When can I enroll in a Medicare supplement plan?
When can I enroll in a Medicare Supplement Plan? When newly eligible for Medicare, you enter a seven-month Initial Enrollment Period (IEP) which begins three months before your 65th birthday and ends three months after the month of your birthday.
Should you switch Medicare supplement insurance plans?
When you switch Medicare Supplement Insurance plans, you generally are allowed 30 days to decide to keep it or not. This 30-day “free look” period starts when your new Medicare Supplement plan takes effect. To qualify, you need to pay the premiums for both your new plan and your old plan for one month. Should You Change Your Medigap Policy?
Can I get Medicare supplement insurance if I'm under 65?
Yes, you may be eligible to purchase a Medicare Supplement Insurance plan if you are under 65 and are enrolled in Medicare because of a disability. Federal law does not require states to sell Medicare Supplement Insurance policies to people under 65, but certain state laws do.
How to compare Medicare supplement plans for 2020?
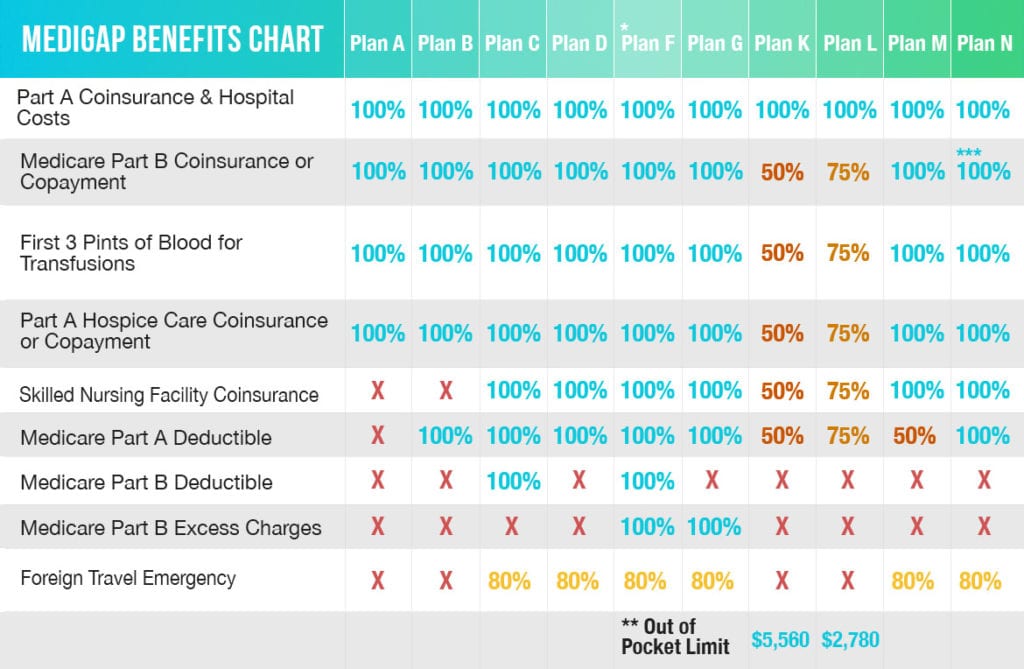
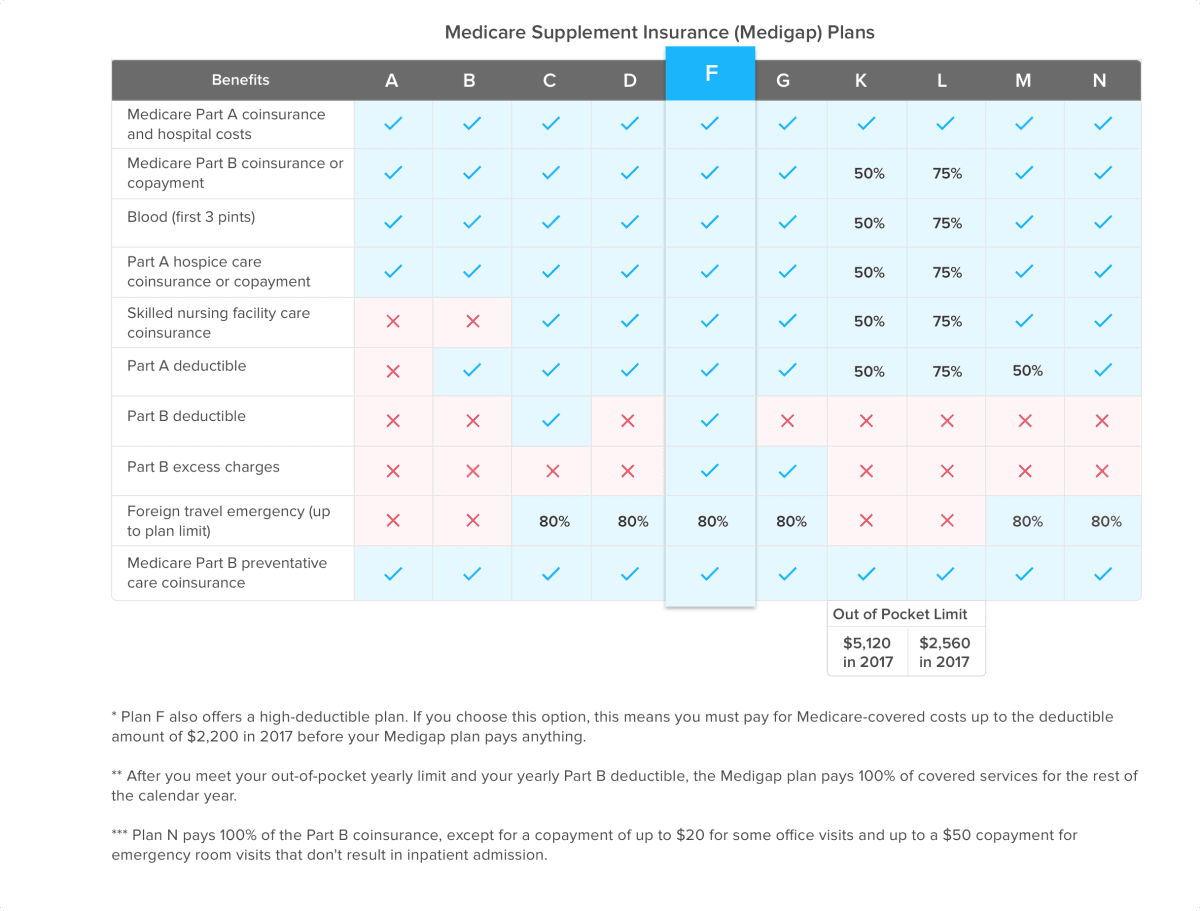
How to Compare Medicare Supplement Plans 1. Plans F and G also offer a high-deductible plan that each have an annual deductible of $2,340 in 2020. Once the... 2. Plan K has an out-of-pocket yearly limit of $5,880 in 2020. After you pay the out-of-pocket yearly limit and yearly... 3. Plan L has an ...
Can you change your Medicare Supplement anytime?
As a Medicare beneficiary, you can change supplements at any time. As a result, there's no guarantee an application will be accepted if switched outside the designated Open Enrollment Period. An application may be “medically underwritten”.
When can you change supplement plans?
When you switch from one Medicare Supplement insurance plan to another, you typically get 30 days to decide if you want to keep it. This 30-day free look period starts when you get your new Medicare Supplement insurance plan. You'll need to pay the premiums for both your new plan and your old plan for one month.
How often can you change your Medicare Supplement?
Is there a time limit or deadline for changing Medicare supplement plans? No there is not. Once your six-month open enrollment period has expired, you can change anytime. However, there's generally no reason to change unless you've had a rate increase and are shopping for a lower rate.
