Full Answer
What is the deadline for Medicare supplement?
You may qualify for a Special Enrollment Period for a number of reasons, which can include:
- You moved to a new area that is outside of your current Medicare Advantage plan's service area
- You left your employer coverage
- Medicare ended your current Medicare Advantage plan's contract
Is there open enrollment for Medicare supplements?
Medicare open enrollment lasts from October 15 to December 7 each year ... Medicare Part D and Medicare Supplement insurance, so it’s your job to educate and help them determine which coverage combination best addresses their needs.
How to enroll in Medicare if you are turning 65?
- You have no other health insurance
- You have health insurance that you bought yourself (not provided by an employer)
- You have retiree benefits from a former employer (your own or your spouse’s)
- You have COBRA coverage that extends the insurance you or your spouse received from an employer while working
Is there a deadline for Medicare supplemental insurance?
When you switch from one Medicare Supplement insurance plan to another, you typically get 30 days to decide if you want to keep it. This 30-day free look period starts when you get your new Medicare Supplement insurance plan. You’ll need to pay the premiums for both your new plan and your old plan for one month.
Can I add a Medicare Supplement at any time?
One interesting feature of Medicare Supplement insurance plans is that you can apply for a plan anytime – you only need to be enrolled in Medicare Part A and Part B. However, a plan doesn't have to accept your application, unless you have guaranteed-issue rights.
How long do I have to enroll in a Medicare Supplement?
six monthsThe best time to enroll in a Medicare Supplement plan may be your Medicare Supplement Open Enrollment Period. This period lasts six months and begins the first day of the month in which you are both 65 or older and enrolled in Medicare Part B. For example, your birthday is August 31, 1953, so you turn 65 in 2018.
When should I start looking at Medicare plans?
Your first chance to sign up (Initial Enrollment Period) It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month.
Do you have to renew Medicare Supplement every year?
The plain and simple answer to this question is no, you don't have to renew your Medigap plan each year. All Medicare Supplement plans are guaranteed renewable for life as long as you're paying your premium, either monthly, quarterly, semi-annually, or annually.
Can you have a Medicare Advantage plan and a supplemental plan at the same time?
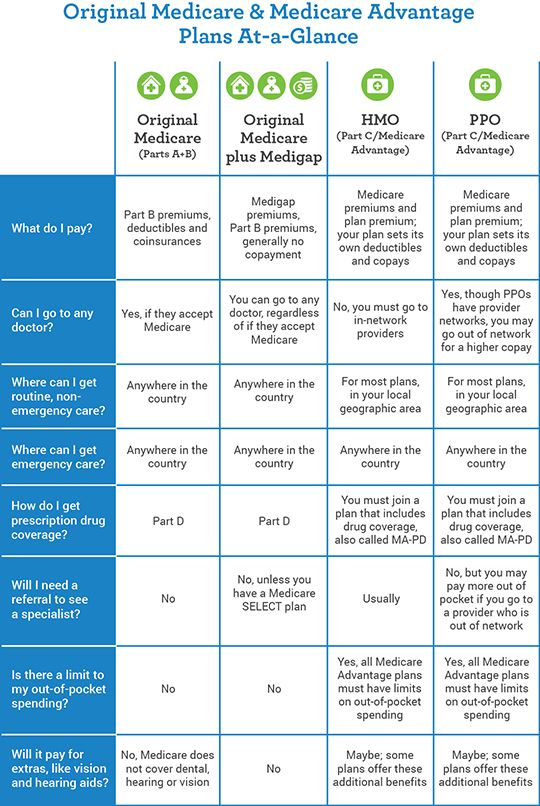
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.
What do I need to do before I turn 65?
Turning 65 Soon? Here's a Quick Retirement ChecklistPrepare for Medicare. ... Consider Additional Health Insurance. ... Review Your Social Security Benefits Plan. ... Plan Ahead for Long-Term Care Costs. ... Review Your Retirement Accounts and Investments. ... Update Your Estate Planning Documents.
Does Medicare become effective on your 65th birthday?
Can I start Medicare before my 65th birthday? You will have a Medicare initial enrollment period. If you sign up for Medicare Part A and Part B during the first three months of your initial enrollment period, your coverage will start on the first day of the month you turn 65.
