When can I Change my Medicare supplement plan?
When can I change my Medicare Supplement Plan? Medicare beneficiaries can make changes to parts of their Medicare coverage – including their Medicare Advantage (Part C) and Prescription Drug Plans (Part D) – during Medicare’s Annual Enrollment Period (AEP) which takes place every year from October 15th to December 7th.
How old do you have to be to buy Medicare supplement plans?
In order to purchase a Medicare Supplement plan, you must be 65 years of age and enrolled in Part B. To be eligible for Medicare, you must be at least 65 years old, a citizen of the United States or permanent legal resident for at least five consecutive years.
Can I buy Medicare supplement insurance if I have Medicare Part C?
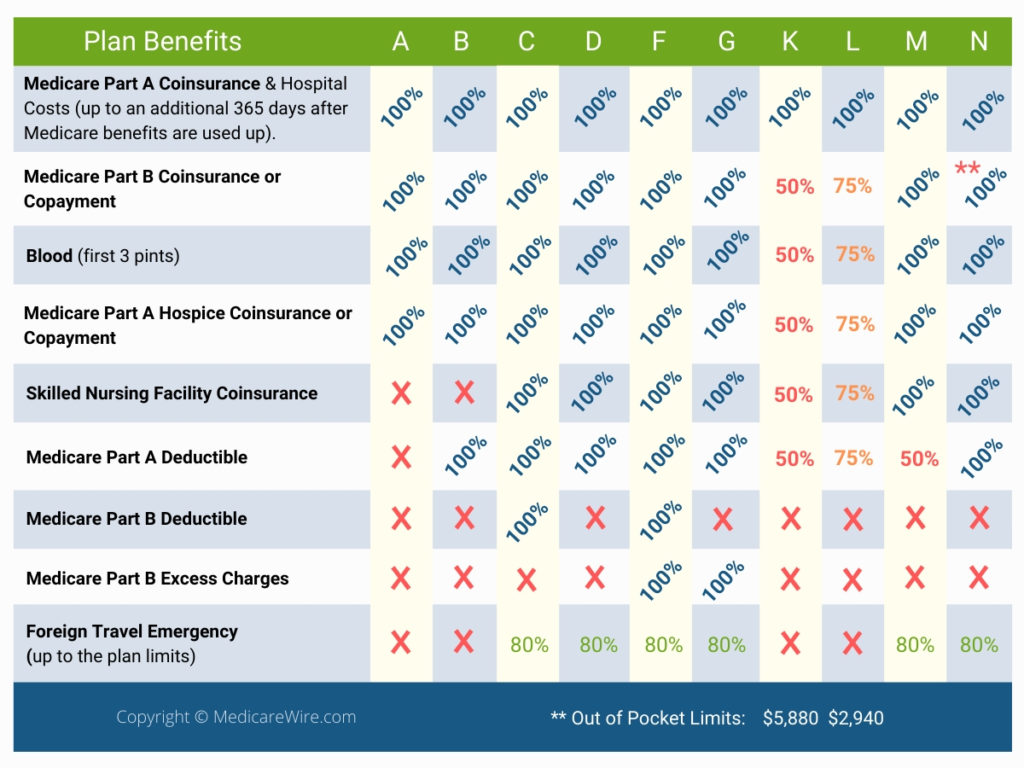
If you have a Part C plan, you cannot purchase a Medicare Supplement insurance plan. Each plan varies in what it covers, but all plans pay for Medicare Part A (hospital insurance) coinsurances for up to 365 days beyond the coverage that Medicare offers.
What is a Medicare supplement insurance policy?
These supplemental plans may include those that are provided by an employer, Medigap plans, or supplemental health care coverage through Medicaid. Medicare supplement insurance policies help fill in the gaps left by Original Medicare health care insurance.

How long do I have to pick a Medicare Supplement?
Within six months of beginning to receive Medicare Part B benefits — regardless of whether you enroll in Part B at age 65 or delay enrollment until you (or your spouse) stop working for an employer that provides health insurance. This six-month “open enrollment” period for Medigap is a once-only opportunity.
When can you switch from an Advantage plan to a supplemental plan?
Once you've left your Medicare Advantage plan and enrolled in Original Medicare, you are generally eligible to apply for a Medicare Supplement insurance plan.
