What is the deadline for Medicare supplement?
When to sign up for a Medicare Supplement (Medigap) plan. If you choose to get your benefits through Original Medicare, you have the option of purchasing a Medigap plan. Once you turn 65 and have enrolled in Part B, you will have a 6-month Medigap Initial Enrollment Period. Medicare Supplement, also known as Medigap, policies help cover some of the costs Original Medicare …
Is there open enrollment for Medicare supplements?
Sep 16, 2018 · The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period —for most people, this period starts the month that you turn 65 and have Medicare Part B, and goes for six months.
How to enroll in Medicare if you are turning 65?
Dec 12, 2019 · When to apply for a Medicare Supplement plan Here's the quick answer: Most people should apply for a Medigap plan within six months of signing up for Part B. Medigap open enrollment begins when you sign up for Medicare Part B (at age 65) and lasts for six months.
Is there a deadline for Medicare supplemental insurance?
For example, if you turn 65 and are enrolled in Part B in June, the best time for you to buy a Medigap policy is from June to November. After this enrollment period, your option to buy a Medigap policy may be limited and it may cost more. Some states have additional open enrollment periods. I'm under 65.

Can Medicare Supplements be purchased at any time of the year?
If you're in good health and comfortable answering medical questions, you can apply to change Medigap plans at any time of the year. Medicare Advantage plans and Medicare Part D prescription drug plans can only be changed during certain times of year, but Medicare supplements are different.Jan 26, 2021
What is the open enrollment period for Medicare Supplements?
Under federal law, you have a six-month open enrollment period that begins the month you are 65 or older and enrolled in Medicare Part B. During your open enrollment period, Medigap companies must sell you a policy at the best available rate regardless of your health status, and they cannot deny you coverage.
Can I change Medicare supplement plans anytime?
You can change your Medicare Supplement Plan anytime, just be aware that you might have to answer medical questions if your outside your Open Enrollment Period.
Can you switch from Medicare Advantage to Medigap without underwriting?
For example, when you get a Medicare Advantage plan as soon as you're eligible for Medicare, and you're still within the first 12 months of having it, you can switch to Medigap without underwriting. The opportunity to change is the "trial right."Jun 3, 2020
What states are guaranteed issue for Medicare Supplement?
Only four states (CT, MA, ME, NY) require either continuous or annual guaranteed issue protections for Medigap for all beneficiaries in traditional Medicare ages 65 and older, regardless of medical history (Figure 1).Jul 11, 2018
What are the four prescription drug coverage stages?
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.Oct 1, 2021
How often can you change your Medicare Part D plan?
If you want to switch to a Part D plan or a Medicare Advantage plan that has earned Medicare's highest quality rating (five stars) — if one is available in your area — you can do so once at any time of the year, except for one week (Nov.
Can you change Medicare Supplement plans mid year?
You can either change to a standardized Medicare Supplement insurance plan with the same or fewer basic benefits than your current plan, or buy any Medicare Supplement Plan A, B, C*, F*, K, or L. You've had your current Medicare Supplement insurance plan for less than six months.
Is Medicare Supplement Plan F going away in 2020?
According to AARP, Medicare Supplement Plan F provides the most coverage, and as a result, it's the most popular plan among those eligible for Medicare. But with recent changes, Plan F is no longer available to everyone as of January 1, 2020.Jul 9, 2020
What is the difference between an Advantage plan and a supplemental plan?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.Oct 1, 2021
What is difference between Medigap and advantage?
Medigap is supplemental and helps to fill gaps by paying out-of-pocket costs associated with Original Medicare while Medicare Advantage plans stand in place of Original Medicare and generally provide additional coverage.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
When Am I Eligible For Medicare Supplement Coverage?
Because Medicare Supplement policies complement your Original Medicare coverage, you must be enrolled in Part A and Part B to be eligible for this...
How Can Enrollment Periods Affect My Eligibility For Medicare Supplement Plans?
The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period—for most people, this per...
Am I Eligible For A Medicare Supplement Plan If I’M Under Age 65?
Federal law does not require insurance companies to sell Medicare Supplement policies to people under 65, but many states do have this requirement....
Am I Eligible For A Medicare Supplement Plan If I Have A Medicare Advantage Plan?
Medicare Supplement policies don’t work with Medicare Advantage plans. If you decide to switch from Original Medicare to a Medicare Advantage plan,...
Am I Eligible For A Medicare Supplement Plan If I Have Coverage Through Medicaid?
While some beneficiaries may be eligible for both Medicare and Medicaid benefits (also known as “dual eligibles”), Medicaid typically doesn’t work...
How long does it take to apply for Medicare Supplement?
When to apply for a Medicare Supplement plan. Here's the quick answer: Most people should apply for a Medigap plan within six months of signing up for Part B. Medigap open enrollment begins when you sign up for Medicare Part B (at age 65) and lasts for six months. If you defer Part B coverage past age 65 because of health coverage ...
Is eligibility.com a Medicare provider?
Eligibility.com is a DBA of Clear Link Technologies, LLC and is not affiliated with any Medicare System Providers.