Do you automatically get a Medicare card when you turn 65?
You should receive your Medicare card in the mail three months before your 65th birthday. If you are NOT receiving benefits from Social Security or the RRB at least four months before you turn 65, you will need to sign up with Social Security to get Parts A and B.
When Am I Eligible For Medicare Supplement Coverage?
Because Medicare Supplement policies complement your Original Medicare coverage, you must be enrolled in Part A and Part B to be eligible for this...
How Can Enrollment Periods Affect My Eligibility For Medicare Supplement Plans?
The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period—for most people, this per...
Am I Eligible For A Medicare Supplement Plan If I’M Under Age 65?
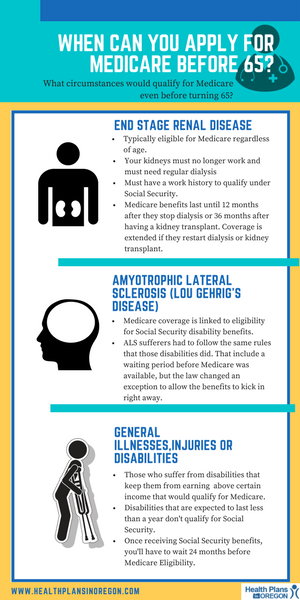
Federal law does not require insurance companies to sell Medicare Supplement policies to people under 65, but many states do have this requirement....
Am I Eligible For A Medicare Supplement Plan If I Have A Medicare Advantage Plan?
Medicare Supplement policies don’t work with Medicare Advantage plans. If you decide to switch from Original Medicare to a Medicare Advantage plan,...
Am I Eligible For A Medicare Supplement Plan If I Have Coverage Through Medicaid?
While some beneficiaries may be eligible for both Medicare and Medicaid benefits (also known as “dual eligibles”), Medicaid typically doesn’t work...
What is Medicare Supplement Insurance?
Medicare Supplement Insurance (Medigap or MedSup), sold by private companies, helps pay some health care costs that Original Medicare (Part A and Part B) doesn’t cover. Policies can include coverage for deductibles, coinsurance, hospital costs, skilled nursing facility costs, and sometimes health care costs when traveling outside the U.S.
How long is the free look period for Medigap?
If you’re within your six-month Medigap Open Enrollment Period and considering a different Medigap plan, you may try a new Medigap policy during a 30-day “free look period.”. During this period, you will have two Medigap plans, and pay the premium for both.
What happens if a Medigap policy goes bankrupt?
Your Medigap insurance company goes bankrupt and you lose your coverage , or your Medigap policy coverage otherwise ends through no fault of your own. You leave a Medicare Advantage plan or drop a Medigap policy because the company hasn’t followed the rules, or it misled you.
What Are Medicare Supplement Plans?
Since 2014, nearly 4 million people have purchased a Medicare Supplement Plan. But what are they, and why are they becoming more popular for people on Medicare?
Who Is Eligible to Enroll in a Medicare Supplement Plan?
Anyone who is eligible for Original Medicare coverage can buy Medicare Supplement Insurance.
When to Apply for Your Medicare Supplement Plan
Purchasing a Medicare Supplement Plan can be a stressful process, but signing up at the right time will ensure:
Medicare Supplement Open Enrollment Period
Your Medicare Supplement Plan Open Enrollment Period (also known as your Medigap Open Enrollment Period) is a one-time six month period when you can sign up for a Medicare Supplement Plan without having to worry about your health status or chronic conditions.
Special Enrollment Periods and Medicare Supplement Plans
Usually, a person will only get one opportunity to benefit from their Medigap Open Enrollment Period.
Applying at Any Time for a Medicare Supplement Plan
You can also purchase Medicare Supplement Insurance outside of your Medicare Supplement Open Enrollment Period, but remember that insurance companies don’t have to accept you as a member.
Choosing the Right Medicare Supplement Plan Can Make All the Difference
It’s also important to consider the type of cover you get when you sign up for a Medicare Supplement Plan.
When to buy Medigap policy?
