When can I disenroll from Medicare Advantage?
The Medicare Advantage Disenrollment Period (MADP) is when you can disenroll from a Medicare Advantage plan and return to Original Medicare. This period occurs every year from January 1 to February 14.
How to switch from Medicare Advantage to Original Medicare?
- Call the Medicare Advantage plan you wish to leave and ask for a disenrollment form.
- Call 1-800-MEDICARE (1-800-633-4227) to request that your disenrollment be processed over the phone. TTY users should call 1-877-486-2048. ...
- Call the Social Security Administration or visit your Social Security Office to file your disenrollment request.
How to disenroll from an advantage plan?
You may disenroll from your Bright HealthCare Medicare Plan by:
- Enrolling in another Medicare Advantage plan. Enrollment into another Medicare Advantage or a prescription drug plan will disenroll you from your Bright HealthCare plan. ...
- Providing a written notice to Bright HealthCare by mail or fax, signed by you or a legal representative. Download a disenrollment form.
- Calling 1-800-Medicare.
How often can I change Medicare plans?
You’ll need the following information:
- Your Medicare number
- The policy and group numbers of your current plan
- The dates you want changes to take effect (if you’re in a special enrollment period)
Can I switch back to a Medigap from Medicare Advantage?
You may have chosen Medicare Advantage and later decided that you'd rather have the protections of a Medicare Supplement (Medigap) insurance plan that go along with Original Medicare. The good news is that you can switch from Medicare Advantage to Medigap, as long as you meet certain requirements.
Can a person switch from Medicare Advantage to original Medicare?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
When can you make changes to Medigap?
The Medigap insurance company may be able to make you wait up to 6 months for coverage of pre-existing conditions. The number of months you've had your current Medigap policy must be subtracted from the time you must wait before your new Medigap policy covers your pre-existing condition.
When can you disenroll from a Medicare Advantage plan?
The Medicare Advantage Disenrollment Period (MADP) is when you can disenroll from a Medicare Advantage plan and return to Original Medicare. This period occurs every year from January 1 to February 14.
Can I switch from a Medicare Advantage plan to a Medigap plan?
Most Medicare Advantage Plans offer prescription drug coverage. , you may want to drop your Medigap policy. Your Medigap policy can't be used to pay your Medicare Advantage Plan copayments, deductibles, and premiums.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Can you add Medigap plans at any time?
Generally, there is no type of Medicare plan that you can get “any time.” All Medicare coverage, including Medicare Supplement (Medigap) plans, is subject to enrollment periods. Other types of Medicare plans, like Medicare Advantage and Medicare Part D prescription drug plans, have open enrollment periods every year.
Can I switch my Medicare supplement plan at any time?
As a Medicare beneficiary, you can change supplements at any time. As a result, there's no guarantee an application will be accepted if switched outside the designated Open Enrollment Period. An application may be “medically underwritten”.
Can Medigap insurance be denied for pre existing conditions?
Be aware that under federal law, Medigap policy insurers can refuse to cover your prior medical conditions for the first six months. A prior or pre-existing condition is a condition or illness you were diagnosed with or were treated for before new health care coverage began.
Are you automatically disenrolled from a Medicare Advantage plan?
To switch to a new Medicare Advantage Plan, simply join the plan you choose during one of the enrollment periods. You'll be disenrolled automatically from your old plan when your new plan's coverage begins. To switch to Original Medicare, contact your current plan, or call us at 1-800-MEDICARE.
Why is Medicare Advantage being pushed so hard?
Advantage plans are heavily advertised because of how they are funded. These plans' premiums are low or nonexistent because Medicare pays the carrier whenever someone enrolls. It benefits insurance companies to encourage enrollment in Advantage plans because of the money they receive from Medicare.
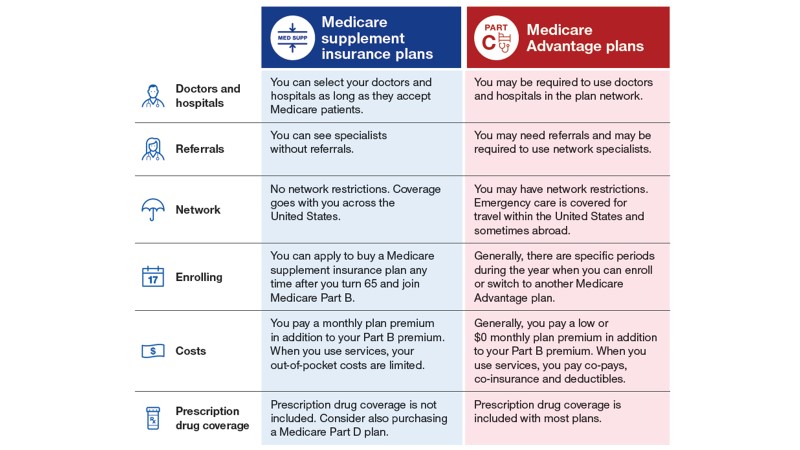
What is the difference between a Medicare Supplement and a Medicare Advantage plan?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.