Does Medigap guarantee issue rights?
As you can see, Medigap guaranteed issue rights are incredibly valuable. Outside your open enrollment period, there are a few other scenarios where you have these rights as well. Typically these situations apply to you when you lose your existing coverage or after you try out Medicare Advantage.
Can you keep Medicare and Medigap together?
Be sure to keep your Medicare and Medigap cards together in a safe place. Your Medigap plan will be guaranteed renewable if you apply within your window of guaranteed issue rights. Guaranteed renewable means that as long as you continue to pay your premiums, you’ll keep your plan for as long as you’d like.
When to buy Medigap policy?
Buy a policy when you're first eligible. The best time to buy a Medigap policy is during your 6-month Medigap Open Enrollment Period. You generally will get better prices and more choices among policies. During that time you can buy any Medigap policy sold in your state, even if you have health problems. This period automatically starts the first ...
How long does it take for a pre-existing condition to be covered by Medicare?
Coverage for the pre-existing condition can be excluded if the condition was treated or diagnosed within 6 months before the coverage starts under the Medigap policy. After this 6-month period, the Medigap policy will cover the condition that was excluded. When you get Medicare-covered services, Original Medicare.
What is a select Medicare policy?
Medicare Select. A type of Medigap policy that may require you to use hospitals and, in some cases, doctors within its network to be eligible for full benefits. . If you buy a Medicare SELECT policy, you have rights to change your mind within 12 months and switch to a standard Medigap policy.
What is a copayment?
A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug. .
Can Medigap refuse to cover out-of-pocket costs?
A health problem you had before the date that new health coverage starts. . In some cases, the Medigap insurance company can refuse to cover your. out-of-pocket costs. Health or prescription drug costs that you must pay on your own because they aren’t covered by Medicare or other insurance.
Can you shorten the waiting period for a pre-existing condition?
It's possible to avoid or shorten waiting periods for a. pre-existing condition. A health problem you had before the date that new health coverage starts. if you buy a Medigap policy during your Medigap open enrollment period to replace ".
Can you get Medicare if you are 65?
Some states provide these rights to all people with Medicare under 65. Other states provide these rights only to people eligible for Medicare because of disability or only to people with ESRD. Check with your State Insurance Department about what rights you might have under state law.
How Medicare works with other insurance
Learn how benefits are coordinated when you have Medicare and other health insurance.
Retiree insurance
Read 5 things you need to know about how retiree insurance works with Medicare. If you're retired, have Medicare and have group health plan coverage from a former employer, generally Medicare pays first. Your retiree coverage pays second.
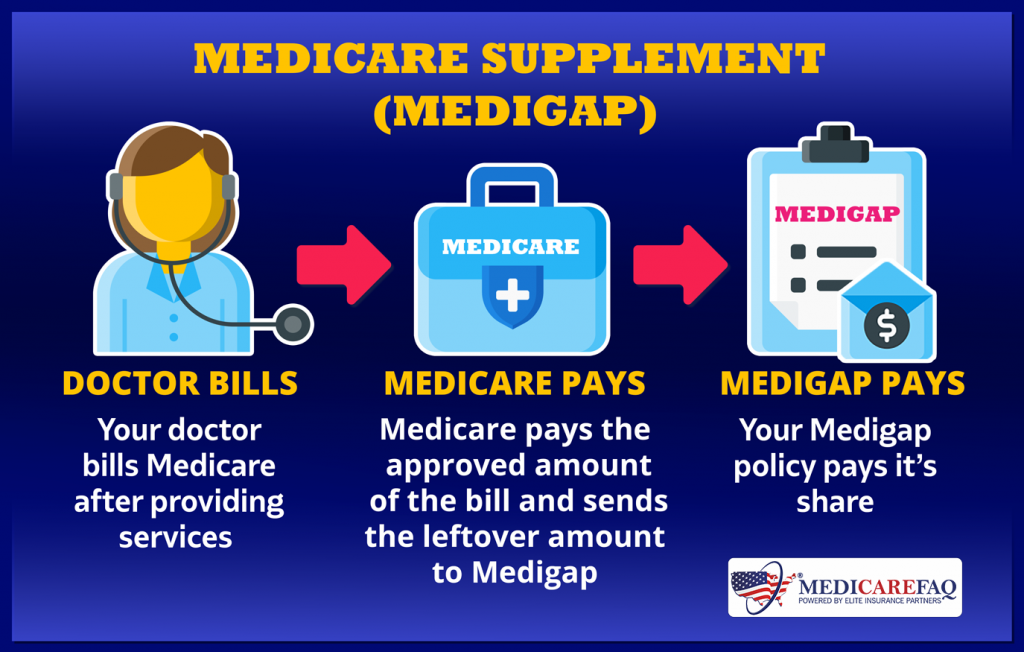
What's Medicare Supplement Insurance (Medigap)?
Read about Medigap (Medicare Supplement Insurance), which helps pay some of the health care costs that Original Medicare doesn't cover.
When can I buy Medigap?
Get the facts about the specific times when you can sign up for a Medigap policy.
