Yes, you may be eligible to purchase a Medicare Supplement
Medigap
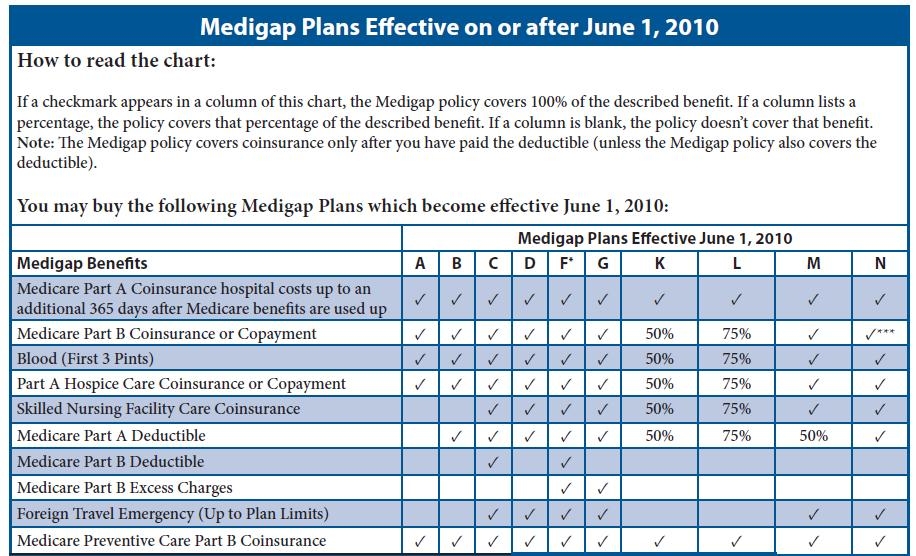
Medigap refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges. Medigap's name is derived from the notion that it exists to …
Full Answer
Who is eligible for a Medicare supplement insurance plan?
Feb 08, 2021 · The best time to buy a Medicare Supplement plan, or Medigap, is during your six-month open enrollment period. During this time, an insurance company cannot deny you coverage based on your health. After this period, you may pay more for a Medigap policy or get denied coverage due to poor health. Connect With a Medicare Expert
When can you sign up for Medicare supplement insurance?
Sep 16, 2018 · However, depending on where you live, you might not be able to purchase the policy option you want—or any Medicare Supplement policy—until you turn 65. As mentioned above, the best time to enroll in a plan is during your Medicare Supplement Open Enrollment Period, when you have guaranteed-issue rights.
Is there open enrollment for Medicare supplements?
Aug 09, 2018 · When can I enroll in a Medicare Supplement Plan? When newly eligible for Medicare, you enter a seven-month Initial Enrollment Period (IEP) which begins three months before your 65th birthday and ends three months after the month of your birthday.
When is open enrollment for Medicare?
Federal law guarantees you the right to buy any Medicare supplement insurance policy available where you live during the six months after you turn 65 and first enroll in Medicare Part B.

Can a Medicare supplement plan be purchased at any time of the year?
Can you add a supplement to Medicare at any time?
When can a consumer enroll in a Medicare supplement plan?
What situations allow for the purchase of a Medigap plan?
What is the average cost of supplemental insurance for Medicare?
Can I switch from Medicare Advantage to Medicare supplement?
Can Medigap insurance be denied for pre-existing conditions?
How long before you turn 65 do you apply for Medicare?
It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month.
What is the downside to Medigap plans?
Do you have to renew Medicare supplement every year?
You do not have to do anything annually to renew them, and there is no annual open enrollment period for Medicare Supplement plans. They have the benefit of being “guaranteed renewable”. It will continue indefinitely unless you don't pay the premium.May 16, 2018
How long is the guaranteed issue period for Medicare supplement?
Why do doctors not like Medicare Advantage plans?
When Am I Eligible For Medicare Supplement Coverage?
Because Medicare Supplement policies complement your Original Medicare coverage, you must be enrolled in Part A and Part B to be eligible for this...
How Can Enrollment Periods Affect My Eligibility For Medicare Supplement Plans?
The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period—for most people, this per...
Am I Eligible For A Medicare Supplement Plan If I’M Under Age 65?
Federal law does not require insurance companies to sell Medicare Supplement policies to people under 65, but many states do have this requirement....
Am I Eligible For A Medicare Supplement Plan If I Have A Medicare Advantage Plan?
Medicare Supplement policies don’t work with Medicare Advantage plans. If you decide to switch from Original Medicare to a Medicare Advantage plan,...
Am I Eligible For A Medicare Supplement Plan If I Have Coverage Through Medicaid?
While some beneficiaries may be eligible for both Medicare and Medicaid benefits (also known as “dual eligibles”), Medicaid typically doesn’t work...
When does Medigap coverage start?