How long does it take to switch to Medicare Advantage?
If a person enrolls in Medicare Advantage when they first become eligible for Medicare, they can switch to original Medicare and Medigap within the first 3 months of their plan.
How to disenroll from Medicare Advantage?
It is possible to disenroll from a Medicare Advantage plan by contacting the insurance company directly and requesting a disenrollment form. People can also call Medicare at 800-633-4227 and ask for disenrollment from their plan, or they can visit their local Social Security office.
How to find a Medigap policy?
If a person has never enrolled in a Medigap plan, they can find available Medigap policies by searching on Medicare.gov, contacting a State Health Insurance Assistance Program, or contacting an insurance agent or company to obtain a Medigap quote.
What is Medicare Advantage?
Medicare Advantage, or Medicare Part C, is a bundled plan that private companies administer. The plans vary based on which medical services are available in a certain area, and people often need to receive treatment from an approved network of healthcare professionals. Learn more here.
When does Medicare drop out of the OEP?
The first enrollment period runs from October 15 to December 7 each year. This is the OEP for all Medicare plans, including Medicare Advantage and Medicare prescription drug coverage.
Is Medicare Advantage a supplemental insurance?
There are several differences between Medicare Advantage and Medicare supplemental insurance, or Medigap. For example, a person can only enroll in a Medigap plan alongside original Medicare (Part A and Part B). However, this is not compulsory and serves only as a supplemental policy to reduce out-of-pocket costs.
Does Medicare cover out of pocket costs?
However, out-of-pocket costs usually include deductibles and coinsurance. Medigap plans, or Medicare supplement plans, are available to help people fund these extra costs. People can enroll in them alongside traditional ...
When can I disenroll from Medicare Advantage?
Annual enrollment takes place in the fall from October 15 through December 7.
When is the open enrollment period for Medicare?
The Medicare Advantage open enrollment period is one last chance to change your policy for the year. It takes place from January 1 through March 31 each year. There are other enrollment periods available, such as the initial enrollment period for those newly eligible for Medicare.
How many states require Medigap?
Also, four states require Medigap companies to offer plans to those over 65 either throughout the year or during one month of each year. People in Maine, Massachusetts, Connecticut and New York have ongoing access to Medigap plans.
Can you cancel Medigap before you cancel?
You want to be sure the Medigap plan accepts your application before you cancel your Advantage plan. The most important information any insurance agent will tell you: Never cancel a policy over a quote. It's best to wait until you have the final plan in your hands before you cancel current coverage.
Can you switch to Medigap without underwriting?
For example, when you get a Medicare Advantage plan as soon as you're eligible for Medicare, and you're still within the first 12 months of having it, you can switch to Medigap without underwriting. The opportunity to change is the "trial right.".
Can you judge a Medicare plan by the premium?
You can't judge a policy by the premium; instead, judge a plan by the way it covers you when you need to be covered. A higher premium with lower out-of-pocket dues could potentially be more beneficial than a lower premium with higher costs. Medigap has some advantages over a Medicare Advantage plan.
Can you change your Medicare plan during your birthday?
Some states, such as California and Oregon, allow you to change from one Medigap plan to a different Medigap plan during your birthday month. Vermont and Washington allow Medigap changes throughout the year, though there are some guidelines. While Medicare is a federal program, there are a lot of states with specific rules.
If you change from Medicare Advantage to Original Medicare plus a Medigap plan when you have guaranteed issue rights, your application won't go through medical underwriting (that's a good thing)
If you’re enrolled in a Medicare Advantage (MA) plan but changed your mind and would rather have a Medicare Supplement (Medigap) insurance plan with Original Medicare, that’s ok. You’re able to switch from Medicare Advantage to Medigap during certain times of the year or with specific qualifying circumstances.
Changing from Medicare Advantage to Medigap
You cannot enroll in both Medicare Advantage and Medigap. If you’d like to switch from an MA plan to a Medigap plan alongside Original Medicare, you must meet certain requirements or do so during a specific time of the year.
When Can I Switch from Medicare Advantage to Medigap?
