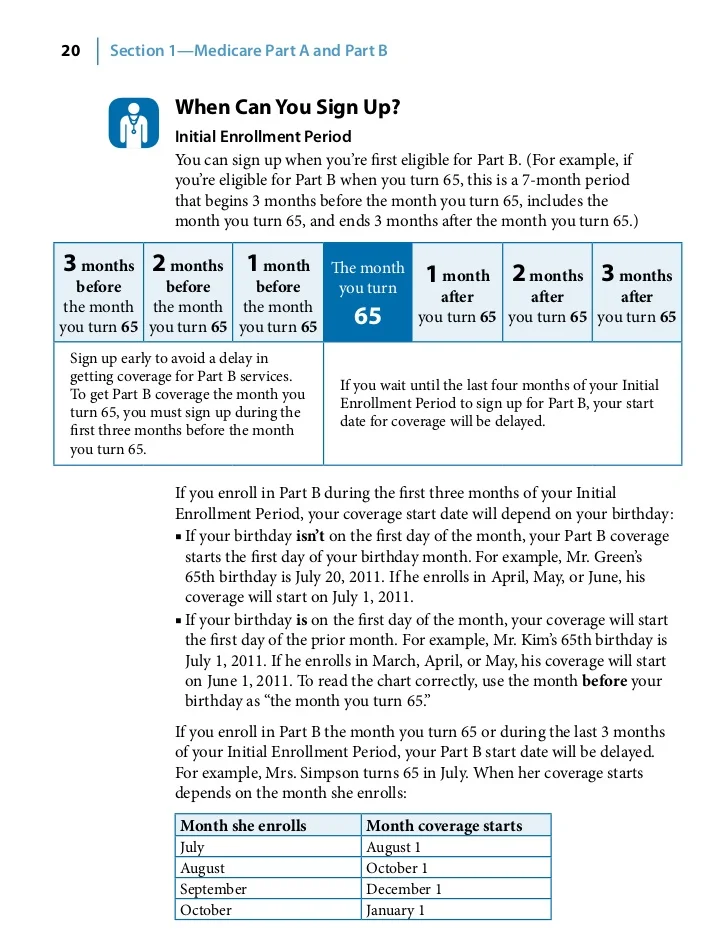
In most cases, you can enroll in Part D coverage within a seven-month time period that covers the months before, during and after reaching Medicare eligibility at age 65. This includes three months prior to your 65th birthday, the month of your birthday and then three months after your 65th birthday.
Full Answer
When should you enroll in Medicare Part D?
You’re eligible to enroll in a Part D plan if you receive Medicare upon turning 65. You’re also able to enroll if you sign up for Medicare due to a disability. If you delay getting Part D coverage for a while because you already had a group health plan that covered prescription drugs, you can apply for Part D when your existing coverage ends.
What drugs are excluded from Part D plans?
What drugs are excluded from Part D plans? There are many drugs that no Medicare plans will cover under the Part D benefit, based on national Medicare guidelines. Drugs for anorexia, weight loss, or weight gain (i.e., Xenical®, Meridia, phentermine HCl, etc.) Drugs that promote fertility (i.e., Clomid, Gonal-f, Ovidrel®, Follistim®, etc.)
What is covered by Medicare Part D?
QUINCY (WGEM) - For those of you with a Medicare D plan, a list of vaccines is now covered for you in Adams County. Starting on Monday, the Adams County Health Department will begin offering vaccines for Shingles, Tetanus, Hepatitis A and B, and more.
What is the average cost of Medicare Part D?
So how much does Medicare Part D cost? According to the Centers for Medicare & Medicaid Services (CMS), the average cost of a Medicare Part D plan in 2022 will be approximately $33 per month. That represents a 4.9% increase from the 2021 average of $31.47 per month.

Can you enroll in Medicare Part D at any time?
Keep in mind, you can enroll only during certain times: Initial enrollment period, the seven-month period that begins on the first day of the month three months before the month you turn 65 and lasts for three months after the birthday month.
Can I enroll in Medicare Part D if I don't have Part B?
