Full Answer
How to get prescription drug coverage from Medicare?
How to get prescription drug coverage 1 There are 2 ways to get Medicare drug coverage: Medicare drug plans. ... 2 Consider all your drug coverage choices. Before you make a decision, learn how prescription drug coverage works with your other drug coverage. 3 Joining a Medicare drug plan may affect your Medicare Advantage Plan. ...
How many drugs do Medicare Advantage plans cover?
Consult this list of 300 drugs that some Medicare Advantage plans and Medicare Part D prescription drug plans may or may not cover.
What changes can Medicare make to prescription drug coverage?
Medicare prescription drug plans can make the following changes to prescription drug coverage: First, Medicare can stop covering a medication and drop it from its formulary (a list of drugs the plan will cover, broken into tiers).
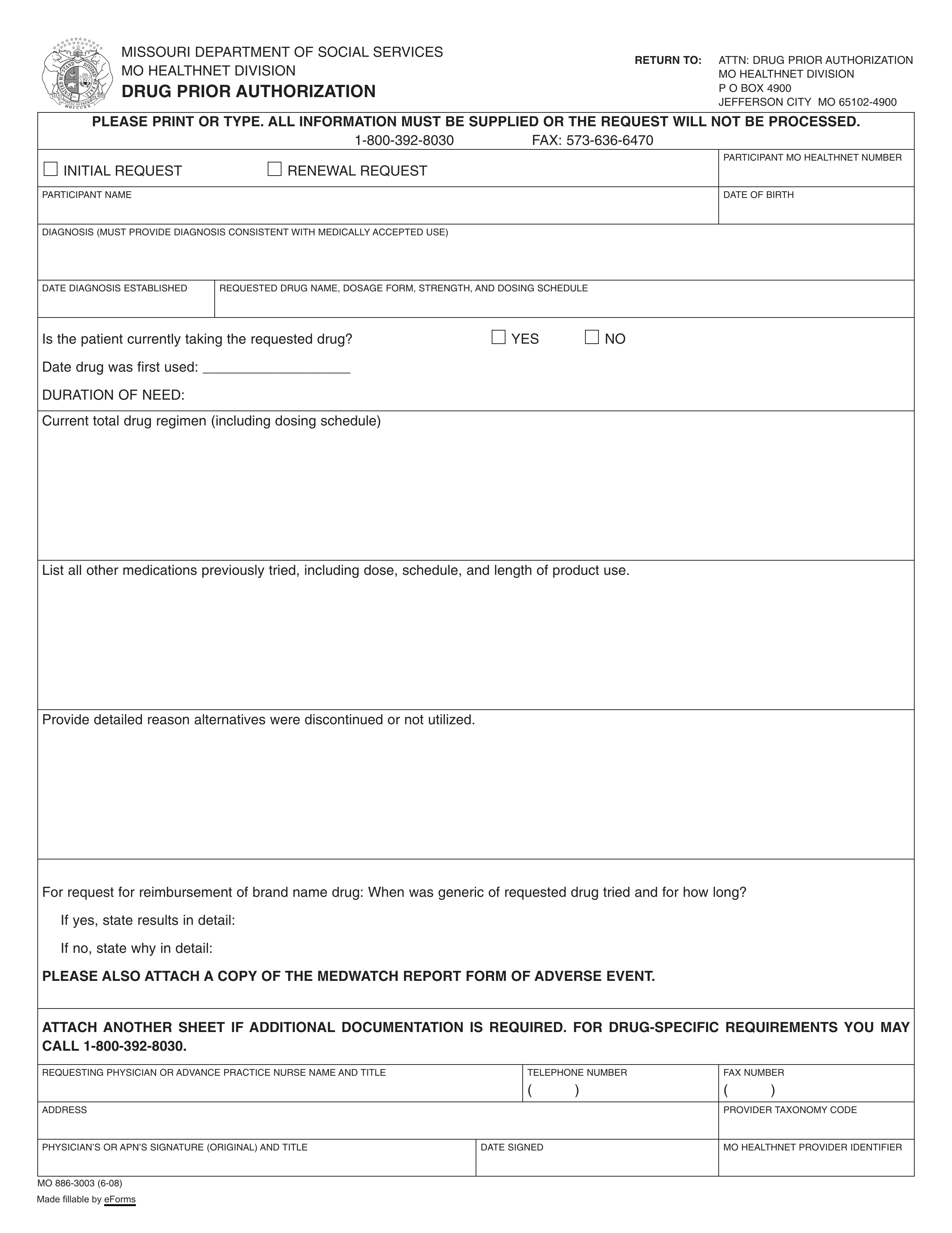
