When to use CPT code 98940 instead of 98941?
Dec 06, 2018 · I am New to Chiropractic billing and the provider is receiving denials for his established E/M visits when billed with a 98941-98942. New patient visits are paid with no issues, correct -25 modifier is being used, separate and billable diagnosis are used.
Does Medicare cover chiropractic adjustments CPT 98943?
Mar 19, 2019 · Claims submitted for Chiropractic Manipulative Treatment (CMT) CPT codes 98940, 98941, or 98942, (found in Group 1 codes under CPT/HCPCS Codes) must contain an AT modifier or they will be considered not medically necessary. Utilization Guidelines. Payment is to the billing Chiropractor and is based on the physician fee schedule.
How much is CPT code 99213 for Medicare?
• Codes for spinal manipulations (98940 – 98942) are specific to the number of regions treated. If only two regions are treated, 98940 should be used instead of 98941–52. Claims submitted for CPT code 98940, 98941, or 98942 with the demonstration code “demo 45” shall be rejected.
How many times do you need to code 98943?
99214. 25 minutes. $110.43. 99215. 40 minutes. $148.33. ( Source) Other Medicare rates for CPT code 99213 are $81.62, in WA in King County, so it depends on the locality. Source.
Does code 98943 require a modifier?
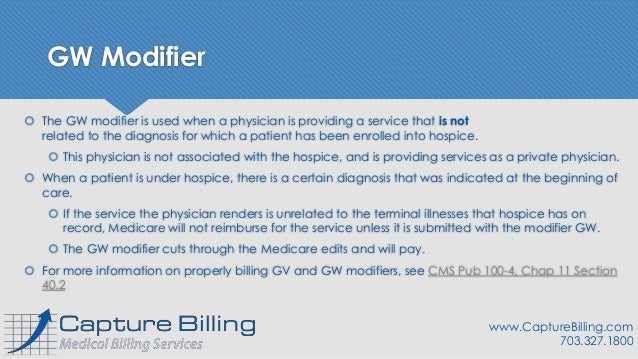
The “AT” modifier distinguishes active/corrective treatment from maintenance therapy. The AT modifier should be appended to the chiropractic manipulation (98940-98943) to show active treatment. The absence of the AT modifier would indicate maintenance or palliative care.
Does 98941 need a modifier?
When providing maintenance therapy, no modifier is required when billing procedure codes 98940, 98941, or 98942. The AT modifier must not be placed on the claim when maintenance therapy has been provided. Claims without the AT modifier will be considered as maintenance therapy and denied.
Does Medicare cover 98943?
Medicare does not cover chiropractic treatments to extraspinal regions (CPT 98943), which includes the head, upper and lower extremities, rib cage, and abdomen.
What does CPT code 98941 include?
CPT Code 98941 Chiropractic manipulative treatment (CMT); Spinal, 3-4 regions. CPT Code 98942 Chiropractic manipulative treatment (CMT); Spinal, 5 regions. CPT Code 98943 Chiropractic manipulative treatment (CMT); Extraspinal, 1 or more regions.May 18, 2020
Is 98941 covered by Medicare?
Diagnosis Code Description Medicare Covered Chiropractic Services If the CPT code is 98940, 98941, or 98942 and is billed with one of the following primary diagnosis codes and with modifier AT, then the chiropractic service is covered.
Is 97012 covered by Medicare?
There is insufficient scientific data to support the benefits of this technique. Therefore, non-surgical spinal decompression is not covered by Medicare (CMS Publication 100-03, Medicare National Coverage Determinations (NCD) Manual: Section 160.16).
What does CPT code 98943 mean?
Chiropractic Manipulative Treatment ProceduresCPT® 98943, Under Chiropractic Manipulative Treatment Procedures. The Current Procedural Terminology (CPT®) code 98943 as maintained by American Medical Association, is a medical procedural code under the range - Chiropractic Manipulative Treatment Procedures.
What is modifier 25 in CPT coding?
Evaluation and ManagementThe Current Procedural Terminology (CPT) definition of Modifier 25 is as follows: Modifier 25 – this Modifier is used to report an Evaluation and Management (E/M) service on a day when another service was provided to the patient by the same physician or other qualified health care professional.
What CPT codes can an acupuncturist bill?
Bill a new patient for their first acupuncture visit using CPT codes 99201 to 99204. E/M services can be billed for periodic follow-up evaluations (every 30 days or every sixth visit using CPT codes 99211 – 99214) with established acupuncture patients.Jul 29, 2021
What is the code 99213?
CPT® code 99213: Established patient office or other outpatient visit, 20-29 minutes.
Does 97012 need a modifier?
Whether it's 97012 or 97140, by appending the 59 modifier, you will ensure that you receive reimbursement for both services.Jun 28, 2019
What are chiropractic modifiers?
Modifiers are referred to as level one modifiers that are used to supplement information about a claim. By example, you're all familiar with like using modifier 25. It's there to tell them that the exam is separate. So really modifiers, just do additional things to allow us to know something about the code.Jun 11, 2021
What is CMT 98940?