At what age does the open enrollment period typically begin for Medicare Supplement coverage?
65 or olderI'm 65 or older. Your Medigap open enrollment period begins when you enroll in Part B and can't be changed or repeated. In most cases, it makes sense to enroll in Part B when you're first eligible, because you might otherwise have to pay a Part B late enrollment penalty.
Can I be denied a Medicare Supplement plan?
For the most part, Medicare Supplement policies are guaranteed renewal. This means as long as you pay the monthly premium, you cannot be denied coverage once you enroll in a plan, regardless of any health conditions that may arise.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Can I switch Medicare Supplement plans anytime?
As a Medicare beneficiary, you can change supplements at any time. As a result, there's no guarantee an application will be accepted if switched outside the designated Open Enrollment Period. An application may be “medically underwritten”.
What changes are coming to Medicare in 2022?
Changes to Medicare in 2022 include a historic rise in premiums, as well as expanded access to mental health services through telehealth and more affordable options for insulin through prescription drug plans. The average cost of Medicare Advantage plans dropped while access to plans grew.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
Do Medicare Supplement plans cover pre existing conditions?
The pre-existing condition waiting period “ This means that you may have to pay all your own out-of-pocket costs for your pre-existing condition for up to six months. After the waiting period, the Medicare Supplement insurance plan may cover Medicare out-of-pocket costs relating to the pre-existing condition.
Do Medigap plans have out-of-pocket limits?
Do Medigap Plans have an Out-of-Pocket Maximum? Medigap plans don't have a maximum out-of-pocket because they don't need one. The coverage is so good you'll never spend $5,000 a year on medical bills.
Can I be turned down for Medicare Part D?
To disenroll from a Medicare drug plan during Open Enrollment, you can do one of these: Call us at 1-800 MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Mail or fax a signed written notice to the plan telling them you want to disenroll.
What does my supplemental insurance cover?
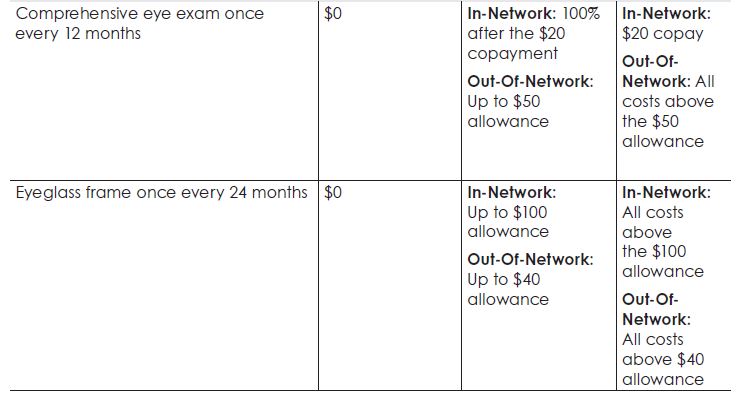
Some supplemental insurance plans will pay for the out-of-pocket cost-sharing that goes along with your health insurance plan (ie, deductibles, copayments, and coinsurance), or for medical services that your health plan doesn't cover at all, such as dental and vision costs.
Medicare Supplement Program: Fast Facts
Medicare Supplement insurance provides coverage for copayments, coinsurance, deductibles, and other expenses not covered by Original Medicare .
Medigap Plan C And Plan F Changed In 2020
A slight but important change was made to the selection of standardized Medigap plans available in most states.
If You Are Under 65 And Have Medicare Due To Disability
Federal law does not give you the same protections that are given to people 65 and older when buying Medigap. Therefore, whether you can buy any Medigap policy or one that is affordable depends on your own states law.
Can I Buy A Medigap Plan After My Enrollment Initial Window Closes
After your six-month open enrollment window, Medigap plans are medically underwritten in nearly every state, meaning that if you apply for coverage outside of your open enrollment window, you can be declined or charged more based on your medical history.
When Can You Enroll In A Medicare Supplement Plan Or Medigap Policy
If youre thinking about joining a Medicare Supplement Plan or Medigap policy, figuring out when to enroll can be difficult.
What Happens If I Miss My Medicare Supplement Open Enrollment Period
Your eligibility may be impacted if you miss the Medicare Supplement Open Enrollment Period:
Important Enrollment Dates And Qualifications For Medicare Supplement Plans
While you can switch to a new plan at any time, its wise to be strategic about when you enroll in a Medigap plan, change your plan, or drop the plan entirely.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
Can you cancel a Medigap policy?
