When can you enroll in Medicare supplement?
· The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period—for most people, this period starts the month that you turn 65 and have Medicare Part B, and goes for six months. This is when you can get any Medicare Supplement plan that’s available in your area, regardless of any health issues you …
When can you start applying for Medicare?
· When can I enroll in a Medicare Supplement Plan? When newly eligible for Medicare, you enter a seven-month Initial Enrollment Period (IEP) which begins three months before your 65th birthday and ends three months after the month of your birthday.
When is the best time to apply for Medicare?
If you are losing health insurance, like a employer sponsored group plan, you can generally apply for a Medicare Supplement Plan up-to 3 months before you would like coverage to start. In general, we recommend that you apply for a Medicare Supplement Plan around 2-3 months before you would like coverage to start.
What is the best medical supplement for Medicare?
The same is true for Medicare supplement plans, which are also known as Medigap plans. You can apply for these plans if you: Are enrolled in both Medicare Part A hospital and Part B medical insurance. Live in Michigan for at least six months of the year. Unlike the Medicare Advantage plans, you are able to apply for these plans anytime throughout the year once you meet the …
Can you add a supplement to Medicare at any time?
You can apply for a Medicare Supplement insurance plan anytime once you're enrolled in Medicare Part A and Part B – you're not restricted to certain enrollment periods as you are with other Medicare enrollment options.
When can a consumer enroll in a Medicare supplement plan?
General Enrollment Period (GEP): If you have Medicare Part A and are enrolling in Part B for the first time during the GEP, which is from January 1 – March 31 each year, you can also enroll in a Medicare Advantage plan (with our without prescription drug coverage) or a Part D prescription drug plan between April 1 – ...
Can a Medicare supplement plan be purchased at any time of the year?
If you're in good health and comfortable answering medical questions, you can apply to change Medigap plans at any time of the year. Medicare Advantage plans and Medicare Part D prescription drug plans can only be changed during certain times of year, but Medicare supplements are different.
What is deadline for Medicare supplement?
You can certainly apply for a new Medigap plan during the annual Medicare open enrollment period (October 15 to December 7), but that's no different from any other time of the year.
When can you switch from Medicare Advantage to a Medicare supplement?
From January 1 to March 31 each year, a person can switch from one Medicare Advantage plan to another or drop their Medicare Advantage plan altogether in favor of original Medicare. During this time, a person can also join a prescription drug plan and Medigap.
What is the average cost of supplemental insurance for Medicare?
Medicare Supplemental Insurance (Medigap) Costs. In 2020, the average premium for Medicare supplemental insurance, or Medigap, was approximately $150 per month or $1,800 per year, according to Senior Market Sales, a full-service insurance organization.
Do you have to renew Medicare supplement every year?
Medicare Supplement (Medigap) Plans: You do not have to do anything annually to renew them, and there is no annual open enrollment period for Medicare Supplement plans. They have the benefit of being “guaranteed renewable”. It will continue indefinitely unless you don't pay the premium.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
How many pints of blood are covered by Medicare supplement core benefits?
three pintsHow many pints of blood will be paid for by Medicare Supplement core benefits? Medicare Supplement core policy benefits will pay for the first three pints of blood.
Can Medigap insurance be denied for pre existing conditions?
Be aware that under federal law, Medigap policy insurers can refuse to cover your prior medical conditions for the first six months. A prior or pre-existing condition is a condition or illness you were diagnosed with or were treated for before new health care coverage began.
How long before you turn 65 do you apply for Medicare?
3 monthsYour first chance to sign up (Initial Enrollment Period) It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month.
What states are guaranteed issue for Medicare supplement?
Only four states (CT, MA, ME, NY) require either continuous or annual guaranteed issue protections for Medigap for all beneficiaries in traditional Medicare ages 65 and older, regardless of medical history (Figure 1).
When Am I Eligible For Medicare Supplement Coverage?
Because Medicare Supplement policies complement your Original Medicare coverage, you must be enrolled in Part A and Part B to be eligible for this...