Ask for your policy to become effective when you want coverage to start. Generally, Medigap policies begin the first of the month after you apply. If, for any reason, the insurance company won't give you the effective date for the month you want, call your State Insurance Department.
How long does it take to buy Medigap?
A one-time only, 6-month period when federal law allows you to buy any Medigap policy you want that's sold in your state. It starts in the first month that you're covered under Part B and you're age 65 or older.
How to fill out a medical application?
Tips for filling out your application 1 Fill out the application carefully and completely, including medical questions. The answers you give will determine your eligibility for open enrollment or guaranteed issue rights (also called "Medigap protections"). 2 If your insurance agent fills out the application, check to make sure it's correct. 3 Remember that the insurance company can't ask you any questions about your family history or require you to take a genetic test. 4 If you buy a Medigap policy during your#N#Medigap Open Enrollment Period#N#A one-time only, 6-month period when federal law allows you to buy any Medigap policy you want that's sold in your state. It starts in the first month that you're covered under Part B and you're age 65 or older. During this period, you can't be denied a Medigap policy or charged more due to past or present health problems. Some states may have additional open enrollment rights under state law.#N#, the insurance company can’t use any medical answers you give to deny you a Medigap policy or change the price. 5 If you provide evidence that you're entitled to a guaranteed issue right, the insurance company can't use any medical answers you give to deny you a Medigap policy or change the price.
Can you ask about your family history on Medigap?
Remember that the insurance company can't ask you any questions about your family history or require you to take a genetic test. A one-time only, 6-month period when federal law allows you to buy any Medigap policy you want that's sold in your state.
How long is the open enrollment period for Medigap?
Medigap Open Enrollment Period. A one-time only, 6-month period when federal law allows you to buy any Medigap policy you want that's sold in your state. It starts in the first month that you're covered under Part B and you're age 65 or older.
How to pay for insurance?
How to pay for your policy. It's best to pay by check, money order, or bank draft. Make it payable to the insurance company, not the agent. If buying from an agent, get a receipt with the insurance company's name, address, and phone number for your records. Some companies may offer electronic funds transfer.
When does Medigap start?
Generally, Medigap policies begin the first of the month after you apply. If, for any reason, the insurance company won't give you the effective date for the month you want, call your State Insurance Department.
Can you use Medicare Supplement Plan with Medicare Supplement?
While some beneficiaries may be eligible for both Medicare and Medicaid benefits (also known as “dual eligibles”), Medicaid typically doesn’t work with Medicare Supplement plans. You can only use your Medicare Supplement plan to pay for costs in Original Medicare.
How long do you have to wait to get Medicare Supplement?
Keep in mind that even though a Medicare Supplement insurance company cannot reject your enrollment for health reasons, the company is allowed to make you wait up to six months before covering your pre-existing conditions.
Does Medicare Supplement cover out-of-pocket expenses?
Medicare Supplement plans aren’t meant to provide stand-alone health coverage; these plans just help with certain out-of-pocket costs that Original Medicare doesn’t cover. If you’re under 65 and have Medicare because of disability, end-stage renal disease, or amyotrophic lateral sclerosis, your eligibility for Medicare Supplement coverage may ...
Does Medicare Supplement include prescription drug coverage?
In addition, keep in mind that Medicare Supplement plans don’t include prescription drug benefits (Medicare Part D). In the past, some Medicare Supplement plans may have included this coverage, but plans sold today don’t include prescription drug benefits. If you have an older Medicare Supplement policy with prescription drug coverage, ...
How long does Medicare Supplement open enrollment last?
How can enrollment periods affect my eligibility for Medicare Supplement plans? The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period —for most people, this period starts the month that you turn 65 and have Medicare Part B, and goes for six months.
When is the best time to enroll in Medicare Supplement?
The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period — for most people, this period starts the month that you turn 65 and have Medicare Part B, and goes for six months.
Can you change your Medicare Supplement plan if it goes bankrupt?
For example, if your Medicare Supplement insurance company goes bankrupt or misleads you, you may be able to change Medicare Supplement plans with guaranteed issue.
What is Medicare Supplement Insurance?
Medicare Supplement Insurance (Medigap or MedSup), sold by private companies, helps pay some health care costs that Original Medicare (Part A and Part B) doesn’t cover. Policies can include coverage for deductibles, coinsurance, hospital costs, skilled nursing facility costs, and sometimes health care costs when traveling outside the U.S.
How long is the free look period for Medigap?
If you’re within your six-month Medigap Open Enrollment Period and considering a different Medigap plan, you may try a new Medigap policy during a 30-day “free look period.”. During this period, you will have two Medigap plans, and pay the premium for both.
How long can you wait to buy a Medigap policy?
However, they cannot make you wait in this way if you’ve had continuous “creditable coverage” for at least six months before buying the Medigap policy.
How long do you have to enroll in Medigap before you can buy it?