There are a few times per year when you can leave a Medicare Advantage plan:
How to Switch from Medicare Advantage to Medigap
Here are the steps you’d take to switch from an MA plan to Original Medicare with a Medigap policy during a qualifying circumstance or enrollment period:
What Are Guaranteed-Issue Rights?
In most cases, if you switch to Original Medicare from an MA plan, you lose your guaranteed-issue rights for Medigap. These rights ensure you can purchase any plan sold in your state/area, and you can’t be charged higher premiums based on your health status.
What Is Medicare Advantage?
Medicare Advantage plans (Part C) are offered by private insurance companies contracted through Medicare. They offer the same hospital and medical coverage that Original Medicare does (through Part A and Part B), but they also offer additional coverage such as vision, dental, hearing aids, travel, wellness/gym memberships, and more.
What Is Medigap?
Medicare Supplement, or Medigap, is a supplemental insurance that helps fill “gaps” in Original Medicare coverage. While Medicare pays for much of the hospital and medical costs you may need, it doesn’t cover everything, which is why some people choose to purchase a Medigap policy.
How many options are there for Medicare Advantage?
Usually there are 4 options for seniors currently on a Medicare Advantage (MA) plan who would like to change to a Medicare Supplement (Medigap) plan. Under the first two options, switchers are guaranteed to be approved. Options 3 and 4 require completing certain medical questions before approval.
What is the phone number for Medicare?
If you have an urgent matter or need enrollment assistance, call us at 800-930-7956. By submitting your question here, you agree that a licensed sales representative may respond to you about Medicare Advantage, Prescription Drug, and Medicare Supplement Insurance plans.
Does Medigap cover out of pocket expenses?
Certain Medigap plans cover all deductibles and most cover all out of pocket costs. You want protect your wealth. Owning a Medigap plan is considered by many the best way to protect yourself from the high cost of medical bills .
Does Medigap have the same network as Medicare?
You are looking to access a bigger network of doctors. Medigap accesses the same network of doctors as Original Medicare, the largest network of doctors in America. You want increased benefits.
How long do you have to keep Medicare Advantage Plan?
If you don’t drop your Medicare Advantage Plan and return to Original Medicare within 12 months of joining, generally, you must keep your Medicare Advantage Plan for the rest of the year. You can disenroll or change plans during the Open Enrollment Period or if you qualify for a Special Enrollment Period.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). .
Does Medigap have prescription drug coverage?
The Medigap policy can no longer have prescription drug coverage even if you had it before, but you may be able to join a. Medicare Drug Plan (Part D) Part D adds prescription drug coverage to: Original Medicare. Some Medicare Cost Plans. Some Medicare Private-Fee-for-Service Plans.
Can you get a Medigap policy back if you leave Medicare?
If you leave the Medicare Advantage Plan, you might not be able to get the same, or in some cases, any Medigap policy back unless you have a " trial right. ". If you have a Medicare Advantage Plan, it's illegal for anyone to sell you a Medigap policy unless you're switching back to. Original Medicare.
How to switch Medigap insurance?
How to switch Medigap policies. Call the new insurance company and arrange to apply for your new Medigap policy. If your application is accepted, call your current insurance company, and ask for your coverage to end. The insurance company can tell you how to submit a request to end your coverage.
What happens if you buy a Medigap policy before 2010?
If you bought your policy before 2010, it may offer coverage that isn't available in a newer policy. If you bought your policy before 1992, your policy: Might not be a Guaranteed renewable policy. May have a bigger Premium increase than newer, standardized Medigap policies currently being sold. expand.
How long do you have to have a Medigap policy?
If you've had your Medicare SELECT policy for more than 6 months, you won't have to answer any medical questions.
How long is the free look period for Medigap?
Medigap free-look period. You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period.". The 30- day free look period starts when you get your new Medigap policy. You'll need to pay both premiums for one month.
Can you exclude pre-existing conditions from a new insurance policy?
The new insurance company can't exclude your Pre-existing condition. If you've had your Medigap policy less than 6 months: The number of months you've had your current Medigap policy must be subtracted from the time you must wait before your new Medigap policy covers your pre-existing condition.
Does Medicare cover Part B?
As of January 1, 2020, Medigap plans sold to new people with Medicare aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on January 1, 2020.
Can I keep my Medigap policy if I move out of state?
I'm moving out of state. You can keep your current Medigap policy no matter where you live as long as you still have Original Medicare. If you want to switch to a different Medigap policy, you'll have to check with your current or new insurance company to see if they'll offer you a different policy. If you decide to switch, you may have ...