How Can Enrollment Periods Affect My Eligibility For Medicare Supplement Plans?
The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period—for most people, this per...
Am I Eligible For A Medicare Supplement Plan If I’M Under Age 65?
Federal law does not require insurance companies to sell Medicare Supplement policies to people under 65, but many states do have this requirement....
Am I Eligible For A Medicare Supplement Plan If I Have A Medicare Advantage Plan?
Medicare Supplement policies don’t work with Medicare Advantage plans. If you decide to switch from Original Medicare to a Medicare Advantage plan,...
Am I Eligible For A Medicare Supplement Plan If I Have Coverage Through Medicaid?
While some beneficiaries may be eligible for both Medicare and Medicaid benefits (also known as “dual eligibles”), Medicaid typically doesn’t work...
What is Medicare Supplement Insurance?
Medicare Supplement Insurance (Medigap or MedSup), sold by private companies, helps pay some health care costs that Original Medicare (Part A and Part B) doesn’t cover. Policies can include coverage for deductibles, coinsurance, hospital costs, skilled nursing facility costs, and sometimes health care costs when traveling outside the U.S.
How long is the free look period for Medigap?
If you’re within your six-month Medigap Open Enrollment Period and considering a different Medigap plan, you may try a new Medigap policy during a 30-day “free look period.”. During this period, you will have two Medigap plans, and pay the premium for both.
Does Blue Cross Blue Shield of Michigan accept Medicare?
or its territories that accepts Medicare. You don't have to use our network. Blue Cross Blue Shield of Michigan administers Blue Cross Medicare Supplement plans. Where you live, your age, gender and whether you use tobacco may affect what you pay for your plan. Your health status may also affect what you pay. This is a solicitation of insurance. We may contact you about buying insurance. Blue Cross Medicare Supplement plans aren't connected with or endorsed by the U.S. government or the federal Medicare program.
How long can you live in Michigan with Medicare?
Live in Michigan for at least six months of the year. Applying for these plans isn't restricted to certain times of the year like Medicare Advantage plans.
When to buy Medigap policy?
Buy a policy when you're first eligible. The best time to buy a Medigap policy is during your 6-month Medigap Open Enrollment Period. You generally will get better prices and more choices among policies. During that time you can buy any Medigap policy sold in your state, even if you have health problems. This period automatically starts the first ...
Can you get Medicare if you are 65?
Some states provide these rights to all people with Medicare under 65. Other states provide these rights only to people eligible for Medicare because of disability or only to people with ESRD. Check with your State Insurance Department about what rights you might have under state law.
How long does it take for a pre-existing condition to be covered by Medicare?
Coverage for the pre-existing condition can be excluded if the condition was treated or diagnosed within 6 months before the coverage starts under the Medigap policy. After this 6-month period, the Medigap policy will cover the condition that was excluded. When you get Medicare-covered services, Original Medicare.
What is a copayment?
A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug. .
How long does it take to apply for Medicare Supplement?
When to apply for a Medicare Supplement plan. Here's the quick answer: Most people should apply for a Medigap plan within six months of signing up for Part B. Medigap open enrollment begins when you sign up for Medicare Part B (at age 65) and lasts for six months. If you defer Part B coverage past age 65 because of health coverage ...
How long does Medicare open enrollment last?
When to apply for a Medicare Supplement plan. Medigap open enrollment begins when you sign up for Medicare Part B (at age 65) and lasts for six months. If you defer Part B coverage past age 65 because of health coverage from your employer, this six-month window would start whenever you sign up for Part B.
Does Medicare cover medical expenses?
December 12, 2019. Medicare can cover a wide range of medical costs, but like anything else, it’s not perfect. We would all like a bit more coverage than Original Medicare can offer, especially when we know we'll be in more need of the benefits later in life. Luckily, Medicare Supplement (also called Medigap) plans provide a solution, ...
When does Medicare Part B open enrollment start?