Can you change Medicare Supplement plans with pre-existing conditions?
You can change your Medicare Supplement plan at any time. However, if you're outside of your Medigap Open Enrollment Period or don't have guaranteed issue rights at the time, you'll have to answer underwriting questions and could face denial or increased monthly premiums due to pre-existing conditions.
Can I switch to a different Medigap policy?
. If you want to switch to a different Medigap policy, you'll have to check with your current or new insurance company to see if they'll offer you a different policy. If you decide to switch, you may have to pay more for your new Medigap policy.
Can you have two Medicare Supplement plans?
Retirees can't have more than one Medicare supplement plan or one at the same time as a Medicare Advantage plan. To cut costs on health care, start by calculating whether a supplement or an Advantage plan will save you the most money.
Is there a penalty for changing Medicare Supplement plans?
It usually costs nothing to switch Medicare plans. However, people who switch plans may face higher premiums. Some people may also face penalties for switching to certain plans after the IEP.
Can I change Medicare plans in the middle of the year?
If you're covered by both Medicare and Medicaid, you can switch plans at any time during the year. This applies to Medicare Advantage as well as Medicare Part D.
Can I change from Medicare Supplement plan F to plan G?
Can't I just move from a Medigap Plan F to a Plan G with the same insurance plan? Yes, you can. However, it usually still requires answering health questions on an application before they will approve the switch.
When can someone enroll in a Medicare Supplement without the chance for denial premium increase or exclusions due to pre-existing conditions?
For up to six months after your Medicare Supplement plan begins, your new plan can choose not to cover its portion of payments for preexisting conditions that were treated or diagnosed within six months of the start of the policy.
Is there a waiting period for pre-existing conditions Medicare Supplement?
Health or prescription drug costs that you must pay on your own because they aren't covered by Medicare or other insurance. for these pre-existing health problems for up to 6 months (called the "pre-existing condition waiting period"). After these 6 months, the Medigap policy will cover your pre-existing condition.
Can you switch from Medicare Supplement to advantage?
If you currently have Medicare, you can switch to Medicare Advantage (Part C) from Original Medicare (Parts A & B), or vice versa, during the Medicare Annual Enrollment Period. If you want to make a switch though, it may also require some additional decisions.
How long do you have to keep Medicare Supplement?
The Medicare Supplement “Free Look” Period. When you switch Medicare Supplement Insurance plans, you generally are allowed 30 days to decide to keep it or not. This 30-day “free look” period starts when your new Medicare Supplement plan takes effect.
What is a Medicare Supplement Plan?
Medigap plans are designed to fill those gaps by supplementing your Original Medicare coverage to pay for certain out-of-pocket costs. A Medicare Supplement plan may pay your coinsurance or copayments from Medicare Part A and Part B.
What happens if you don't change your Medicare Supplement?
If you don't change Medicare Supplement insurance plans during your Medigap Open Enrollment Period, your insurer can force you to undergo medical underwriting, and they can now assess your health history during the application process and can turn you down if it chooses.
What to do if you are unhappy with your Medicare Supplement?
If you are unhappy with your insurance company for any reason, you can purchase a plan from a different insurance underwriter. Call to speak with a licensed insurance agent who can help you compare Medicare Supplement plans in your area. They can help you change plans once you find the best plan for your needs.
How long does it take to enroll in Medigap?
If you do consider enrolling in a Medigap plan Medigap plans, you should try to apply for a plan during your 6-month Medigap Open Enrollment Period. Your Medigap Open Enrollment Period is a 6-month period that starts the day you are both 65 years old and enrolled in Medicare Part B.
How long do you have to wait to switch Medigap?
Your insurance company may agree to sell you a new policy with the same basic benefits, but you may have to wait up to six months before the new plan covers any pre-existing health conditions . If any of the above situations apply to you, you can switch Medigap plans without medical underwriting.
Do you have to change your Medicare plan during the open enrollment period?
