employer coverage means you are still actively working, not retired. In this scenario, you have the right to remain on your employer’s group health insurance plan if you choose. Your Medicare benefits can coordinate with that coverage. HOW it coordinates depends on the size of your employer.
Why would an insurance company reject my application?
When they see that you have large group coverage, they may reject your application because they know it will be of no use to you. Medicare and Employer coverage will be good enough coverage.
Which pays first, Medicare or Cobra?
The opposite is true of COBRA. Medicare pays first and COBRA pays second.
How many Medicare beneficiaries were there in 2016?
In 2016, 6.1 million Medicare beneficiaries—nearly 1 in 5 (19%) Medicare beneficiaries in traditional Medicare—had no other source of coverage. Compared to all traditional Medicare beneficiaries in 2016, a larger share of beneficiaries with no supplemental coverage had modest incomes (between $20,000 and $40,000), were age 85 or older, and male. ...
How many people had supplemental insurance in 2016?
Sources of Supplemental Coverage in 2016. In 2016, eight in 10 beneficiaries in traditional Medicare (81%) had some type of supplemental insurance, including employer-sponsored insurance (30%), Medigap (29%), and Medicaid (22%) (Figure 1). But nearly 1 in 5 beneficiaries in traditional Medicare ...
What is Medicaid in 2016?
Medicaid, the federal-state program that provides health and long-term care coverage to low-income people, was a source of supplemental coverage for more than 1 in 5 (22%, or 7.0 million) traditional Medicare beneficiaries with low incomes and modest assets in 2016 (not including 3.5 million beneficiaries who were enrolled in both Medicare Advantage and Medicaid). For these beneficiaries, sometimes called dual eligible beneficiaries because they are eligible for both Medicare and Medicaid, Medicaid typically covers the Medicare Part B premium and may also pay a portion of Medicare deductibles and other cost-sharing requirements. The majority of dually eligible beneficiaries are eligible for full Medicaid benefits, including long-term services and supports. Compared to all traditional Medicare beneficiaries in 2016, a significantly larger share of traditional Medicare beneficiaries with Medicaid had low incomes, reported their health status as fair or poor, were under age 65 and qualified for Medicare due to a disability, and were black (18%) or Hispanic (15%).
What is employer sponsored health insurance?
Employer-sponsored insurance provides retiree health coverage to 3 in 10 (30%) traditional Medicare beneficiaries in 2016, or nearly 10 million beneficiaries (not including 3.4 million beneficiaries who were enrolled in Medicare Advantage plans offered exclusively to employers’ or unions’ retirees and 2.0 million who had Medicare as a secondary payer). Compared to all traditional Medicare beneficiaries in 2016, those with employer-sponsored retiree coverage had relatively high incomes and higher education levels, and were disproportionately white (Table 1). Over time, the share of beneficiaries with employer-sponsored retiree coverage is expected to decline, because the share of large firms offering it to their employees has dropped over time.
How many people are on Medicare?
Today, 60 million people, including 51 million older adults and 9 million younger adults with disabilities, rely on Medicare for their health insurance coverage. Medicare beneficiaries can choose to get their Medicare benefits (Part A and Part B) through the traditional Medicare program, or they can enroll in a Medicare Advantage plan, such as a Medicare HMO or PPO. In 2018, two-thirds of Medicare beneficiaries are in traditional Medicare, and one-third are enrolled in Medicare Advantage plans.
Does Medicare cover Part A and Part B?
Medigap policies, sold by private insurance companies, fully or partially cover Part A and Part B cost-sharing requirements , including deductibles, copayments, and coinsurance. Compared to all traditional Medicare beneficiaries in 2016, those with Medigap had higher incomes and education levels, and were more likely to be white—similar to ...
Is Medicare a black or Hispanic?
Compared to all traditional Medicare beneficiaries in 2016, a significantly larger share of traditional Medicare beneficiaries with Medicaid had low incomes, reported their health status as fair or poor, were under age 65 and qualified for Medicare due to a disability, and were black (18%) or Hispanic (15%). No supplemental coverage.
What is Medicare Secondary Payer?