This publication has information about enrolling in Medicare Advantage Plans and Medicare drug plans (Part D). You must have Medicare Part A (Hospital Insurance) and Part B (Medical Insurance) to join a Medicare Advantage Plan.
Can you enroll in Medicare Part D only?
If you are eligible for Medicare coverage, you are also eligible for the Medicare drug benefit (Part D). You must be enrolled in Medicare Part A and/or Part B to enroll in Part D. Medicare drug coverage is only available through private plans.
Is it too late to add Part D to Medicare?
You must do this within 60 days from the date on the letter telling you that you owe a late enrollment penalty. Also send any proof that supports your case, like a copy of your notice of creditable prescription drug coverage from an employer or union plan.
Who is most likely to be eligible to enroll in a Part D prescription drug plan?
You are eligible for Medicare Part D drug benefits if you meet the qualifications for Medicare eligibility, which are: You are age 65 or older. You have disabilities. You have end-stage renal disease.
Is it worth getting Medicare Part D?
Most people will need Medicare Part D prescription drug coverage. Even if you're fortunate enough to be in good health now, you may need significant prescription drugs in the future. A relatively small Part D payment entitles you to outsized benefits once you need them, just like with a car or home insurance.
What is the main problem with Medicare Part D?
The real problem with Medicare Part D plans is that they weren't set up with the intent of benefiting seniors. They were set up to benefit: –Pharmacies, by having copays for generic medications that are often far more than the actual cost of most of the medications.
What makes you eligible for Medicare Part D?
Those 65 or older who are entitled to or already enrolled in Medicare are eligible for Part D drug insurance. Also eligible are people who have received Social Security Disability Insurance (SSDI) benefits for more than 24 months and those who have been diagnosed with end-stage renal disease.
What is the most popular Medicare Part D plan?
Best-rated Medicare Part D providersRankMedicare Part D providerMedicare star rating for Part D plans1Kaiser Permanente4.92UnitedHealthcare (AARP)3.93BlueCross BlueShield (Anthem)3.94Humana3.83 more rows•Mar 16, 2022
What is the cost of Part D Medicare for 2022?
$33Part D. The average monthly premium for Part coverage in 2022 will be $33, up from $31.47 this year. As with Part B premiums, higher earners pay extra (see chart below). While not everyone pays a deductible for Part D coverage — some plans don't have one — the maximum it can be is $480 in 2022 up from $445.
Do I need Medicare Part D if I don't take any drugs?
No. Medicare Part D Drug Plans are not required coverage. Whether you take drugs or not, you do not need Medicare Part D.
When did the Part D late enrollment penalty start?
The Part D penalty has been in effect since Medicare introduced the drug benefit in 2006. At that time, people already in Medicare could sign up until May 15, 2006, without incurring a late enrollment penalty.
What happens if you don't enroll in Medicare?
Failing to enroll within this time period, also known as the initial enrollment period, means that you may face a late enrollment penalty if you choose to add Part D coverage at a later date. Although this penalty is added only after adding Part D coverage following the initial enrollment period, it may stick around for the duration of your Medicare enrollment even if you choose to remove Part D coverage in the future .
Why is Medicare important?
Enrolling in Medicare is an important step for many people in protecting their health and their finances as they age. The Medicare program assists millions of seniors and certain individuals with qualifying disabilities, and without Medicare, some Americans would struggle to afford the cost of healthcare and related expenses.
When does Part D start?
Your IEP runs from February 1 to August 31. The date when your Part D coverage begins depends on when you sign up: Enrolling during the first three months of the IEP means coverage begins the first day of the fourth month.
What happens if you turn 65 and have Medicare?
Are eligible for Extra Help. Note: If you are enrolled in Medicare because of a disability and currently pay a premium penalty, once you turn 65 you will no longer have to pay the penalty.
When does IEP coverage begin?
Enrolling during the fourth month of the IEP or any of the three months afterwards means coverage begins the month following the month of enrollment.
How long does an IEP last?
Your Part D IEP is usually the same as your Medicare IEP: the seven-month period that includes the three months before, the month of , and the three months following your 65th birthday. For example, let’s say you turn 65 in May. Your IEP runs from February 1 to August 31.