If you don't change Medicare Supplement insurance plans during your Medigap Open Enrollment Period, ...
What is the original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). (Part A and Part B) or a.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What happens if you don't get Medicare?
If you don't get Medicare drug coverage or Medigap when you're first eligible, you may have to pay more to get this coverage later. This could mean you’ll have a lifetime premium penalty for your Medicare drug coverage . Learn more about how Original Medicare works.
How much does Medicare pay for Part B?
For Part B-covered services, you usually pay 20% of the Medicare-approved amount after you meet your deductible. This is called your coinsurance. You pay a premium (monthly payment) for Part B. If you choose to join a Medicare drug plan (Part D), you’ll pay that premium separately.
Does Medicare Advantage cover prescriptions?
Most Medicare Advantage Plans offer prescription drug coverage. . Some people need to get additional coverage , like Medicare drug coverage or Medicare Supplement Insurance (Medigap). Use this information to help you compare your coverage options and decide what coverage is right for you.
Your other coverage
Do you have, or are you eligible for, other types of health or prescription drug coverage (like from a former or current employer or union)? If so, read the materials from your insurer or plan, or call them to find out how the coverage works with, or is affected by, Medicare.
Cost
How much are your premiums, deductibles, and other costs? How much do you pay for services like hospital stays or doctor visits? What’s the yearly limit on what you pay out-of-pocket? Your costs vary and may be different if you don’t follow the coverage rules.
Doctor and hospital choice
Do your doctors and other health care providers accept the coverage? Are the doctors you want to see accepting new patients? Do you have to choose your hospital and health care providers from a network? Do you need to get referrals?
Prescription drugs
Do you need to join a Medicare drug plan? Do you already have creditable prescription drug coverag e? Will you pay a penalty if you join a drug plan later? What will your prescription drugs cost under each plan? Are your drugs covered under the plan’s formulary? Are there any coverage rules that apply to your prescriptions?
Quality of care
Are you satisfied with your medical care? The quality of care and services given by plans and other health care providers can vary. Get help comparing plans and providers
Convenience
Where are the doctors’ offices? What are their hours? Which pharmacies can you use? Can you get your prescriptions by mail? Do the doctors use electronic health records prescribe electronically?
How to compare Medicare Supplement Plans 2021?
How to Compare Medicare Supplement Plans. You can use the 2021 Medigap plan chart below to compare the benefits that are offered by each type of plan. Use the scroll bar at the bottom of the chart to view all plans and information. Click here to view enlarged chart. Scroll to the right to continue reading the chart. Scroll for more.
What is the most popular Medicare Supplement?
Medigap Plan F is the most popular Medicare Supplement Insurance plan . 53 percent of all Medigap beneficiaries are enrolled in Plan F. 2. Plan F covers more standardized out-of-pocket Medicare costs than any other Medigap plan. In fact, Plan F covers all 9 of the standardized Medigap benefits a plan may offer.
How much is the Medicare Part B deductible for 2021?
In 2021, the Part B deductible is $203 per year. Medicare Part B coinsurance or copayment. After you meet your Part B deductible, you are typically required to pay a coinsurance or copay of 20 percent of the Medicare-approved amount for your covered services.
What is the second most popular Medicare plan?
Medigap Plan G is the second most popular Medigap plan, and it is quickly growing in popularity. Plan G enrollment spiked 39 percent in recent years. 2. Medigap Plan G covers all of the same out-of-pocket Medicare costs than Plan F covers, except for the Medicare Part B deductible.
What are the benefits of Medigap?
Here are some key facts about Medicare Supplement Insurance: 1 Medigap insurance doesn't typically offer any additional benefits. Instead, it picks up the out-of-pocket costs associated with Medicare. 2 Medigap insurance is accepted by any doctor, hospital or health care provider who accepts Medicare. 3 If your health care service or medical device is covered by Medicare, your Medigap plan would cover any additional out of pocket costs so that you don't pay anything for your services (depending on your Medigap plan coverage and whether or not you've reached certain Medicare deductibles).