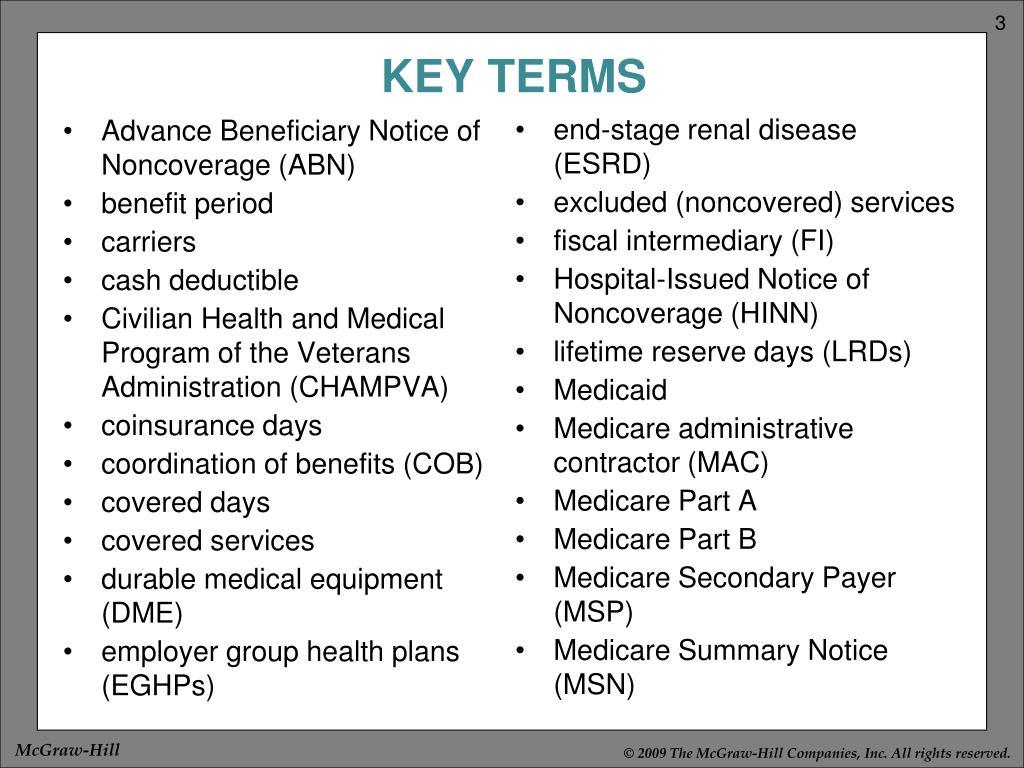
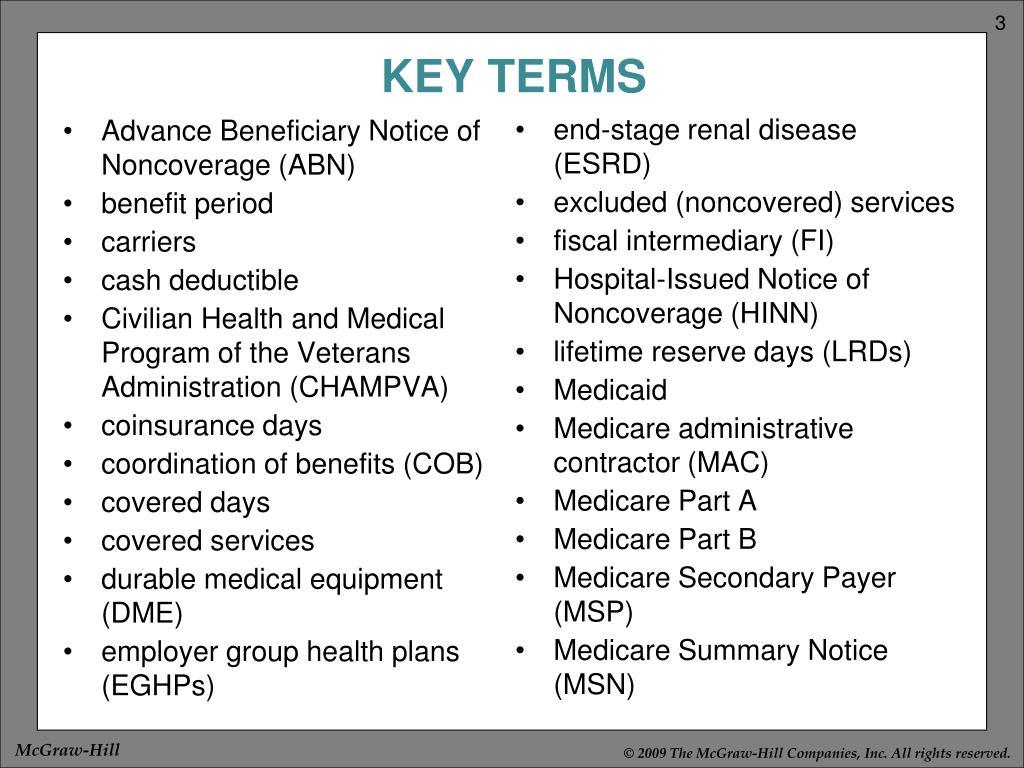
The Medicare Secondary Payer (MSP) program exists so that Medicare is not the primary payer of claims when individuals have certain other health insurance coverages. The Benefits Coordination & Recovery Center (BCRC) acts on behalf of Medicare to collect and manage information on other types of insurance or coverage a Medicare beneficiary may have.
What is the downside of having two insurance plans?
The downside of having two insurance plans (group and Medicare) is that you pay two sets of premiums and deductibles. Your secondary insurance will not pay toward your primary health insurance deductible, and it’s likely you will still have to pay out-of-pocket costs.
What is a COB?
Coordination of benefits (COB) is relevant for individuals with more than one primary payer. It is used to determine which insurance plan has the primary payment responsibility and the extent to which each plan covers an individual.
Who is the primary payer for Medicare?
Medicare is the primary payer for Medicare beneficiaries who are on employer plans if there are less than 20 employees. However, if the beneficiary is on an employer plan with 20 or more employees, that plan will serve as the primary payer,
What happens when Medicare beneficiaries have other health insurance?
When a Medicare beneficiary has other insurance (like employer group health coverage), rules dictate which payer is responsible for paying first. Please review the Reporting Other Health Insurance page for information on how and when to report other health plan coverage to CMS.
What is Medicare for seniors?
Medicare is a health insurance program designed to assist the nation's elderly to meet hospital, medical, and other health costs. Medicare is available to most individuals 65 years of age and older.
