Do not use special characters, (dollar signs, decimals, dashes, asterisk, or backslashes) unless otherwise specified. Use an ink jet or laser printer to complete the CMS-1500 claim form. Because claims submitted with dot matrix printers have breaks in the letters and numbers, OCR equipment is unable to properly read these claims.
Full Answer
How does the Medicare contractor notify the CMS Central Office?
1) The Medicare contractor shall send notification to the CMS Central Office (not the hospital), via email to [email protected] and regional office that a hospital has met the criteria for reconciliation.
What is the CMS questionnaire for Medicare?
The CMS Questionnaire should be used to determine the primary payer of the beneficiary’s claims. This questionnaire consists of six parts and lists questions to ask Medicare beneficiaries.
Can CMS Direct Medicare contractors to use an alternative CCR?
Effective August 8, 2003, the CMS Central Office may direct Medicare contractors to use an alternative CCR if CMS believes this will result in a more accurate CCR.
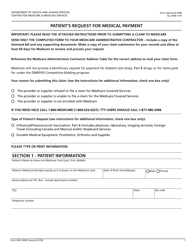
How to fill out the CMS 1500 form?
Instructions on how to fill out the CMS 1500 Form Item Instructions Item 1 Type of Health Insurance Coverage Applicable to the Claim Show the type of health insurance coverage applicable to this claim by checking the appropriate box, e.g., if a Medicare claim is being filed, check the Medicare box. Item 1a Insured’s ID Number
How do I fill out a CMS 1500 for Medicare?
14:5319:58How-to Accurately Fill Out the CMS 1500 Form for Faster PaymentYouTubeStart of suggested clipEnd of suggested clipField 1 is the very first field on the CMS 1500 form and it tells the insurance carrier the categoryMoreField 1 is the very first field on the CMS 1500 form and it tells the insurance carrier the category of insurance that the policy falls into. It can be left blank.
What goes in box 17a on CMS 1500?
Item 17a – Enter the ID qualifier 1G, followed by the CMS assigned UPIN of the referring/ordering physician listed in item 17. The UPIN may be reported on the Form CMS-1500 until May 22, 2007, and MUST be reported if an NPI is not available.
When entering the patient's name on the CMS 1500 claim form what punctuation should be used?
Patient names are entered onto the claim form with last name, first name, middle initial separated by commas. When entering professional names which of the following guidelines should be followed on Item 2 on the CMS-1500 claim form?
How do I bill a claim to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What goes in box 23 on a CMS-1500?
Box 23 is used to show the payer assigned number authorizing the service(s).
What is a qualifier in box 17?
What is it? Box 17 identifies the name of the referring provider on the claim. Enter the applicable qualifier to the left of the vertical dotted line to identify which provider is being reported.
What is the only form of punctuation allowed on a CMS 1500?
Is punctuation allowed on the CMS-1500? The only form of punctuation allowed on a CMS-1500 is a comma, or unique punctuation in a patient's name.
How are the line items sequenced on the claim form?
They are sequenced by revenue code in ascending numerical order. What is the purpose of the standard CMS-1500 claim form? On the CMS-1500 form, which item number identifies the prior authorization or referral number?
When entering professional names which of the following guidelines should be followed on item 2 on the CMS 1500 claim form?
When entering professional names, which of the following guidelines should be followed on item 2 on the CMS 1500 claim form? Patient names are entered onto the claim form with last name, first name, middle initial separated by commas.
Does Medicare accept the CMS-1500 claim form?
Medicare will accept any Page 3 type (i.e., single sheet, snap-out, continuous feed, etc.) of the CMS-1500 claim form for processing. To purchase forms from the U.S. Government Printing Office, call (202) 512-1800. The following instructions are required for a Medicare claim.
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
Can patient bill Medicare directly?
If you see a participating doctor, they handle Medicare billing, and you don't have to file any claim forms. However, certain doctors don't bill Medicare directly. If you want Medicare to pay for your care, you'll need to send a form to request reimbursement.
What qualifier should be listed in block 17 for a referring provider?
The qualifiers appropriate for identifying an ordering, referring, or supervising role are as follows: • DN -- referring provider • DK -- ordering provider • DQ -- supervising provider • Enter the qualifier to the left of the dotted vertical line on item 17.