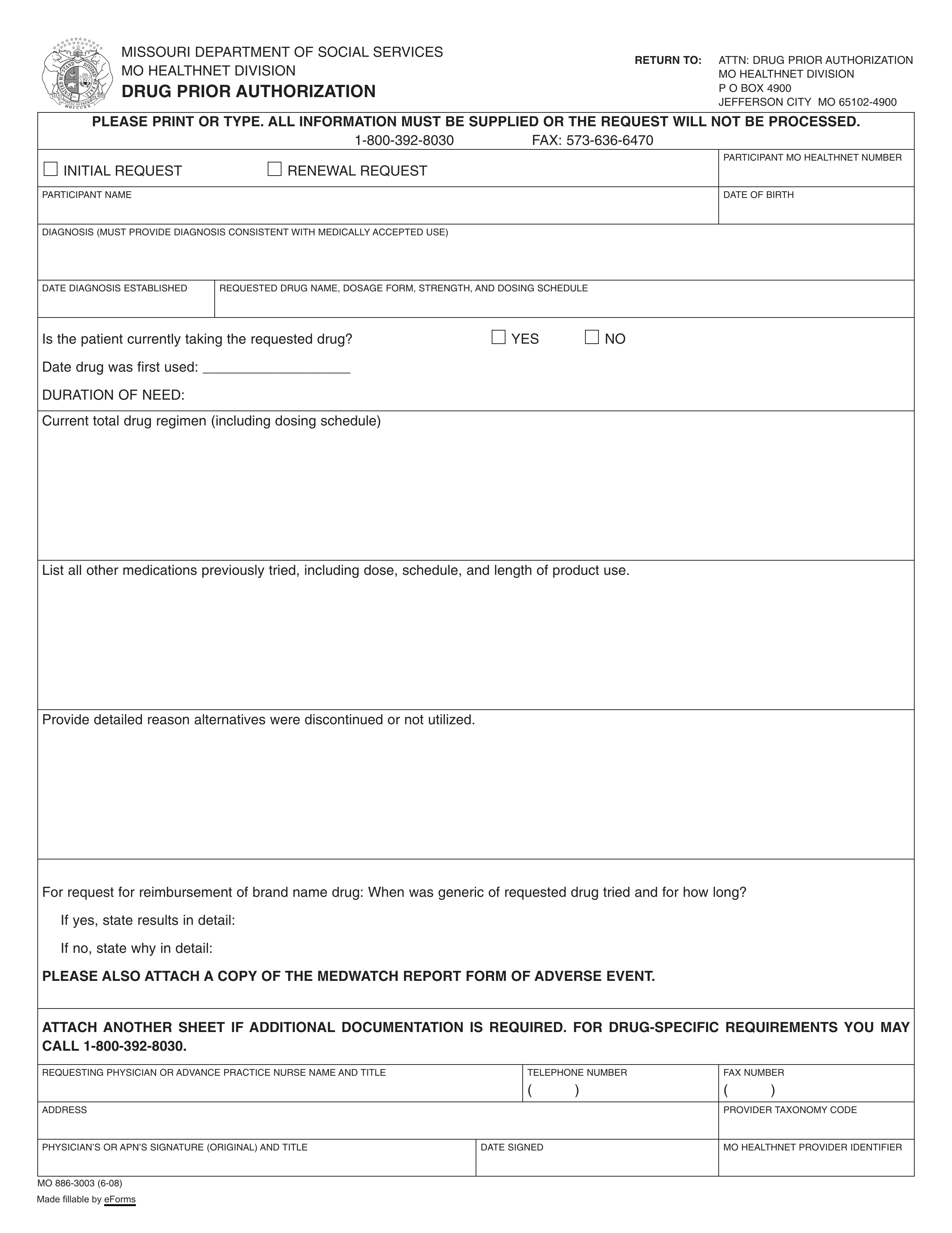
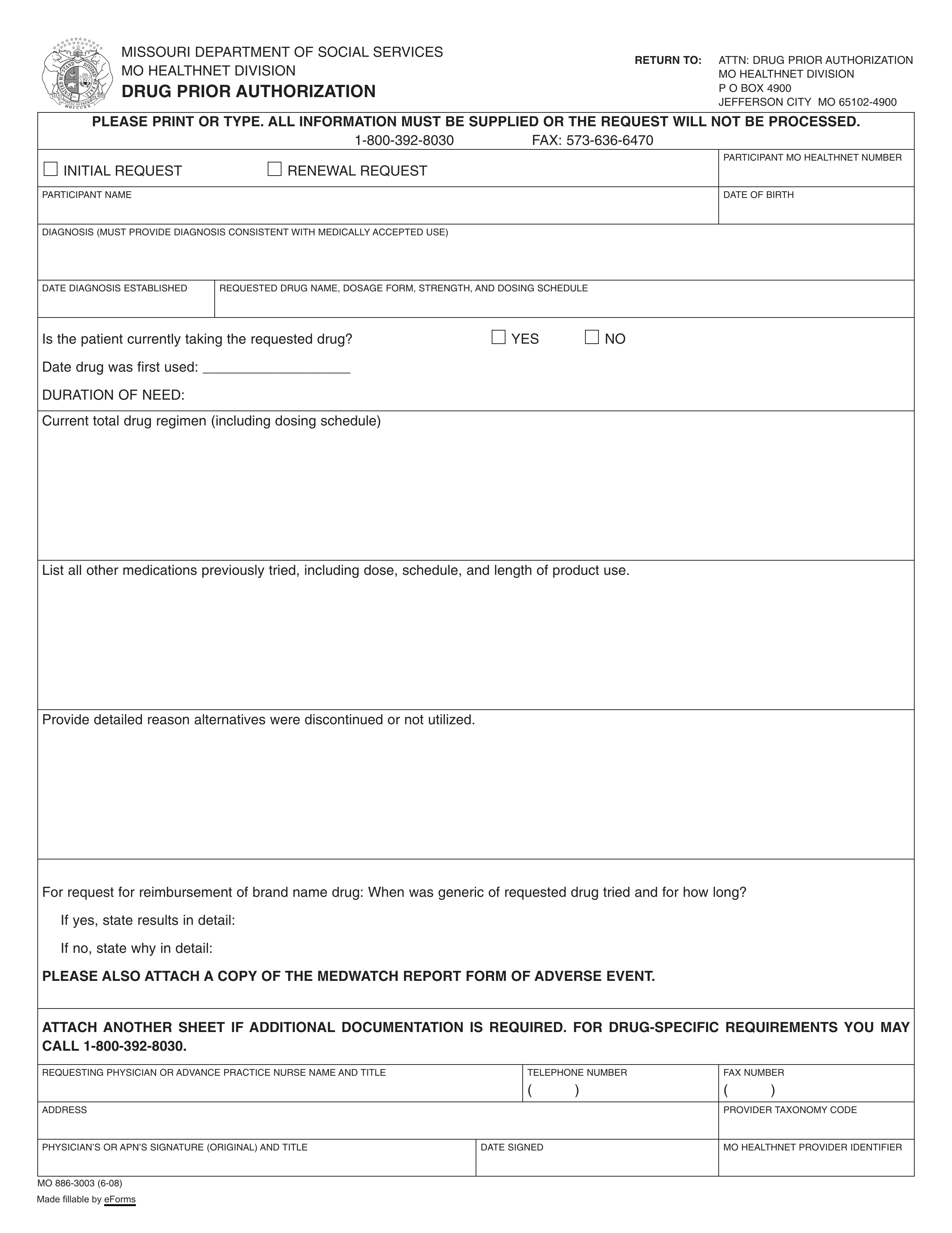
What is prior authorization for Medicare drug plans?
Approval that you must get from a Medicare drug plan before you fill your prescription in order for the prescription to be covered by your plan. Your Medicare drug plan may require prior authorization for certain drugs. . In most cases, you must first try a certain, less expensive drug on the plan’s
How long is a prescription good for Medicare?
To ensure that an item is still medically necessary, the delivery date/date of service must be within 3 months from the "Initial Date" of the CMN or DIF or 3 months from the date of the physician's signature.
What are the 4 phases of Medicare Part D coverage?
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.
Does Medicare Part D expire?
If your Medicare Advantage or Part D plan is ending at the close of the year, it is important to understand how you are affected and actions you should take to ensure you have needed coverage. If your plan is ending, it should send you a letter in early October explaining that it will no longer be available next year.
Do Medicare drug plans automatically renew?
Like Medicare Advantage, your Medicare Part D (prescription drug) plan should automatically renew. Exceptions would be if Medicare does not renew the contract with your insurance company or the company no longer offers the plan.
How do I avoid the Medicare Part D donut hole?
If you have limited income and resources, you may want to see if you qualify to receive Medicare's Extra Help/Part D Low-Income Subsidy. People with Extra Help see significant savings on their drug plans and medications at the pharmacy, and do not fall into the donut hole.
What is the Doughnut hole for 2021?