What is the CMS?
The Centers for Medicare & Medicaid Services (CMS) is the federal agency that manages Medicare. When a Medicare beneficiary has other health insurance or coverage, each type of coverage is called a "payer.". "Coordination of benefits" rules decide which one is the primary payer (i.e., which one pays first). To help ensure that claims are paid ...
How long does it take for Medicare to pay a claim?
When a Medicare beneficiary is involved in a no-fault, liability, or workers’ compensation case, his/her doctor or other provider may bill Medicare if the insurance company responsible for paying primary does not pay the claim promptly (usually within 120 days).
Does Medicare pay a conditional payment?
In these cases, Medicare may make a conditional payment to pay the bill. These payments are "conditional" because if the beneficiary receives an insurance or workers’ compensation settlement, judgment, award, or other payment, Medicare is entitled to be repaid for the items and services it paid.
How many Medicare beneficiaries have employer sponsored retirement?
Employer-sponsored Retiree Health Coverage. In total, 14.3 million of Medicare beneficiaries – a quarter (26%) Medicare beneficiaries overall — also had some form of employer-sponsored retiree health coverage in 2018. Of the total number of beneficiaries with retiree health coverage, nearly 10 million beneficiaries have retiree coverage ...
How is supplemental coverage determined?
Sources of supplemental coverage are determined based on the source of coverage held for the most months of Medicare enrollment in 2018. The analysis excludes beneficiaries who were enrolled in Part A only or Part B only for most of their Medicare enrollment in 2018 (n=4.7 million) and beneficiaries who had Medicare as a secondary payer ...
What is the age limit for Medigap?