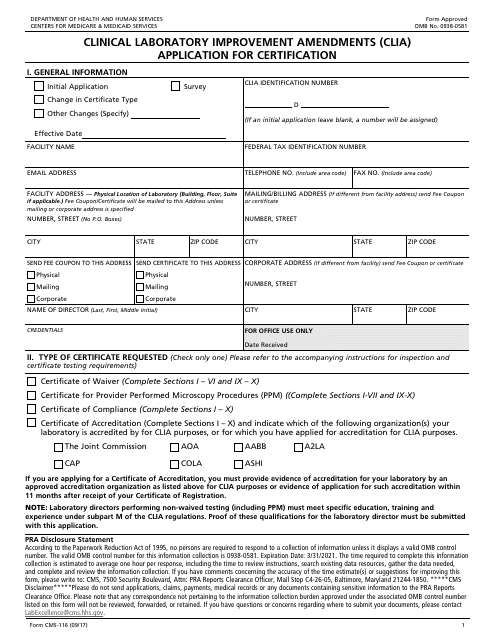
What box does the CLIA number go in on a CMS-1500?
item 23On each claim, the CLIA number of the laboratory that is actually performing the testing must be reported in item 23 on the CMS-1500 form.
What is authorization in medical billing?
Authorization in medical billing refers to the process wherein the payer authorizes to cover the prescribed services before the services are rendered. This is also termed as pre-authorization or prior authorization services.
How many boxes are there in cms1500?
There are 33 boxes in a CMS-1500 form. All of these boxes must be filled for the insurance claim to pass through.
What is Medicare claim processing manual?
The Medicare Claims Processing Manual (Internet-Only Manual [IOM] Pub. 100-04) includes instructions on claim submission. Chapter 1 includes general billing requirements for various health care professionals and suppliers. Other chapters offer claims submission information specific to a health care professional or supplier type. Once in IOM Pub. 100-04, look for a chapter(s) applicable to your health care professional or supplier type and then search within the chapter for claims submission guidelines. For example, Chapter 20 is the Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS).
What is MSP in Medicare?
MSP provisions apply to situations when Medicare isn’t the patient’s primary health insurance coverage.MSP provisions ensure Medicare doesn’t pay for services and items that pertain to other health insurance or coverage that’s primarily responsible for paying. For more information, refer to the Medicare Secondary Payer
What is the 837P form?
This booklet offers education for health care administrators, medical coders, billing and claims processing personnel, and other medical administrative staff who are responsible for submitting Medicare professional and supplier claims for Medicare payment using the 837P or Form CMS-1500.
What is the 10th revision of the ICd 10?
The International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM),is used to code diagnostic information on claims. Visit the Centers for Disease Control and Prevention website to access ICD-10-CM codes electronically or you may purchase hard copy code books from code book publishers.
When do hospitals report Medicare beneficiaries?
If the beneficiary is a dependent under his/her spouse's group health insurance and the spouse retired prior to the beneficiary's Medicare Part A entitlement date, hospitals report the beneficiary's Medicare entitlement date as his/her retirement date.
What is secondary payer?
Medicare is the Secondary Payer when Beneficiaries are: 1 Treated for a work-related injury or illness. Medicare may pay conditionally for services received for a work-related illness or injury in cases where payment from the state workers’ compensation (WC) insurance is not expected within 120 days. This conditional payment is subject to recovery by Medicare after a WC settlement has been reached. If WC denies a claim or a portion of a claim, the claim can be filed with Medicare for consideration of payment. 2 Treated for an illness or injury caused by an accident, and liability and/or no-fault insurance will cover the medical expenses as the primary payer. 3 Covered under their own employer’s or a spouse’s employer’s group health plan (GHP). 4 Disabled with coverage under a large group health plan (LGHP). 5 Afflicted with permanent kidney failure (End-Stage Renal Disease) and are within the 30-month coordination period. See ESRD link in the Related Links section below for more information. Note: For more information on when Medicare is the Secondary Payer, click the Medicare Secondary Payer link in the Related Links section below.
Does Medicare pay for black lung?
Federal Black Lung Benefits - Medicare does not pay for services covered under the Federal Black Lung Program. However, if a Medicare-eligible patient has an illness or injury not related to black lung, the patient may submit a claim to Medicare. For further information, contact the Federal Black Lung Program at 1-800-638-7072.
Does Medicare pay for the same services as the VA?
Veteran’s Administration (VA) Benefits - Medicare does not pay for the same services covered by VA benefits.
Is Medicare a primary or secondary payer?
Providers must determine if Medicare is the primary or secondary payer; therefore, the beneficiary must be queried about other possible coverage that may be primary to Medicare. Failure to maintain a system of identifying other payers is viewed as a violation of the provider agreement with Medicare.
What is the word "none" in Medicare?
If the insured reports a terminating event with regard to insurance which had been primary to Medicare (e.g., insured retired), enter the word NONE and proceed to item 11b.
When was 32B not reported?
Enter the ID qualifier 1C followed by one blank space and then the PIN of the service facility. Effective May 23, 2007, and later, 32b is not to be reported.