How much coinsurance is required for skilled nursing?
There is no coinsurance requirement for the first 20 days of inpatient skilled nursing facility care. However, a $185.50 per day coinsurance requirement begins on day 21 of your stay, and you are then responsible for all costs after day 101 of inpatient skilled nursing facility care (in 2021).
How much does Medicare Part A cover?
Medicare Part A helps cover your hospital costs if you are admitted to a hospital for inpatient treatment (after you reach your Medicare Part A deductible, which is $1,484 per benefit period in 2021). For the first 60 days of your hospital stay, you aren't required to pay any Part A coinsurance.
How to switch Medigap insurance?
How to switch Medigap policies. Call the new insurance company and arrange to apply for your new Medigap policy. If your application is accepted, call your current insurance company, and ask for your coverage to end. The insurance company can tell you how to submit a request to end your coverage.
How long do you have to have a Medigap policy?
If you've had your Medicare SELECT policy for more than 6 months, you won't have to answer any medical questions.
What happens if you buy a Medigap policy before 2010?
If you bought your policy before 2010, it may offer coverage that isn't available in a newer policy. If you bought your policy before 1992, your policy: Might not be a Guaranteed renewable policy. May have a bigger Premium increase than newer, standardized Medigap policies currently being sold. expand.
How long is the free look period for Medigap?
Medigap free-look period. You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period.". The 30- day free look period starts when you get your new Medigap policy. You'll need to pay both premiums for one month.
Can you exclude pre-existing conditions from a new insurance policy?
The new insurance company can't exclude your Pre-existing condition. If you've had your Medigap policy less than 6 months: The number of months you've had your current Medigap policy must be subtracted from the time you must wait before your new Medigap policy covers your pre-existing condition.
Does Medicare cover Part B?
As of January 1, 2020, Medigap plans sold to new people with Medicare aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on January 1, 2020.
Can I keep my Medigap policy if I move out of state?
I'm moving out of state. You can keep your current Medigap policy no matter where you live as long as you still have Original Medicare. If you want to switch to a different Medigap policy, you'll have to check with your current or new insurance company to see if they'll offer you a different policy. If you decide to switch, you may have ...
What Is Medigap?
Medigap, or Medicare Supplement, is a private insurance policy purchased to help pay for what isn’t covered by Original Medicare (which includes Part A and Part B). These secondary coverage plans only apply with Original Medicare—not other private insurance policies, standalone Medicare plans or Medicare Advantage plans.
How to Choose the Right Medicare Supplement Plan for You
What are my health care needs now and possibly in the future? Consider your current health status as well as your family history.
Best Medicare Supplement Providers
Many health insurance companies offer various Medigap plans, but not all providers issue policies in all 50 states or boast high rankings from rating agencies like A.M. Best.
How to Sign Up for Medigap Plans
Signing up for a Medigap plan is easy. “Medicare supplements may be bought through an agent or from the carrier directly,” says Corujo. Since there’s no annual open enrollment period, you may join at any time.
What age do you have to be to get Medicare Supplement?
Disabled Under 65 . In 27 states, Medicare Supplement Insurance companies are required to sell policies to people under age 65 who receive Medicare benefits because of a qualifying disability or medical condition.
Do you have to have Medicare to be under 65?
State laws vary, but some states only require insurance companies to offer certain plans to people under 65. For example, Texas only requires companies to offer Medigap Plan A, which is the least comprehensive plan available. If you live in a different state, you may be denied altogether. Only the 27 states above are required to offer any Medicare ...
Do you pay more for Medigap than over 65?
You will probably pay more for your plan than people over 65. Some states require insurance companies to sell you a Medigap policy for the same price as people over 65, but most states allow companies to charge you more if you are under 65 and disabled. You may have to settle on a less comprehensive plan. State laws vary, but some states only ...