Can I change Medicare Advantage plans anytime?
- The Annual Election Period (AEP), also called Fall Open Enrollment, October 15 – December 7 every year.
- The Medicare Advantage Open Enrollment Period, January 1 – March 31 every year, starting in 2019.
- The 5-Star Special Enrollment Period. ...
- Other Special Enrollment Periods, if applicable. ...
How often can I change Medicare plans?
Jun 03, 2020 · This period lasts from January 1 to March 31 each year, and during this time, you can make one change to your healthcare coverage. You can switch to an alternative Medicare Advantage plan, with or without prescription drug coverage, or you can revert to Original Medicare (and enroll in a stand-alone prescription drug plan). If you make a change during the Medicare …
What to know when selecting a Medicare plan?
To switch to Original Medicare, contact your current plan, or call us at 1-800-MEDICARE. Unless you have other drug coverage, you should carefully consider Medicare prescription drug coverage (Part D). You may also want to consider a Medicare Supplement Insurance (Medigap) policy. Remember, you may only be able to switch at certain times of the year.
When is the deadline for changing Medicare plans?
If you have a Medicare Advantage plan, however, you can make changes to your Part D coverage during the Medicare Advantage Open Enrollment Period, which runs from January 1 to March 31 each year. You can also sign up for Part D coverage during this period if you’re switching from a Medicare Advantage plan back to Original Medicare (Parts A and B).
How and when to change Medicare plans?
Aug 20, 2021 · You can change from your current Part D plan to a different one during the Medicare open enrollment period, which runs from October 15 to December 7 each year. During the open enrollment period, you can change plans as often as you want. Your final choice will take effect on January 1. of the following year.

When can you change Medicare Supplement Plans?
You can change your Medicare Supplement Plan at any time. However, if you have health issues that could cause a rate increase of denial of coverage...
What is the Medicare free look period?
Most companies will allow you a free-look period for thirty days when you can examine and use your plan. If you find your plan unsatisfactory, you...
Can Medicare Supplement Insurance plan be Cancelled?
Generally, no. Your insurance company cannot cancel your Medicare Supplement insurance plans unless you don't make your premium payments or the ins...
Can I change my Medicare Part D plan anytime?
You can change from your current Part D plan to a different one during the Medicare open enrollment period, which runs from October 15 to December...
How to switch to Medicare Advantage?
To switch to a new Medicare Advantage Plan, simply join the plan you choose during one of the enrollment periods. You'll be disenrolled automatically from your old plan when your new plan's coverage begins. To switch to Original Medicare, contact your current plan, or call us at 1-800-MEDICARE. Unless you have other drug coverage, you should ...
What happens if you lose Medicare coverage?
In other cases, you may still be able to use your employer or union coverage along with the Medicare Advantage plan you join.
What to Do if You Missed Medicare Annual Enrollment Period
If you miss the Medicare Annual Enrollment Period, there are a few circumstances in which you are allowed to change your coverage. Each year, there are five set times you can enroll in Medicare or change existing Medicare plans:
When can I change my Medicare Supplement Insurance plan?
There are limited circumstances in which you can change your Medicare Supplement plan, also known as Medigap. If you’re still within your Initial Enrollment Period (three months before and three months after your birth month), you have the option to switch your coverage.
When can I change my Medicare Part D plan?
In most cases, you can only make changes to your Medicare Part D coverage during the Annual Enrollment Period. If you have a Medicare Advantage plan, however, you can make changes to your Part D coverage during the Medicare Advantage Open Enrollment Period, which runs from January 1 to March 31 each year.
How to Change Medicare Plans During a Medicare Enrollment Period
If you are eligible to change your Medicare plan during one of the Medicare enrollment periods, SelectQuote can help you do so. We can help you understand your options for coverage and find a plan that includes the benefits you need at a price that fits your budget.
Want to switch Medicare plans? Let SelectQuote compare Medicare plans for you
If you need help understanding your enrollment and coverage options, save yourself time and the hassle of navigating the Medicare maze on your own. In just minutes, we can compare Medicare plans available to you from some of the most trusted insurance companies in the nation.
Reasons to Consider Changing Your Medicare Supplement Plan
As was mentioned earlier, when Medicare beneficiaries purchase a Medicare Supplement plan, the decision on which plan to purchase is based on the healthcare services you generally need at that time and your budget for purchasing coverage.
Is it Possible to avoid Medical Underwriting outside of the Open Enrollment Period?
The short answer is YES but you must be eligible under one of the following qualifiers:
Can I switch from a Medicare Supplement to a Medicare Advantage Plan?
Yes, you can switch from your Medigap plan to a Medicare Advantage plan between October 15 and December 7, which is the annual enrollment period.
Is your healthcare plan still meeting your healthcare needs?
Are changes to your current Medicare plan costing you a little bit more this year? Are you taking any new drugs that may cost less on another plan? Is your doctor still in your plan’s network? Plans can change from year to year. Maybe it’s time to consider your options.
Are you missing out on any new Medicare Advantage benefits?
Most of our Medicare Advantage plans now include coverage for prescription drugs. Many include coverage for routine dental, vision and hearing care, as well—benefits not provided by Original Medicare.
Making the switch is simple
If you currently have Original Medicare and switch to a Medicare Advantage plan, your new health insurance plan will be activated on Jan. 1.
When does Medicare open enrollment period end?
If you’re enrolled in Medicare Advantage and want to switch back to Original Medicare, Part A and Part B, you can do so during the Medicare Advantage Open Enrollment Period (OEP), which runs from January 1-March 31 each year. You will also have until March 31 to join a stand-alone Medicare Prescription Drug Plan (Part D), and your coverage will go into effect the first day of the month after your new plan gets your enrollment form.