For 2021, the coverage gap begins when the total amount your plan has paid for your drugs reaches $4,130 (up from $4,020 in 2020). At that point, you're in the doughnut hole, where you'll now receive a 75% discount on both brand-name and generic drugs.
Do I need to renew my Medicare Supplement every year?
The plain and simple answer to this question is no, you don't have to renew your Medigap plan each year. All Medicare Supplement plans are guaranteed renewable for life as long as you're paying your premium, either monthly, quarterly, semi-annually, or annually.
What is the main problem with Medicare Part D?
The real problem with Medicare Part D plans is that they weren't set up with the intent of benefiting seniors. They were set up to benefit: –Pharmacies, by having copays for generic medications that are often far more than the actual cost of most of the medications.
Why was my Medicare Part D Cancelled?
Why was my Medicare plan coverage cancelled? Your Medicare Part D prescription drug plan (PDP) or Medicare Advantage plan (MA, MAPD, or SNP) coverage can be cancelled because of changes to the Medicare plan or because of something that you have done (or not done).
Can you switch Medicare Part D plans anytime?
You can change from one Part D plan to another during the Medicare open enrollment period, which runs from October 15 to December 7 each year. During this period, you can change plans as many times as you want.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
Can I add Part D to my Medicare at any time?
Keep in mind, you can enroll only during certain times: Initial enrollment period, the seven-month period that begins on the first day of the month three months before the month you turn 65 and lasts for three months after the birthday month.
How long does Medicare cover after kidney transplant?
If you're entitled to Medicare only because of ESRD, your Medicare coverage ends 36 months after the month of the kidney transplant. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage. Transplant drugs can be very costly.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
What is Medicare Part A?
Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage. Transplant drugs can be very costly. If you’re worried about paying for them after your Medicare coverage ends, talk to your doctor, nurse, or social worker.
What happens if you get a drug that Part B doesn't cover?
If you get drugs that Part B doesn’t cover in a hospital outpatient setting, you pay 100% for the drugs, unless you have Medicare drug coverage (Part D) or other drug coverage. In that case, what you pay depends on whether your drug plan covers the drug, and whether the hospital is in your plan’s network. Contact your plan to find out ...
What is Part B covered by Medicare?
Here are some examples of drugs Part B covers: Drugs used with an item of durable medical equipment (DME) : Medicare covers drugs infused through DME, like an infusion pump or a nebulizer, if the drug used with the pump is reasonable and necessary.
Does Medicare cover transplant drugs?
Medicare covers transplant drug therapy if Medicare helped pay for your organ transplant. Part D covers transplant drugs that Part B doesn't cover. If you have ESRD and Original Medicare, you may join a Medicare drug plan.
Does Part B cover drugs?
covers drugs Part B doesn't cover. If you have drug coverage, check your plan's. A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list. to see what outpatient drugs it covers.
How to get prescription drug coverage
Find out how to get Medicare drug coverage. Learn about Medicare drug plans (Part D), Medicare Advantage Plans, more. Get the right Medicare drug plan for you.
What Medicare Part D drug plans cover
Overview of what Medicare drug plans cover. Learn about formularies, tiers of coverage, name brand and generic drug coverage. Official Medicare site.
How Part D works with other insurance
Learn about how Medicare Part D (drug coverage) works with other coverage, like employer or union health coverage.
Are there any changes to the cost-sharing structure of Medicare Part D programs?
Because Medicare is a federally administered program, the program’s cost-sharing structure (how much enrollees pay out of pocket) is subject to changes per federal policy. This year, there is another adjustment to the standard benefit, and, in 2022, Medicare will continue to offer plans that cap insulin costs at $35 for a month’s supply.
What are the ways that Medicare Part D plans can change drug coverage from year to year?
Medicare prescription drug plans can make the following changes to prescription drug coverage:
How will Medicare Part D coverage change in 2022?
GoodRx Research analyzed the publicly available Medicare prescription drug plan data to evaluate any changes to plan coverage in the upcoming year. In 2022, there are over 5,300 plans, 85% of which are Medicare Advantage plans. However, this doesn’t mean people have all plans available to them.
Summing it up
GoodRx Research finds that Medicare prescription drug plans have minimal drug coverage changes from 2021 to 2022. However, it is good practice to reevaluate the prescription drug plan that you’re in for 2022, especially before the end of open enrollment on December 7, 2021.
How long can you have opioids on Medicare?
First prescription fills for opioids. You may be limited to a 7-day supply or less if you haven’t recently taken opioids. Use of opioids and benzodiazepines at the same time.
What happens if a pharmacy doesn't fill a prescription?