Buy a policy when you're first eligible. The best time to buy a Medigap policy is during your 6-month Medigap Open Enrollment Period. You generally will get better prices and more choices among policies. During that time you can buy any Medigap policy sold in your state, even if you have health problems. This period automatically starts the first ...
How long does it take for a pre-existing condition to be covered by Medicare?
Coverage for the pre-existing condition can be excluded if the condition was treated or diagnosed within 6 months before the coverage starts under the Medigap policy. After this 6-month period, the Medigap policy will cover the condition that was excluded. When you get Medicare-covered services, Original Medicare.
What is a select Medicare policy?
Medicare Select. A type of Medigap policy that may require you to use hospitals and, in some cases, doctors within its network to be eligible for full benefits. . If you buy a Medicare SELECT policy, you have rights to change your mind within 12 months and switch to a standard Medigap policy.
Can you shorten the waiting period for a pre-existing condition?
It's possible to avoid or shorten waiting periods for a. pre-existing condition. A health problem you had before the date that new health coverage starts. if you buy a Medigap policy during your Medigap open enrollment period to replace ".
Can you get Medicare if you are 65?
Some states provide these rights to all people with Medicare under 65. Other states provide these rights only to people eligible for Medicare because of disability or only to people with ESRD. Check with your State Insurance Department about what rights you might have under state law.
Can you charge more for a Medigap policy?
Charge you more for a Medigap policy. In some cases, an insurance company must sell you a Medigap policy, even if you have health problems. You're guaranteed the right to buy a Medigap policy: When you're in your Medigap open enrollment period. If you have a guaranteed issue right.
How long does it take to apply for Medicare Supplement?
When to apply for a Medicare Supplement plan. Here's the quick answer: Most people should apply for a Medigap plan within six months of signing up for Part B. Medigap open enrollment begins when you sign up for Medicare Part B (at age 65) and lasts for six months. If you defer Part B coverage past age 65 because of health coverage ...
Is eligibility.com a Medicare provider?
Eligibility.com is a DBA of Clear Link Technologies, LLC and is not affiliated with any Medicare System Providers.
Does Medigap guarantee issue rights?
As you can see, Medigap guaranteed issue rights are incredibly valuable. Outside your open enrollment period, there are a few other scenarios where you have these rights as well. Typically these situations apply to you when you lose your existing coverage or after you try out Medicare Advantage.
Can you keep Medicare and Medigap together?
Be sure to keep your Medicare and Medigap cards together in a safe place. Your Medigap plan will be guaranteed renewable if you apply within your window of guaranteed issue rights. Guaranteed renewable means that as long as you continue to pay your premiums, you’ll keep your plan for as long as you’d like.
What is Medicare Supplement Open Enrollment Period?
What is Medicare Supplement Open Enrollment? Medicare Supplement Open Enrollment Period is a once in a lifetime window that allows you to enroll in any Medigap plan without answering health questions.
Why do people delay enrolling in Medicare Supplement?
For some; they choose to delay enrolling in Part B due to still working and having creditable coverage with their employer. When they do retire and enroll in Part B, they will initiate their Medicare Supplement Open Enrollment Period.
What happens if you miss your Medigap open enrollment period?
When you miss your Medigap Open Enrollment Period and are denied coverage, there are alternative options. If you have a serious health condition that causes a Medigap carrier not to accept you, you should be able to enroll in a Medicare Advantage plan.
How long does Medicare open enrollment last?
Applying outside your open enrollment window can result in higher premiums, as well as restrict your coverage options. This window only lasts for six months for each new beneficiary, unless you delay enrollment into Part B due to having other creditable coverage.
Does timing affect Medigap coverage?
Timing can affect how much you pay for coverage; how easy coverage is to obtain, and it can significantly determine the options available to you. The Megiap OEP is the only time you’ll ever get that allows you to enroll in any Medigap letter plan. You’ll be able to avoid having to answer any health questions.
Which states have open enrollment?
Some states have unique open enrollment rules, like Connecticut and California. In California, they have a birthday rule that allows you to enroll days surrounding your birthday without answering health questions. In Connecticut, they have a year-round open enrollment window for all beneficiaries.
Can you get insurance if you enroll in one time?
If they enroll as soon as their first eligible, during the one-time individual open enrollment window, these health problems will not prevent them from getting coverage.