What happens if you don’t enroll in Medicare Part D during your initial enrollment period?
If you fail to enroll in Medicare Part D during your initial enrollment period, you won’t have another opportunity until the open enrollment period begins.
How do you switch to Medicare D from Medicare Advantage?
If you opted for Medicare Advantage rather than Original Medicare and wanted to make a switch, you can do so at a specific time of year.
How to get prescription drug coverage
Find out how to get Medicare drug coverage. Learn about Medicare drug plans (Part D), Medicare Advantage Plans, more. Get the right Medicare drug plan for you.
What Medicare Part D drug plans cover
Overview of what Medicare drug plans cover. Learn about formularies, tiers of coverage, name brand and generic drug coverage. Official Medicare site.
How Part D works with other insurance
Learn about how Medicare Part D (drug coverage) works with other coverage, like employer or union health coverage.
What happens if you don't enroll in Medicare Part D?
If you don’t enroll when you’re first eligible and don’t have creditable coverage, you could face a late enrollment penalty. Let’s take a closer look at using an example. Tip: Medicare Plan D and Part D aren’t the same things.
How does Medicaid work with Medicare Part D Plans?
Medicaid provides coverage for individuals and families that have low incomes or limited resources. Not all will qualify for Medicaid coverage in addition to Medicare coverage.
Why is Medicare Part D important?
For many, prescription medications are vital to maintaining a healthy lifestyle. The costs of medications can drain finances, Medicare Part D prescription helps those who need assistance with medications .
How long do you have to change your plan if you are no longer eligible for Part D?
If you’re no longer eligible for Extra Help for the following year, you will have a 3-month window to change plans. This period starts either the date you’re notified or when you’re no longer eligible;
Do all Medicare beneficiaries qualify for Medicaid?
Not all will qualify for Medicaid coverage in addition to Medicare coverage. Medicare beneficiaries with full Medicaid benefits are dually eligible. The majority of beneficiaries that are dual-eligible have very low income and significant health care needs. Dual eligible beneficiaries now automatically have Part D.
Is it necessary to take prescriptions on a regular basis?
For many seniors, taking prescription drugs on a regular basis is not optional. Patients who have regular medication needs should be sure to enroll as soon as Medicare Part D eligibility begins. Unexpected or not, the cost of medications can be financially exhausting, Part D plans provide you with a much lower cost for the same quality ...
Can Medicare delay Part D?
Delaying Part D When Eligible. Medicare may add a Part D Late Enrollment Penalty to your Part D premium each month you have Part D coverage. Unless you enroll in a Part D plan when you’re first eligible during your IEP. As we grow older our chances of needing prescriptions will often increase. If you have no creditable prescription drug coverage, ...
When does Medicare start?
If you want Medicare coverage to start when your job-based health insurance ends, you need to sign up for Part B the month before you or your spouse plan to retire. Your coverage will start the month after Social Security (or the Railroad Retirement Board) gets your completed forms. You’ll need to fill out an extra form showing you had job-based health coverage while you or your spouse were working.
When does Part B start?
If you sign up during this 8-month period, your Part B coverage will start the month after Social Security (or the Railroad Retirement Board) gets your completed forms. You’ll need to fill out an extra form showing you had job-based health coverage while you or your spouse were working.
What happens if you don't sign up for Medicare?
If you don’t sign up when you’re first eligible, you’ll have to wait to sign up and go months without coverage. You might also pay a monthly penalty for as long as you have Part B. The penalty goes up the longer you wait to sign up.
Can you get help with Medicare if you have medicaid?
Depending on the type of Medicaid you have, you may also qualify to get help paying your share of Medicare costs. Get details about cost saving programs.
Does Medicare cover hospital visits?
Medicare can help cover your costs for health care, like hospital visits and doctors’ services.
Does my state sign me up for Medicare?
Your state will sign you up for Medicare (or if you need to sign up).
Do you have health insurance now?
Are you or your spouse still working for the employer that provides your health insurance coverage?