98940 – Chiropractic manipulative treatment (CMT); spinal, one or two regions. Documentation must include a validated diagnosis for one or two spinal regions and support that manipulative treatment occurred in one to two regions of the spine (region as defined by CPT). – average fee payment-$20 – $30
What is the ICD-9 code for CPT?
All ICD-9-CM diagnosis codes and CPT treatment and procedure codes must be validated in the patient chart and coordinated as to the diagnoses and treatment code descriptors. A valid diagnosis is the most appropriate I CD-9-CM code that is supported by subjective symptoms, physical findings, and diagnostic testing/imaging (if appropriate)…
How to check status of Palmetto GBA claim?
You can determine the status of a claim through the Palmetto GBA eServices tool or by calling the Palmetto GBA Interactive Voice Response (IVR) unit.
What is an x-ray test?
For example, an x-ray or any diagnostic test taken for the purpose of determining or demonstrating the existence of a subluxation of the spine is a diagnostic x-ray test covered under 1861 (s) (3) of the Act if ordered , taken , and interpreted by a physician who is a doctor of medicine or osteopathy.
What is correction in medical terms?
The word “correction” may be used in lieu of “treatment.”. Also, a number of different terms composed of the following words may be used to describe manual manipulation as defined above: – Spine or spinal adjustment by manual means; – Spine or spinal manipulation; – Manual adjustment; and.
What is subluxation in spine?
Subluxation is defined as a motion segment, in which alignment, movement integrity, and/or physiological function of the spine are altered although contact between joint surfaces remains intact. A subluxation may be demonstrated by an x-ray or by physical examination, as described below. 1. Demonstrated by X-Ray.
What is acute subluxation?
Acute subluxation – A patient’s condition is considered acute when the patient is being treated for a new injury, identified by x-ray or physical exam as specified above. The result of chiropractic manipulation is expected to be an improvement in, or arrest of progression, of the patient’s condition.
What are the components of a medical record?
Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components to be present in the medical record: 1 An expanded problem focused history 2 An expanded problem focused examination 3 Medical decision making of low complexity
How much does Medicare pay?
These rates are adjusted by Medicare. Some insurance companies only pay 15% over the Medicaid rate in their state, whereas others pay 45%, 60%, 80%, 85% on top of their state’s medicaid rate. You can see these rates vary across insurance companies.
How long does a physician spend with a patient?
Physicians typically spend 15 minutes face-to-face with the patient and/or family. A tip for code 99213 is to think of expanded visits as a sum of the continued symptoms or another extended form of the problem.
What is an office visit?
Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components to be present in the medical record:
What is BCBS denial?
According to recent reports, chiropractic practices received denials from Blue Cross and Blue Shield (BCBS) for claims billed with modifiers. Medical billing outsourcing companies that provide chiropractic billing services found that most of the claims denied were those that required the 25 and 59 modifiers. The Explanation of Benefits (EOBs) indicated that the modifiers were used inappropriately or utilization of the modifier was higher than average. In December 2017, the Illinois Chiropractic Society (ICS) reported that in the cases they reviewed, the procedure code and modifiers were billed correctly based on the claims information, but that the denials are the result of a new code-editing feature that BCBS announced to all provider types.
What is NCCI modifier?
The National Correct Coding Initiative (NCCI) edit program developed by the Centers for Medicare and Medicaid Services (CMS) is used by carriers and third party administrators in an effort to prevent improper payment when certain codes are submitted together. Modifier 59 and some other modifiers are exceptions to the NCCI PTP (procedure-to-procedure) edits.
How long is manual therapy?
For e.g., manual therapy might be performed for 10 minutes, followed by 15 minutes of therapeutic activities, followed by another 5 minutes of manual therapy . CPT code 97530 should not be reported and modifier 59 should not be used if the two procedures are performed during the same time block. The bottom line:
What is CMT in chiropractic?
Answer: Chiropractic manipulative treatment (CMT) is a form of manual treatment to influence joint and neurophysiological function. This treatment may be accomplished using a variety of techniques. The chiropractic manipulative treatment codes include a pre-manipulation patient assessment.
What are the five regions of the spine?
For purposes of CMT, the five spinal regions referred to are: cervical region (includes atlanto-occipital joint); thoracic region (includes costovertebral and costotransverse joints); lumbar region ; sacral region ;
What is CPT code 98943?
Since CPT Code 98943 (which is chiropractic adjustment to the extremities) is a procedure performed by exclusively by chiropractors, there seems to be some misunderstandings and misinterpretation of proper coding rules when it comes to getting paid.
Can Medicare cover 98943?
A perfect example here is Medicare. There’s basically no good reason that Medicare does not cover the 98943 adjustment, other than it’s not in their policy! You can fight it if that’s your bent or just steer around the issue because you know it’s there.
Is 98943 a bundled CPT?
Bundling Assumptions – many chiropractors (and some payers) assume 98943 is not a separately payable service and that it is simply included (bundled) in with their spinal adjustment codes (98940-98942). While it is true that Medicare does not reimburse CPT code 98943, most other payers do.