Can you change Medicare plans during a special election?
Medicare has certain provisions to help you deal with unexpected happenings. If you go through certain special circumstances, you may be able to change Medicare plans during Special Election Periods. These events may include, but aren’t limited to:
When is the Medicare Advantage open enrollment period?
The Medicare Advantage Open Enrollment Period, January 1 – March 31 every year, starting in 2019. The 5-Star Special Enrollment Period. You can switch to a Medicare Advantage plan with a 5-star rating between December 8 one year and November 30 the next year.
Does Medicare cover prescription drugs?
Here are just a few. Many – but not all – Medicare Advantage plans cover prescription drugs. Some Medicare Advantage plans give you extra benefits, like routine dental or hearing care. Some plans may require you to use doctors in the plan’s provider network, or pay more if you go outside the network. Premiums vary among plans.
When do insurance companies send out notices of changes to Medicare?
Every September, insurance companies must send out a Medicare Annual Notice of Change (ANOC) letter to Medicare beneficiaries. This letter tells you of any changes to your rates. If your rates go up, you may want to consider looking for a new policy.
How long do you have to wait to switch Medigap?
Your insurance company may agree to sell you a new policy with the same basic benefits, but you may have to wait up to six months before the new plan covers any pre-existing health conditions . If any of the above situations apply to you, you can switch Medigap plans without medical underwriting.
How to avoid medical underwriting?
The main way to avoid medical underwriting is if you have a Medicare Supplement insurance guaranteed-issue right. Some guaranteed-issue rights occur when: Your Medigap insurance company went bankrupt or ended your policy through no fault of your own.
What happens if you don't change your Medicare Supplement?
If you don't change Medicare Supplement insurance plans during your Medigap Open Enrollment Period, your insurer can force you to undergo medical underwriting, and they can now assess your health history during the application process and can turn you down if it chooses.
What is a Medicare Supplement Plan?
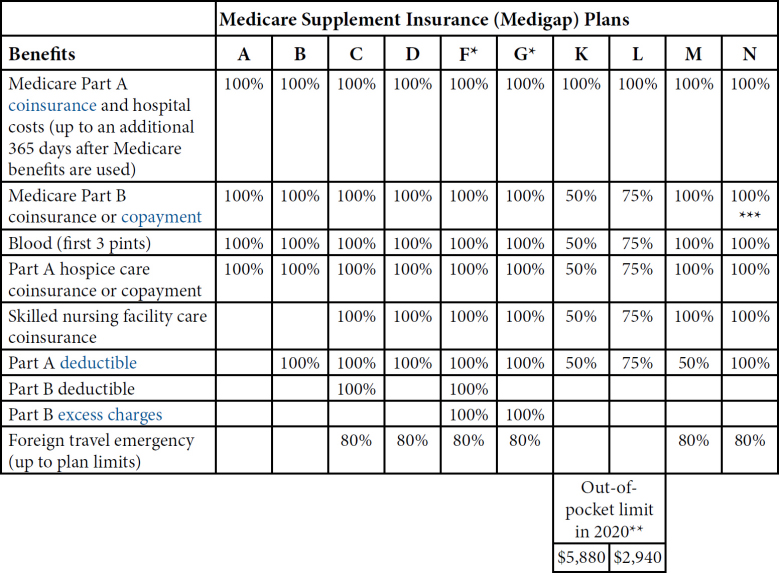
Medigap plans are designed to fill those gaps by supplementing your Original Medicare coverage to pay for certain out-of-pocket costs. A Medicare Supplement plan may pay your coinsurance or copayments from Medicare Part A and Part B.
What to do if you are unhappy with your Medicare Supplement?
If you are unhappy with your insurance company for any reason, you can purchase a plan from a different insurance underwriter. Call to speak with a licensed insurance agent who can help you compare Medicare Supplement plans in your area. They can help you change plans once you find the best plan for your needs.
How long do you have to keep Medicare Supplement?
The Medicare Supplement “Free Look” Period. When you switch Medicare Supplement Insurance plans, you generally are allowed 30 days to decide to keep it or not. This 30-day “free look” period starts when your new Medicare Supplement plan takes effect.
How to switch Medigap insurance?
How to switch Medigap policies. Call the new insurance company and arrange to apply for your new Medigap policy. If your application is accepted, call your current insurance company, and ask for your coverage to end. The insurance company can tell you how to submit a request to end your coverage.
How long do you have to have a Medigap policy?
If you've had your Medicare SELECT policy for more than 6 months, you won't have to answer any medical questions.
What happens if you buy a Medigap policy before 2010?
If you bought your policy before 2010, it may offer coverage that isn't available in a newer policy. If you bought your policy before 1992, your policy: Might not be a Guaranteed renewable policy. May have a bigger Premium increase than newer, standardized Medigap policies currently being sold. expand.
How long is the free look period for Medigap?
Medigap free-look period. You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period.". The 30- day free look period starts when you get your new Medigap policy. You'll need to pay both premiums for one month.
Can you exclude pre-existing conditions from a new insurance policy?
The new insurance company can't exclude your Pre-existing condition. If you've had your Medigap policy less than 6 months: The number of months you've had your current Medigap policy must be subtracted from the time you must wait before your new Medigap policy covers your pre-existing condition.
Does Medicare cover Part B?
As of January 1, 2020, Medigap plans sold to new people with Medicare aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on January 1, 2020.
Can I keep my Medigap policy if I move out of state?
I'm moving out of state. You can keep your current Medigap policy no matter where you live as long as you still have Original Medicare. If you want to switch to a different Medigap policy, you'll have to check with your current or new insurance company to see if they'll offer you a different policy. If you decide to switch, you may have ...