Example B: You’re already 65, you sign-up for Medicare Part B and it begins June 1. This means that your Medigap Open Enrollment Period is from June 1 to November 30. If you get Medicare Part B before you turn 65, then your Open Enrollment Period starts the first day of the month you turn 65.
When is the open enrollment period for Medicare?
This means that your Medigap Open Enrollment Period is from June 1 to November 30. If you get Medicare Part B before you turn 65, then your Open Enrollment Period starts the first day of the month you turn 65. Example C: You enroll in Medicare Part B when you’re still 64 and in your Initial Enrollment Period.
How long does it take to disenroll from Medicare?
You decide to disenroll from a Medicare Advantage plan during a 12-month trial period. There are two times this happens.
Does Medicare cover people under 65?
Not all states require Medicare Supplement plans to cover people with Medicare who are under age 65. There are 33 states that require insurance companies to offer plans to people under age 65 who otherwise qualify for Medicare because of disability or end-stage renal disease (ESRD). 2. Arkansas.
How long does the Medigap open enrollment period last?
covered under Medicare Part B. Your Medigap Open Enrollment Period then lasts for a total of six months.
What happens if you miss the open enrollment deadline?
If you miss your 6-month open enrollment deadline, many insurers will still offer you coverage. However, insurers will be free to deny your application or charge higher monthly payments. In all cases, Medicare Supplement plans are renewable for life once you’ve enrolled in the plan.
What happens if you miss your Medigap enrollment?
If you miss your Medigap Open Enrollment Period, you may be subject to medical underwriting. This means that your application could be denied by the insurance company offering the plan. Your application could also be accepted at a higher price than you were hoping to spend.
What is Medicare Supplement Open Enrollment Period?
What is Medicare Supplement Open Enrollment? Medicare Supplement Open Enrollment Period is a once in a lifetime window that allows you to enroll in any Medigap plan without answering health questions.
Do you have to be 65 to get a Medigap plan?
Many states are not required to offer all supplement plans to those under 65. Most states only offer Plan A to those under 65. If they wait to enroll in a Medigap plan when they turn 65 during their second Medigap OEP, they’ll be able to choose from all the programs available to them in their state.
Which states have open enrollment?
Some states have unique open enrollment rules, like Connecticut and California. In California, they have a birthday rule that allows you to enroll days surrounding your birthday without answering health questions. In Connecticut, they have a year-round open enrollment window for all beneficiaries.
Does California have a birthday rule?
In California, they have a birthday rule that allows you to enroll days surrounding your birthday without answering health questions. In Connecticut, they have a year-round open enrollment window for all beneficiaries. So if you like in one of these states, you have a unique benefit that most beneficiaries don’t get!
What happens if you miss your Medigap open enrollment period?
When you miss your Medigap Open Enrollment Period and are denied coverage, there are alternative options. If you have a serious health condition that causes a Medigap carrier not to accept you, you should be able to enroll in a Medicare Advantage plan.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare. You can also find her over on our Medicare Channel on YouTube as well as contributing to our Medicare Community on Facebook.
How long do you have to keep Medicare Supplement?
The Medicare Supplement “Free Look” Period. When you switch Medicare Supplement Insurance plans, you generally are allowed 30 days to decide to keep it or not. This 30-day “free look” period starts when your new Medicare Supplement plan takes effect.
How long do you have to wait to switch Medigap?
Your insurance company may agree to sell you a new policy with the same basic benefits, but you may have to wait up to six months before the new plan covers any pre-existing health conditions . If any of the above situations apply to you, you can switch Medigap plans without medical underwriting.
Does Medicare Supplement pay for out of pocket costs?
Medigap plans are designed to fill those gaps by supplementing your Original Medicare coverage to pay for certain out-of-pocket costs. A Medicare Supplement plan may pay your coinsurance or copayments from Medicare Part A and Part B. Some Medigap plans also cover Part A and/or Part B deductibles and other costs.
Does Medicare Supplement pay coinsurance?