Do I Have To Sign Up For Medicare If Im Still Working At 65
Medicare Supplement Plans: When to Sign-Up and Avoid the Biggest Mistake!
Cant Get A Medigap Policy Try Medicare Advantage
If no insurer will sell you a Medigap policy, you have an option. Medicare Advantage is another private health plan that can save you money. Plans have a maximum limit on out-of-pocket costs, typically $5,000. Some plans even have no monthly premium.
Medicare Late Enrollment Penalties
If you do not take the corresponding action above that reflects your situation, you may be faced with Medicare late enrollment penalties. These penalties are dual in nature you may receive a financial penalty as well as be restricted on when you can get into Medicare.
When Can You Sign Up For Medicare Supplement Plans
When it comes to Medicare Supplement plans, you can join at any time of the year. If your Open Enrollment window has passed, you can still apply. However, youll most likely have to go through medical underwriting and answer health questions during the application process.
How Do I Choose Medicare Supplement Insurance
Insurance companies label Medigap plans with a letter to show what benefits are included. For example, according to Medicare.gov, Medigap Plan F will pay for health care during foreign travel but Plan A will not.
What If I Miss My Medicare Supplement Open Enrollment Period
When you miss your Medigap Open Enrollment Period and are denied coverage, there are alternative options. If you have a serious health condition that causes a Medigap carrier not to accept you, you should be able to enroll in a Medicare Advantage plan.
Who Is Eligible For Supplemental Insurance
Anyone who has Medicare Part A and Part B is eligible to apply for a Medicare supplement plan. However, you need to qualify for coverage with the private insurance company. When you first turn 65 and sign up for Medicare Part B, you have a Medigap open enrollment period that lasts six months.
What happens if you miss your Medicare open enrollment period?
Outside of the standard six-month Open Enrollment period, a Medicare Supplement policy could: come at a higher premium, be subject to underwriting, or coverage might not be available at all. 1
Is United American Insurance endorsed by the government?
The purpose of this communication is the solicitation of insurance. United American Insurance Company is not connected with, endorsed by, or sponsored by the U.S. government, federal Medicare program, Social Security Administration, or the Department of Health and Human Services. Policies and benefits may vary by state and have some limitations and exclusions. Individual Medicare Supplement insurance policy forms MSA10, MSB10, MSC10, MSD10, MSF10, MSHDF10, MSG10, MSHDG, MSK06R, MSL06R, MSN10 and in WI, MC4810 and MC4810HD, MC4810HDG are available from our Company where state-approved. Some states require these plans be available to persons under age 65 eligible for Medicare due to disability or End Stage Renal disease (ESRD). You may be contacted by an agent or producer representing United American Insurance Company, PO Box 8080, McKinney, TX 75070-8080. OUTLINE OF COVERAGE PROVIDED UPON REQUEST.
Can I get Medicare Supplement at 65?
If you're under age 65 and have Original Medicare, you may not be able to enroll in Medicare Supplement. 2 Federal law does not require insurance companies to offer Medicare Supplement insurance coverage to Medicare beneficiaries under age 65 2; however, some states require insurance companies to offer certain plans to applicants under age 65 on Medicare due to special circumstances.
When does Medicare change coverage?
You can’t use this Special Enrollment Period from October–December. However, all people with Medicare can make changes to their coverage from October 15–December 7, and the changes will take effect on January 1.
What can I do with my Medicare Advantage Plan?
What can I do? Join a Medicare Advantage Plan with drug coverage or a Medicare Prescription Drug Plan. Switch from your current plan to another Medicare Advantage Plan with drug coverage or a Medicare Prescription Drug Plan. Drop your Medicare Advantage Plan with drug coverage and return to Original Medicare .
What is a special enrollment period?
Special circumstances (Special Enrollment Periods) You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles).
What to do if you made wrong choice on Medicare?
Call center representatives can help you throughout the year with options for making changes.
How long does it take to switch plans after moving?
If you tell your plan before you move, your chance to switch plans begins the month before the month you move and continues for 2 full months after you move. If you tell your plan after you move, your chance to switch plans begins the month you tell your plan, plus 2 more full months.