Compared to all traditional Medicare beneficiaries in 2018, a larger share of Medigap policyholders had annual incomes greater than $40,000, had higher education levels, were disproportionately White, and were in excellent, very good, or good health ( Table 1 ). Only a small share of Medigap policyholders (2%) were under age 65 and qualified for Medicare due to having a long-term disability; most states do not require insurers to issue Medigap policies to beneficiaries under age 65. Federal law provides time-limited guarantee issue protections for adults ages 65 and older when they enroll in Medicare if they want to purchase a supplemental Medigap policy, but these protections do not extend to adults under the age of 65. Legislation has been introduced in the 117 th Congress to require insurers to offer Medigap coverage to younger adults with disabilities when they first go on Medicare, and to others.
What is Medicare Advantage?
Medicare Advantage plans provide all benefits covered by Medicare Parts A and B, often provide supplemental benefits, such as dental and vision, and typically provide the Part D prescription drug benefit. Many traditional Medicare beneficiaries also rely on other sources of coverage to supplement their Medicare benefits.
How many people are covered by Medicare?
More than 62 million people, including 54 million older adults and 8 million younger adults with disabilities, rely on Medicare for their health insurance coverage. Medicare beneficiaries can choose to get their Medicare benefits (Part A and Part B) through the traditional Medicare program, or they can enroll in a Medicare Advantage plan, such as a Medicare HMO or PPO. Medicare Advantage plans provide all benefits covered by Medicare Parts A and B, often provide supplemental benefits, such as dental and vision, and typically provide the Part D prescription drug benefit. Many traditional Medicare beneficiaries also rely on other sources of coverage to supplement their Medicare benefits. Supplemental insurance coverage typically covers some or all of Medicare Part A and Part B cost-sharing requirements and, in some instances, provides benefits not otherwise covered by Medicare. Beneficiaries can also enroll in a Part D plan for prescription drug coverage, either a stand-alone plan to supplement traditional Medicare or a Medicare Advantage plan that covers drugs.
Does Medicare have supplemental coverage?
No Supplemental Coverage. In 2018, 5.6 million Medicare beneficiaries in traditional Medicare– 1 in 10 beneficiaries overall (10%) or nearly 1 in 5 of those with traditional Medicare (17%) had no source of supplemental coverage. Beneficiaries in traditional Medicare with no supplemental coverage are fully exposed to Medicare’s cost-sharing ...
Can dual eligible beneficiaries get full medicaid?
The majority of dual-eligible beneficiaries are eligible for full Medicaid benefits, including long-term services and supports. Other dual-eligible beneficiaries may qualify for Medicare premium and cost-sharing assistance through the Medicare Savings Programs, but not full Medicaid benefits, if they meet an income and asset test. Previous KFF analysis has shown that expanding eligibility for the Medicare Savings Program to provide both premium and cost-sharing assistance to beneficiaries with incomes up to 150% FPL and eliminating the asset limits would cover an additional 5.2 million beneficiaries.
How long do you have to enroll in Part B?
There are two main times when you can enroll in part B when you are over 65 and covered by your employer’s insurance: 1 While your work coverage is still active 2 During the eight month period after your employer-based coverage ends or the employment ends, whichever occurs first.
What is the phone number for Medicare?
If you have an urgent matter or need enrollment assistance, call us at 800-930-7956. By submitting your question here, you agree that a licensed sales representative may respond to you about Medicare Advantage, Prescription Drug, and Medicare Supplement Insurance plans.
Does Medicare Part B start at the same time?
That way you can time it that when your work coverage ends, your Medicare Part B (and any supplemental or drug coverage you may purchase) all start at the same time. You should not have a gap when your work coverage has ended but your Medicare has yet to begin.
Can seniors over 65 delay Medicare?
Senior65 generally recommends those over 65 delay enrolling in Medicare Part B if they are offered coverage through work (including spouse’s work). We all want to stay clear of paying Medicare late-enrollment penalties while avoiding gaps in coverage. This is where Senior65 comes in to make sense of it all.
Does Senior65 sell your information?
Senior65 believes in your privacy. We will not sell your personal information. This is a solicitation for insurance.