If your pharmacy can’t fill your prescription as written, the pharmacist will give you a notice explaining how you or your doctor can call or write to your plan to ask for a coverage decision. If your health requires it, you can ask the plan for a fast coverage decision.
Does Medicare cover opioid pain?
There also may be other pain treatment options available that Medicare doesn’t cover. Tell your doctor if you have a history of depression, substance abuse, childhood trauma or other health and/or personal issues that could make opioid use more dangerous for you. Never take more opioids than prescribed.
Do you have to talk to your doctor before filling a prescription?
In some cases, the Medicare drug plan or pharmacist may need to first talk to your doctor before the prescription can be filled. Your drug plan or pharmacist may do a safety review when you fill a prescription if you: Take potentially unsafe opioid amounts as determined by the drug plan or pharmacist. Take opioids with benzodiazepines like Xanax®, ...
Does Medicare cover prescription drugs?
In most cases, the prescription drugs you get in a Hospital outpatient setting, like an emergency department or during observation services , aren't covered by Medicare Part B (Medical Insurance). These are sometimes called "self-administered drugs" that you would normally take on your own. Your Medicare drug plan may cover these drugs under certain circumstances.
Does Medicare require prior authorization?
Your Medicare drug plan may require prior authorization for certain drugs. . In most cases, you must first try a certain, less expensive drug on the plan’s. A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list.
Does Medicare cover self administered drugs?
Your Medicare drug plan may cover these drugs under certain circumstances. You'll likely need to pay out-of-pocket for these drugs and submit a claim to your drug plan for a refund. Or, if you get a bill for self-administered drugs you got in a doctor's office, call your Medicare drug plan for more information.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
How to enroll in Medicare?
Enroll on the Medicare Plan Finder or on the plan's website. Complete a paper enrollment form. Call the plan. Call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. When you join a Medicare drug plan, you'll give your Medicare Number and the date your Part A and/or Part B coverage started.
What are the different types of Medicare plans?
You can only join a separate Medicare drug plan without losing your current health coverage when you’re in a: 1 Private Fee-for-Service Plan 2 Medical Savings Account Plan 3 Cost Plan 4 Certain employer-sponsored Medicare health plans
What happens if you don't get prescription drug coverage?
If you decide not to get it when you’re first eligible, and you don’t have other creditable prescription drug coverage (like drug coverage from an employer or union) or get Extra Help, you’ll likely pay a late enrollment penalty if you join a plan later.
What is a PACE plan?
Programs of All-inclusive Care for the Elderly (PACE) organizations are special types of Medicare health plans. PACE plans can be offered by public or private companies and provide Part D and other benefits in addition to Part A and Part B benefits. with drug coverage.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Do you have to have Part A and Part B to get Medicare?
You get all of your Part A, Part B, and drug coverage, through these plans. Remember, you must have Part A and Part B to join a Medicare Advantage Plan , and not all of these plans offer drug coverage. Visit Medicare.gov/plan-compare to get specific Medicare drug plan and Medicare Advantage Plan costs, and call the plans you’re interested in ...
How long can you get a refill in Medicare?
During the COVID-19 pandemic, Medicare drug plans must relax their “refill-too-soon” policy. Plans must let you get up to a 90-day supply in one fill unless quantities are more limited for safety reasons.
How long can you get extended supply of prescription drugs?
If you think you won't return home for a long time, you may want to get an extended-day supply (a 60- to 90-day supply ) of your drugs. Ask your Medicare drug plan whether it offers extended-day supplies and which pharmacies you can use to get them. For more information on getting prescription drugs during an emergency or disaster, ...
What to do if you have a Medicare drug plan?
If you have a Medicare drug plan and your state has issued a warning of a possible emergency or disaster: If you're not able to go to your usual network pharmacy to replace your prescription drugs, contact your Medicare drug plan to find another network pharmacy nearby.
How to get a refund from Medicare?
To get a refund from your Medicare drug plan, submit a paper claim. Ask your plan where to send your claim. If you paid full cost for the drugs, save your receipts so you can ask your Medicare drug plan if it'll refund you for your costs. You won't get a refund for the out-of-network cost-sharing amount.
Can Medicare cover prescriptions?
In some Medicare plans, your prescriptions are only covered if you get them filled at network pharmacies. Contact your Medicare drug plan if you had to leave your home without your drugs, or your drugs have been damaged or lost because of the emergency or disaster. They can help you find another network pharmacy.
Can you move prescriptions from one pharmacy to another?
Using in-network pharmacies. You'll be able to move most prescriptions from one network pharmacy to another, and back to your regular pharmacy when the emergency or disaster ends. If you need help finding the closest network pharmacy, contact your Medicare drug plan.