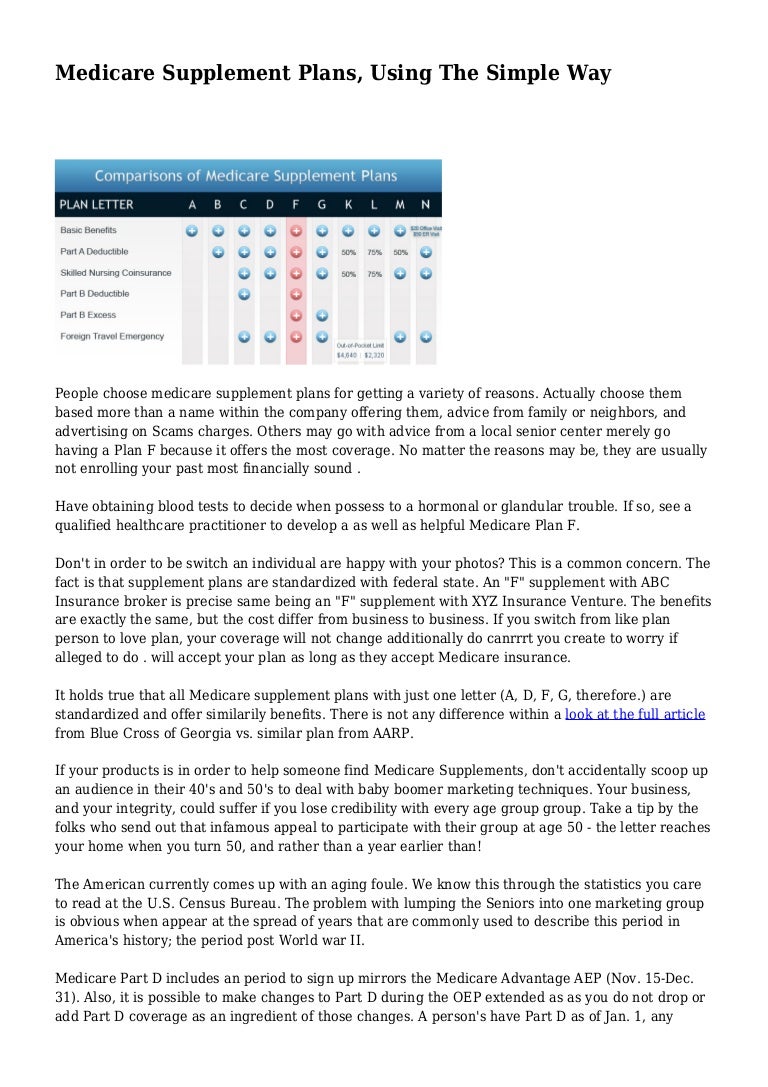
A Medicare Supplement plan may pay your coinsurance or copayments from Medicare Part A and Part B. Some Medigap plans also cover Part A and/or Part B deductibles and other costs. You can use the chart below to compare the out-of-pocket Medicare costs that different types of Medigap plans cover. * Plan F and Plan C are not available ...
Is Medigap a private insurance?
Medigap plans, however, are sold by private insurance companies. You must shop for these plans, and a licensed insurance agent can help you pick the one that offers you the best coverage at the best rates. Medicare Supplement plans carry letters to designate the benefits each type of plan offers.
How long does it take to enroll in Medigap?
If you do consider enrolling in a Medigap plan Medigap plans, you should try to apply for a plan during your 6-month Medigap Open Enrollment Period. Your Medigap Open Enrollment Period is a 6-month period that starts the day you are both 65 years old and enrolled in Medicare Part B.
What to do if your insurance rates go up?
If your rates go up, you may want to consider looking for a new policy. You can shop around for a similar plan offered by the same company or a different company for a lower premium. More coverage. If you decide you need more coverage, you can switch to a different plan letter to get more benefits. Less Coverage.
When does Medicare change coverage?
You can’t use this Special Enrollment Period from October–December. However, all people with Medicare can make changes to their coverage from October 15–December 7, and the changes will take effect on January 1.
What is a special enrollment period?
Special circumstances (Special Enrollment Periods) You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).