How to compare Medigap policies
Read about different types of Medigap policies, what they cover, and which insurance companies sell Medigap policies in your area.
Medigap & travel
Read about which Medigap policies offer coverage when you travel outside the United States (U.S.).
What happens if you miss your Medicare open enrollment period?
Outside of the standard six-month Open Enrollment period, a Medicare Supplement policy could: come at a higher premium, be subject to underwriting, or coverage might not be available at all. 1
Is United American Insurance endorsed by the government?
The purpose of this communication is the solicitation of insurance. United American Insurance Company is not connected with, endorsed by, or sponsored by the U.S. government, federal Medicare program, Social Security Administration, or the Department of Health and Human Services. Policies and benefits may vary by state and have some limitations and exclusions. Individual Medicare Supplement insurance policy forms MSA10, MSB10, MSC10, MSD10, MSF10, MSHDF10, MSG10, MSHDG, MSK06R, MSL06R, MSN10 and in WI, MC4810 and MC4810HD, MC4810HDG are available from our Company where state-approved. Some states require these plans be available to persons under age 65 eligible for Medicare due to disability or End Stage Renal disease (ESRD). You may be contacted by an agent or producer representing United American Insurance Company, PO Box 8080, McKinney, TX 75070-8080. OUTLINE OF COVERAGE PROVIDED UPON REQUEST.
When is the AEP for Medicare?
The Annual Election Period (AEP), also called Fall Open Enrollment, October 15 – December 7 every year. The 5-Star Special Enrollment Period. You can switch to a Medicare prescription drug plan with a 5-star rating from December 8 one year to November 30 the next Read more about the 5-star special enrollment period.
What happens if you don't sign up for Medicare?
There’s another reason to think about signing up for Part D: if you don’t sign up when you’re first eligible for Medicare, you might have to pay a late enrollment penalty if you need medications at a later date and decide to sign up. Learn more about the Part D late enrollment penalty.
What is Medicare Part D?
Medicare Part D is prescription drug coverage , as you may know. You might decide you need this coverage, but when can you get it? We’ll fill you in on when and how to enroll in Medicare Part D. Find affordable Medicare plans in your area. Find Plans.
How long does Medicare Part D last?
The most common enrollment periods are: Your Medicare Initial Enrollment Period. For most people, this is the seven-month period that starts 3 months before the month you turn 65, includes the month you turn 65, and continues three months after that.
Can you get a different SEP?
You might qualify for a different Special Enrollment Period ( SEP) in some cases. Many SEPs involve losing your coverage. For example, if you have other creditable prescription drug coverage and your coverage ends, you might get an SEP when you can sign up for coverage under Medicare Part D. You might also be able to make other coverage changes ...
Do I have to sign up for Medicare Part D?
Medicare Part D is optional – you don’t have to sign up for it. Part D is the prescription drug coverage “part” of Medicare. But you don’t automatically get Part D, even if you’re one of the many who get enrolled in Medicare Part A and Part B automatically.
Does Medicare cover prescriptions?
Original Medicare, Part A and Part B, doesn’t include prescription drug coverage, except in certain cases. Part A usually covers medications given as part of your treatment when you’re a hospital inpatient. Part B may cover prescription drugs administered to you in an outpatient setting, such as a clinic. But when it comes to medications you take ...
When is a Medicare Supplement Guaranteed Issue?
Unlike private health insurance plans, applicants can purchase a Medicare Supplement with guaranteed issue rights, but not always.
When Can You be Denied Medicare Supplemental Insurance?
Although Medicare Supplement plans are generally not medically underwritten for most applicants, there are situations when you can be denied coverage. It’s all about the timing:
Can my Medicare Supplement Plan be non-Renewed?
Generally, Medicare Supplement (Medigap) policies are automatically renewed. But, there are certain circumstances when an insurance company can elect not to offer a renewal:
When are the Medicare Enrollment Deadlines?
For people who are receiving or eligible to receive Social Security benefits, Social Security will send you instructions for signing up three months before the month you turn 65. People who are receiving Social Security benefits will not be charged for Part A which covers hospital visits and services.
Can I Opt-Out of Original Medicare?
You can opt-out of Medicare Part B if you have primary health coverage through an employer, union, on a spouse’s plan, or are receiving veterans’ benefits but you should confirm with your health insurance provider that your plan will meet the Medicare standard.
What age do you have to be to get Medicare Supplement?
Disabled Under 65 . In 27 states, Medicare Supplement Insurance companies are required to sell policies to people under age 65 who receive Medicare benefits because of a qualifying disability or medical condition.
Do you have to have Medicare to be under 65?
State laws vary, but some states only require insurance companies to offer certain plans to people under 65. For example, Texas only requires companies to offer Medigap Plan A, which is the least comprehensive plan available. If you live in a different state, you may be denied altogether. Only the 27 states above are required to offer any Medicare ...
Do you pay more for Medigap than over 65?
You will probably pay more for your plan than people over 65. Some states require insurance companies to sell you a Medigap policy for the same price as people over 65, but most states allow companies to charge you more if you are under 65 and disabled. You may have to settle on a less comprehensive plan. State laws vary, but some states only ...