This means the insurance company can't cancel your Medigap policy as long as you pay the premium. Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
How Medicare works with other insurance
Learn how benefits are coordinated when you have Medicare and other health insurance.
Retiree insurance
Read 5 things you need to know about how retiree insurance works with Medicare. If you're retired, have Medicare and have group health plan coverage from a former employer, generally Medicare pays first. Your retiree coverage pays second.
What's Medicare Supplement Insurance (Medigap)?
Read about Medigap (Medicare Supplement Insurance), which helps pay some of the health care costs that Original Medicare doesn't cover.
When can I buy Medigap?
Get the facts about the specific times when you can sign up for a Medigap policy.
How to compare Medigap policies
Read about different types of Medigap policies, what they cover, and which insurance companies sell Medigap policies in your area.
Medigap & travel
Read about which Medigap policies offer coverage when you travel outside the United States (U.S.).
What is Medicare Supplement Insurance?
Medicare Supplement Insurance (Medigap or MedSup), sold by private companies, helps pay some health care costs that Original Medicare (Part A and Part B) doesn’t cover. Policies can include coverage for deductibles, coinsurance, hospital costs, skilled nursing facility costs, and sometimes health care costs when traveling outside the U.S.
How long is the free look period for Medigap?
If you’re within your six-month Medigap Open Enrollment Period and considering a different Medigap plan, you may try a new Medigap policy during a 30-day “free look period.”. During this period, you will have two Medigap plans, and pay the premium for both.
What happens if a Medigap policy goes bankrupt?
Your Medigap insurance company goes bankrupt and you lose your coverage , or your Medigap policy coverage otherwise ends through no fault of your own. You leave a Medicare Advantage plan or drop a Medigap policy because the company hasn’t followed the rules, or it misled you.
When to enroll in Medicare Supplement Plan?
When to enroll in a Medicare Supplement plan. The best time to enroll in a Medicare Supplement plan is during your Medicare Supplement Open Enrollment Period, the six-month period that starts when you’re 65 or older and enrolled in Medicare Part B. During this time frame, you have “ guaranteed issue rights ,” meaning you have a guaranteed right ...
How long do you have to wait to get Medicare Supplement?
In certain cases, insurance companies may make you wait up to six months before covering pre-existing conditions, known as a “pre-existing condition waiting period.”. After this waiting period is over, the Medicare Supplement plan will cover all of your health conditions. However, if you enroll when you have a guaranteed issue right, ...
Does Medicare Supplement cover coinsurance?
Medicare Supplement plans work alongside your Medicare Part A and Part B benefits to help pay for costs that Medicare doesn’t cover, like copayments, coinsurance, deductibles, and overseas travel coverage. Here’s an overview on how the timing of your enrollment affects your Medicare Supplement coverage.
Can Medicare deny you coverage?
Deny you coverage based on your health status. If you’re trying to enroll in a Medicare Supplement plan for the first time, it could be hard for you to find a plan that will accept you when you have pre-existing health conditions. And even if you’re already enrolled in a Medicare Supplement plan, it may be more difficult to switch ...
Can you get a guaranteed issue with Medicare?
You may have guaranteed-issue rights in some situations, like if you’re in a Medicare Advantage plan and move out of the plan’s area of service, or your Medicare Advantage plan leaves Medicare. But for the most part, you’ll generally have more limited options when it comes to the Medicare Supplement plans available to you.
Can you use medical underwriting to sell Medicare?
Medical underwriting can’t be used by the insurance company when deciding whether to sell you a Medicare Supplement plan. Your health status or pre-existing conditions can’t be taken into consideration when determining Medicare Supplement plan premiums. The insurance company must cover all of your pre-existing conditions.
How to know if you have a Medicare Supplement?
To determine whether or not you have a Medicare Supplement plan, check out your insurance card. You’ll likely see the word “Supplement,” also with a “Plan A”, “Plan G”, or another combination of “Plan” and a letter. Wisconsin, Minnesota, and Massachusetts have their own standardization method.
How long does it take to disenroll from Medicare?
You decide to disenroll from a Medicare Advantage plan during a 12-month trial period. There are two times this happens.