If you enroll in Part B but allow more than six months to pass before buying Medigap (even if you disenroll from Part B to use insurance from a new employer and then reenroll when that employment ends), you are not entitled to another open enrollment period.
Can insurance companies refuse to sell medigap?
Federal law prohibits insurance companies from refusing to sell you a Medigap policy, or from charging you higher premiums based on your current health status or preexisting medical conditions, provided that you buy it within certain specified time frames:
How long does it take to get Medicare Part B?
Within six months of beginning to receive Medicare Part B benefits — regardless of whether you enroll in Part B at age 65 or delay enrollment until you (or your spouse) stop working for an employer that provides health insurance. This six-month “open enrollment” period for Medigap is a once-only opportunity.
How long does it take to lose Medicare Advantage?
Within 63 days of losing coverage if you leave a Medicare Advantage plan or drop a Medigap policy because the company hasn’t followed the rules or has misled you. Within 63 days of losing Medigap coverage through no fault of your own — for example, if the insurance company that sold you the policy goes bankrupt.
What happens if you turn 65 and can't buy a Medigap policy?
If you are unable to buy a Medigap policy right now, or can only buy one that charges you very high premiums, remember that when you turn 65, the clock will be reset.
How many policies are required to be available?
Some states require one or two policies to be made available. Most states allow insurers to take your health status and preexisting medical conditions into account when determining your premium, which can greatly push up the cost.
Is Medicare Supplement available to everyone?
Medicare Supplement insurance plans are not available to everyone. The first requirement is to be enrolled in Medicare Part A and Part B. When you become eligible for Medicare, you may have the choice to stay with Original Medicare (Part A and Part B) or go with a Medicare Advantage plan that covers your Medicare hospital and medical benefits (except for hospice care, which Part A still covers). Many Medicare Advantage plans also offer additional benefits, such as routine dental care. If you have Medicare Advantage, you can’t be sold a Medicare Supplement insurance plan.
What is Medicare Supplement?
Medicare Supplement insurance plans are standardized in most states, meaning that plans of the same letter offered by different companies must cover the same basic benefits. However, pricing for the same plan may differ from company to company. Insurance companies use three ways to price Medicare Supplement insurance plans:
What age do you have to be to get Medicare Supplement?
Disabled Under 65 . In 27 states, Medicare Supplement Insurance companies are required to sell policies to people under age 65 who receive Medicare benefits because of a qualifying disability or medical condition.
Do you have to have Medicare to be under 65?
State laws vary, but some states only require insurance companies to offer certain plans to people under 65. For example, Texas only requires companies to offer Medigap Plan A, which is the least comprehensive plan available. If you live in a different state, you may be denied altogether. Only the 27 states above are required to offer any Medicare ...
Do you pay more for Medigap than over 65?
You will probably pay more for your plan than people over 65. Some states require insurance companies to sell you a Medigap policy for the same price as people over 65, but most states allow companies to charge you more if you are under 65 and disabled. You may have to settle on a less comprehensive plan. State laws vary, but some states only ...
Does Medicare Supplement Insurance cover the gap?
Medicare Supplement Insurance helps you pay for the gaps in Medicare coverage. Once Medicare pays its share of the services you are receiving, Medigap will help you pay the rest. If your Part B policy says it covers 80% of a doctor’s visit, Medicare will pay that. Medigap kicks in for the other 20%.
Does Massachusetts have Medicare Supplement?
Medicare Supplement Plans in Massachusetts. Like we mentioned above, Medicare Supplement Insurance plans are structured differently in Massachusetts. Residents of the Bay State only have two plans to choose from: the Core Plan and the Supplement 1 Plan. Both plans cover basic benefits:
Who regulates Medicare Supplement Insurance?
Medicare Supplement Insurance plans are tightly regulated by the Centers for Medicare and Medicaid Services (CMS), a government agency. CMS determines what each letter plan will cover, and it requires each insurance company to offer the plan as is, without modifications.
Do you have to pay Medicare premiums if you are 65?
Part A covers inpatient hospital services, as well as care in a hospice or skilled nursing facility and some home health care expenses. Most people don’ t have to pay a premium for Part A ( premium-free Part A), but if you’re 65 and you didn’t pay the Medicare tax for 10 years or more, you may have to pay a premium.
How much is Medicare Part B deductible?
For 2019, the deductible for Medicare Part B is $185. After the deductible, you’ll pay 20% of most medical expenses.
Does Medicare pay for prescription drugs?
Medicare Part D helps you pay for prescription drugs. Depending on your plan, you may have to shop at preferred pharmacies to get the best price. You may also have to pay an out-of-pocket deductible before the insurance begins paying. Part D drug plans carry a premium which you must pay in addition to the Plan B premium.
How long do you have to be on Medicare if you have a disability?
If you have a disability and you’re receiving disability benefits from the Social Security Administration, you’ll automatically be enrolled in Parts A and B of Medicare once you’ve been receiving benefits for 24 months.