What happens if you miss your chance to enroll in Medicare at age 65?
If you miss your chance to enroll at age 65, then you don’t have to worry about open enrollment just yet. For example – if you’re 66 years old but have never enrolled in Medicare Part B because you are currently covered by an employer health plan – then your Medigap Open Enrollment Period has not yet occurred.
How long does the Medigap open enrollment period last?
covered under Medicare Part B. Your Medigap Open Enrollment Period then lasts for a total of six months.
What happens if you miss the open enrollment deadline?
If you miss your 6-month open enrollment deadline, many insurers will still offer you coverage. However, insurers will be free to deny your application or charge higher monthly payments. In all cases, Medicare Supplement plans are renewable for life once you’ve enrolled in the plan.
What happens if you miss your Medigap enrollment?
If you miss your Medigap Open Enrollment Period, you may be subject to medical underwriting. This means that your application could be denied by the insurance company offering the plan. Your application could also be accepted at a higher price than you were hoping to spend.
How long does Medicare cover a condition?
While your Medicare Supplement plan can’t pick and choose which health issues to cover, your plan can delay coverage for conditions that were diagnosed or treated during the six months before you enroll and for up to six months after you enroll.
Your first chance to sign up (Initial Enrollment Period)
Generally, when you turn 65. This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65.
Between January 1-March 31 each year (General Enrollment Period)
You can sign up between January 1-March 31 each year. This is called the General Enrollment Period. Your coverage starts July 1. You might pay a monthly late enrollment penalty, if you don’t qualify for a Special Enrollment Period.
Special Situations (Special Enrollment Period)
There are certain situations when you can sign up for Part B (and Premium-Part A) during a Special Enrollment Period without paying a late enrollment penalty. A Special Enrollment Period is only available for a limited time.
Joining a plan
A type of Medicare-approved health plan from a private company that you can choose to cover most of your Part A and Part B benefits instead of Original Medicare. It usually also includes drug coverage (Part D).
When does Medicare open enrollment start?
You may also switch from Medicare Advantage to Original Medicare (and a Medicare Part D prescription drug plan, if you want one) during the Medicare Advantage Open Enrollment Period, which runs from January 1st to March 31st each year.
Can Medicare Advantage charge a higher premium?
Even if they choose to cover you, they can charge you a higher monthly premium than those who enrolled when they were first eligible. The exception to this rule is if you have a guaranteed issue right. Examples of guaranteed issue rights include: You move outside of your Medicare Advantage plan's service area.
What is Medicare Supplement?
Medicare supplement insurance policies help fill in the gaps left by Original Medicare health care insurance. For many people, Medicare Supplement, also known as Medigap, insurance helps them economically by paying some of the out-of-pocket costs associated with Original Medicare.
How many people does Medicare Supplement cover?
Keep in mind that, just like Medicare, Medicare Supplement plans are individual insurance policies. They only cover one person per plan. If you want coverage for your spouse, you must purchase a separate plan.
What percentage of Medicare supplement is paid?
After this is paid, your supplement policy pays your portion of the remaining cost. This is generally 20 percent. Some policies pay your deductibles The deductible is a set amount which you must pay before Medicare begins covering your health care costs.
How long does it take to get a Medigap plan?
When you turn 65 and enroll in Part B, you will have a 6-month Initial Enrollment Period to purchase any Medigap plan sold in your state. During this time, you have a “guaranteed issue right” to buy any plan available. They are required to accept you and cannot charge you more due to any pre-existing conditions.
How long does Medicare cover travel?
Each plan varies in what it covers, but all plans pay for Medicare Part A (hospital insurance) coinsurances for up to 365 days beyond the coverage that Medicare offers. Some of the plans cover a percentage of the cost for emergency health care while traveling abroad.
How old do you have to be to qualify for medicare?
To be eligible for Medicare, you must be at least 65 years old, a citizen of the United States or permanent legal resident for at least five consecutive years. Also, you, or your spouse, must have worked and paid federal taxes for at least ten years (or 40 quarters).
Does Medicare cover long term care?
Most plans do not cover long-term care, vision, dental, hearing care, or private nursing care. All Medicare Supplement insurance coverage comes with a monthly premium which you pay directly to your provider. How much you pay depends on which plan you have.